Abstract
Purpose of Review
Obesity constitutes a global crisis with profound implications on the incidence of metabolic dysfunction-associated steatotic liver disease (MASLD) and metabolic dysfunction-associated steatohepatitis (MASH). This paper aims to comprehensively explore the escalating obesity epidemic’s implications on liver transplantation, focusing on trends, clinical consequences, and therapeutic interventions to optimize outcomes for transplant candidates and recipients.
Recent Findings
Lifestyle modifications, including dietary and exercise programs, are crucial for pre- and post-transplant obesity managements. When lifestyle modifications prove insufficient, several FDA-approved pharmacologic options, such as orlistat, phentermine-topiramate, naltrexone-bupropion, liraglutide, semaglutide, and tirzepatide, can be considered. Bariatric surgical and endoscopic interventions are also viable options for select patients during all phases of liver transplantation with durable weight loss results.
Summary
Individualized therapeutic interventions should be crafted based on a comprehensive assessment, considering nutritional status, physical health, and the severity of liver disease. While lifestyle modification and pharmacologic interventions should be the initial course of action, their efficacy may be suboptimal. In such cases, consideration of bariatric intervention becomes imperative.


Similar content being viewed by others
Data availability
No datasets were generated or analysed during the current study.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Polyzos SA, Kountouras J, Mantzoros CS. Obesity and nonalcoholic fatty liver disease: From pathophysiology to therapeutics. Metabolism. 2019;92:82–97.
Wong VW, et al. Disease progression of non-alcoholic fatty liver disease: a prospective study with paired liver biopsies at 3 years. Gut. 2010;59(7):969–74.
Pierantonelli I, Svegliati-Baroni G. Nonalcoholic fatty liver disease: basic pathogenetic mechanisms in the progression from NAFLD to NASH. Transplantation. 2019;103(1):e1–13.
Younossi ZM, et al. Global epidemiology of nonalcoholic fatty liver disease—meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64(1):73–84.
Estes C, et al. Modeling the epidemic of nonalcoholic fatty liver disease demonstrates an exponential increase in burden of disease. Hepatology. 2018;67(1):123–33.
Watt KD, et al. Obesity management for the hepatologist - what to do, how to do it and why. Hepatology. 2023. This study offers a thorough examination of obesity management for individuals with liver disease, encompassing the pathophysiological impact of obesity on various liver conditions, a range of management strategies, and diverse treatment options.
Lewis A, et al. Organ donation in the US and Europe: the supply vs demand imbalance. Transplant Rev. 2021;35(2):100585.
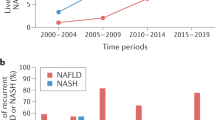
Cotter TG, Charlton M. Nonalcoholic steatohepatitis after liver transplantation. Liver Transpl. 2020;26(1):141–59.
Network O.P.a.T. Trends in SRTR deceased donor transplant and waitlist mortality rates. OPTN Metrics. 2022. https://insights.unos.org/OPTN-metrics/. Accessed 2 Nov 2023.
Schlansky B, et al. Higher mortality and survival benefit in obese patients awaiting liver transplantation. Transplantation. 2016;100(12):2648–55.
Kwong AJ, et al. OPTN/SRTR 2021 Annual data report: liver. Am J Transplant. 2023;23(2 Suppl 1):S178–263.
Berzigotti A, et al. Obesity is an independent risk factor for clinical decompensation in patients with cirrhosis. Hepatology. 2011;54(2):555–61.
Ayala R, et al. Obesity is an independent risk factor for pre-transplant portal vein thrombosis in liver recipients. BMC Gastroenterol. 2012;12:1–6.
Saunders D, et al. Systematic review: the association between obesity and hepatocellular carcinoma–epidemiological evidence. Aliment Pharmacol Ther. 2010;31(10):1051–63.
Gupta A, et al. Obesity is independently associated with increased risk of hepatocellular cancer–related mortality: a systematic review and meta-analysis. Am J Clin Oncol. 2018;41(9):874–81.
Segev DL, et al. Prolonged waiting times for liver transplantation in obese patients. Ann Surg. 2008;248(5):863–70.
Agopian VG, et al. Liver transplantation for nonalcoholic steatohepatitis: the new epidemic. Ann Surg. 2012;256(4):624–33.
Spengler EK, et al. Liver transplantation in the obese cirrhotic patient. Transplantation. 2017;101(10):2288–96.
Leonard J, et al. The impact of obesity on long-term outcomes in liver transplant recipients-results of the NIDDK liver transplant database. Am J Transplant. 2008;8(3):667–72.
Hakeem AR, et al. Increased morbidity in overweight and obese liver transplant recipients: a single-center experience of 1325 patients from the United Kingdom. Liver Transpl. 2013;19(5):551–62.
Saab S, et al. The impact of obesity on patient survival in liver transplant recipients: a meta-analysis. Liver Int. 2015;35(1):164–70.
Fussner LA, et al. Cardiovascular disease after liver transplantation: when, what, and who is at risk. Liver Transpl. 2015;21(7):889–96.
Alberti KGM, Zimmet P, Shaw J. The metabolic syndrome—a new worldwide definition. The Lancet. 2005;366(9491):1059–62.
Di Angelantonio E, et al. Body-mass index and all-cause mortality: individual-participant-data meta-analysis of 239 prospective studies in four continents. The Lancet. 2016;388(10046):776–86.
Gitto S, et al. Nonalcoholic steatohepatitis before and after liver transplant: keeping up with the times. Expert Rev Gastroenterol Hepatol. 2019;13(2):173–8.
Gitto S, et al. De-novo nonalcoholic steatohepatitis is associated with long-term increased mortality in liver transplant recipients. Eur J Gastroenterol Hepatol. 2018;30(7):766–73.
Bischoff SC, et al. Practical guideline on obesity care in patients with gastrointestinal and liver diseases - Joint ESPEN/UEG guideline. Clin Nutr. 2023;42(6):987–1024.
Lai JC, et al. Malnutrition, frailty, and sarcopenia in patients with cirrhosis: 2021 Practice Guidance by the American Association for the Study of Liver Diseases. Hepatology. 2021;74(3):1611–44. Official AASLD Guidance on the management of malnutrition, frailty and sarcopenia in patients with cirrhosis.
Vilar-Gomez E, et al. Weight loss through lifestyle modification significantly reduces features of nonalcoholic steatohepatitis. Gastroenterology. 2015;149(2):367-78e5. Landmark paper evaluating the importance of weight loss in improving biochemical and histological parameters in patients with metabolic dysfunction-associated steatohepatitis.
Everhart JE, et al. Weight-related effects on disease progression in the hepatitis C antiviral long-term treatment against cirrhosis trial. Gastroenterology. 2009;137(2):549–57.
Berzigotti A, et al. Effects of an intensive lifestyle intervention program on portal hypertension in patients with cirrhosis and obesity: The SportDiet study. Hepatology. 2017;65(4):1293–305.
Tandon P, Berzigotti A. Management of lifestyle factors in individuals with cirrhosis: a pragmatic review. Semin Liver Dis. 2020;40(1):20–8.
Salo J, et al. Impairment of renal function during moderate physical exercise in cirrhotic patients with ascites: relationship with the activity of neurohormonal systems. Hepatology. 1997;25(6):1338–42.
Haigh L, et al. The effectiveness and acceptability of Mediterranean diet and calorie restriction in non-alcoholic fatty liver disease (NAFLD): a systematic review and meta-analysis. Clin Nutr. 2022;41(9):1913–31.
Grosso G, et al. A comprehensive meta-analysis on evidence of Mediterranean diet and cardiovascular disease: are individual components equal? Crit Rev Food Sci Nutr. 2017;57(15):3218–32.
Turati F, et al. Mediterranean diet and hepatocellular carcinoma. J Hepatol. 2014;60(3):606–11.
Schwingshackl L, et al. Adherence to mediterranean diet and risk of cancer: an updated systematic review and metaanalysis. Nutrients. 2017;9(10):1063.
European Association for the Study of the Liver. Electronic address, e.e.e. and L. European association for the study of the, EASL clinical practice guidelines on nutrition in chronic liver disease. J Hepatol. 2019;70(1):172–193. Official EASL guidance on nutrition management in patients with chronic liver disease.
Stine JG, et al. Physical activity and nonalcoholic fatty liver disease: a roundtable statement from the American college of sports medicine. Med Sci Sports Exerc. 2023;55(9):1717–1726. Official guidance from the American College of Sports Medicine in collaboration with hepatologists on physical activity in patients with metabolic dysfunction-associated steatotic liver disease.
Chen HW, et al. Home-based physical activity and diet intervention to improve physical function in advanced liver disease: a randomized pilot trial. Dig Dis Sci. 2020;65(11):3350–9.
Zamora-Valdes D, et al. Long-term outcomes of patients undergoing simultaneous liver transplantation and sleeve gastrectomy. Hepatology. 2018;68(2):485–95. Key long-term data of the efficacy of simultaneous sleeve gastrectomy-liver transplantation in obese patients undergoing liver transplantation.
Fatourou EM, Tsochatzis EA. Management of metabolic syndrome and cardiovascular risk after liver transplantation. Lancet Gastroenterol Hepatol. 2019;4(9):731–41.
Watt KD, Charlton MR. Metabolic syndrome and liver transplantation: a review and guide to management. J Hepatol. 2010;53(1):199–206.
Spillman LN, et al. Nutritional intake after liver transplant: systematic review and meta-analysis. Nutrients. 2023;15(11):2487.
Krasnoff JB, et al. A randomized trial of exercise and dietary counseling after liver transplantation. Am J Transplant. 2006;6(8):1896–905. One of the first published randomized controlled trials evaluating the efficacy of an exercise and dietary counseling program in liver transplant recipients.
Hickman IJ, et al. Telehealth-delivered, cardioprotective diet and exercise program for liver transplant recipients: a randomized feasibility study. Transplant Direct. 2021;7(3):e667.
Armstrong MJ, et al. Liraglutide safety and efficacy in patients with non-alcoholic steatohepatitis (LEAN): a multicentre, double-blind, randomised, placebo-controlled phase 2 study. The Lancet. 2016;387(10019):679–90. Landmark randomized controlled trial evaluating liraglutide safety and efficacy in patients with metabolic dysfunction-associated steatotic liver disease.
Richardson SH, et al. Utility of glucagon-like peptide 1 receptor agonists as anti-obesity medications in liver transplant recipients. Liver Transpl. 2024;30(2):226–228.
Harrison SA, et al. Orlistat for overweight subjects with nonalcoholic steatohepatitis: a randomized, prospective trial. Hepatology. 2009;49(1):80–6.
Orlistat. In LiverTox: Clinical and research information on drug-induced liver injury. 2012. Bethesda (MD).
Wang H, et al. Efficacy of orlistat in non-alcoholic fatty liver disease: a systematic review and meta-analysis. Biomed Rep. 2018;9(1):90–6. Meta-analysis including all randomized controlled trials evaluating orlistat in patients with non-alcoholic fatty liver disease.
Cassiman D, et al. Orlistat treatment is safe in overweight and obese liver transplant recipients: a prospective, open label trial. Transpl Int. 2006;19(12):1000–5.
Allison DB, et al. Controlled-release phentermine/topiramate in severely obese adults: a randomized controlled trial (EQUIP). Obesity. 2012;20(2):330–42. One of the landmark trials evaluating the efficacy of phetermine-topiramate in promoting weight loss in obese patients.
Gadde KM, et al. Effects of low-dose, controlled-release, phentermine plus topiramate combination on weight and associated comorbidities in overweight and obese adults (CONQUER): a randomised, placebo-controlled, phase 3 trial. Lancet. 2011;377(9774):1341–52. One of the landmark trials evaluating the efficacy of phetermine-topiramate in promoting weight loss in obese patients.
Administration USFaD. Highlights of prescribing information - QSYMIA. 2012. https://www.accessdata.fda.gov/drugsatfda_docs/label/2012/022580s000lbl.pdf. Accessed 21 Nov 2023
Brown SA, Izzy M, Watt KD. Pharmacotherapy for weight loss in cirrhosis and liver transplantation: translating the data and underused potential. Hepatology. 2021;73(5):2051–62. Important review in Hepatology of the potential applications of pharmacotherapeutic agents approved by the FDA in addition to other frequently-encountered weight loss supplements in facilitating weight loss in obese patients with cirrhosis and liver transplant recipients.
Bajaj HS, et al. Extended-release naltrexone/bupropion and liver health: pooled, post hoc analysis from four randomized controlled trials. Diabetes Obes Metab. 2021;23(3):861–5.
Apovian CM, et al. A randomized, phase 3 trial of naltrexone SR/bupropion SR on weight and obesity-related risk factors (COR-II). Obesity (Silver Spring). 2013;21(5):935–43.
Lewis BR, et al. Pharmacokinetic interactions between cyclosporine and bupropion or methylphenidate. J Child Adolesc Psychopharmacol. 2001;11(2):193–8.
Lynch T, Neff AP. The effect of cytochrome P450 metabolism on drug response, interactions, and adverse effects. Am Fam Physician. 2007;76(3):391–6.
Wang J-Y, et al. GLP− 1 receptor agonists for the treatment of obesity: role as a promising approach. Front Endocrinol. 2023;14:1085799.
Samms RJ, Coghlan MP, Sloop KW. How may GIP enhance the therapeutic efficacy of GLP-1? Trends Endocrinol Metab. 2020;31(6):410–21.
Jerlhag E. GLP-1 signaling and alcohol-mediated behaviors; preclinical and clinical evidence. Neuropharmacology. 2018;136(Pt B):343–9.
Tsermpini EE, et al. Genetic variability of incretin receptors and alcohol dependence: a pilot study. Front Mol Neurosci. 2022;15:908948.
Wilding JP, et al. Once-weekly semaglutide in adults with overweight or obesity. New England Journal of Medicine. 2021;384(11):989–1002. Landmark STEP-1 trial revealing -14.9% weight loss in obese patients using once-weekly subcutaneous semaglutide.
Newsome PN, et al. A placebo-controlled trial of subcutaneous semaglutide in nonalcoholic steatohepatitis. N Engl J Med. 2021;384(12):1113–24. Phase II trial results of daily subcutaneous semaglutide in patients with metabolic dysfunction-associated steatotic liver.
Loomba R, et al. Semaglutide 2· 4 mg once weekly in patients with non-alcoholic steatohepatitis-related cirrhosis: a randomised, placebo-controlled phase 2 trial. Lancet Gastroenterol Hepatol. 2023;8(6):511–22. Important data on the safety of once-weekly, high-dose semaglutide use in patients with cirrhosis.
Jastreboff AM, et al. Tirzepatide once weekly for the treatment of obesity. N Engl J Med. 2022;387(3):205–16. Phase III trial results of once-weekly tirzepatide for the treatment of obesity showing up to 20.9% weight loss with the use of tirzepatide after 72 weeks.
Gastaldelli A, et al. Effect of tirzepatide versus insulin degludec on liver fat content and abdominal adipose tissue in people with type 2 diabetes (SURPASS-3 MRI): a substudy of the randomised, open-label, parallel-group, phase 3 SURPASS-3 trial. Lancet Diabetes Endocrinol. 2022;10(6):393–406.
Rubino D, et al. Effect of continued weekly subcutaneous semaglutide vs placebo on weight loss maintenance in adults with overweight or obesity: the STEP 4 randomized clinical trial. JAMA. 2021;325(14):1414–25.
Courcoulas AP, et al. Long-term outcomes of bariatric surgery: a National Institutes of Health Symposium. JAMA Surg. 2014;149(12):1323–9.
Eisenberg D, et al. 2022 American Society of Metabolic and Bariatric Surgery (ASMBS) and International Federation for the Surgery of Obesity and Metabolic Disorders (IFSO) Indications for Metabolic and Bariatric Surgery. Obes Surg. 2023;33(1):3–14.
Pestana L, et al. Bariatric surgery in patients with cirrhosis with and without portal hypertension: a single-center experience. in Mayo Clinic Proceedings. 2015. Elsevier.
Diwan TS, et al. Obesity, transplantation, and bariatric surgery: an evolving solution for a growing epidemic. Am J Transplant. 2020;20(8):2143–55.
McCarty TR, Thompson CC. The current state of bariatric endoscopy. Dig Endosc. 2021;33(3):321–34.
Sullivan S, Edmundowicz SA, Thompson CC. Endoscopic bariatric and metabolic therapies: new and emerging technologies. Gastroenterology. 2017;152(7):1791–801.
Kumar N, et al. The influence of the Orbera intragastric balloon filling volumes on weight loss, tolerability, and adverse events: a systematic review and meta-analysis. Obes Surg. 2017;27:2272–8.
Jirapinyo P, et al. Effect of endoscopic bariatric and metabolic therapies on nonalcoholic fatty liver disease: a systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2022;20(3):511-524.e1.
Patton H, Heimbach J, McCullough A. AGA clinical practice update on bariatric surgery in cirrhosis: expert review. Clin Gastroenterol Hepatol. 2021;19(3):436–45. Clinical practice guidelines issued by the American Gastroenterological Association that address frequently asked questions concerning the management of obesity in patients with cirrhosis.
Peterli R, et al. Effect of laparoscopic sleeve gastrectomy vs laparoscopic Roux-en-Y gastric bypass on weight loss in patients with morbid obesity: the SM-BOSS randomized clinical trial. JAMA. 2018;319(3):255–65.
Slomski A. Bariatric Surgery Approaches Reduce Fatty Liver Disease. JAMA. 2022;327(8):710–710.
Kumar SB, et al. Is laparoscopic sleeve gastrectomy safer than laparoscopic gastric bypass? A comparison of 30-day complications using the MBSAQIP data registry. Surg Obes Relat Dis. 2018;14(3):264–9.
Saiman Y, Serper M. Frailty and sarcopenia in patients pre- and post-liver transplant. Clin Liver Dis. 2021;25(1):35–51.
Thomas IA, et al. Roux-en-Y gastric bypass is an effective bridge to kidney transplantation: Results from a single center. Clin Transplant. 2018;32(5):e13232.
Lee Y, et al. Bariatric surgery before, during, and after liver transplantation: a systematic review and meta-analysis. Surg Obes Relat Dis. 2020;16(9):1336–47.
Quezada N, et al. Bariatric surgery in cirrhotic patients: a matched case-control study. Obes Surg. 2020;30(12):4724–31.
Shimizu H, et al. Bariatric surgery in patients with liver cirrhosis. Surg Obes Relat Dis. 2013;9(1):1–6.
Miñambres I, et al. Outcomes of bariatric surgery in patients with cirrhosis. Obes Surg. 2019;29(2):585–92.
Sharpton SR, et al. Sleeve gastrectomy prior to liver transplantation is superior to medical weight loss in reducing posttransplant metabolic complications. Am J Transplant. 2021;21(10):3324–32.
Lee Y, et al. Complete resolution of nonalcoholic fatty liver disease after bariatric surgery: a systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2019;17(6):1040-1060.e11.
Bonner K, Heimbach JK. Obesity management in the liver transplant recipient: the role of bariatric surgery. Curr Opin Organ Transplant. 2018;23(2):244–9.
Younus H, et al. Bariatric surgery in cirrhotic patients: is it safe? Obes Surg. 2020;30(4):1241–8.
Jan A, Narwaria M, Mahawar KK. A systematic review of bariatric surgery in patients with liver cirrhosis. Obes Surg. 2015;25(8):1518–26.
Mosko JD, Nguyen GC. Increased perioperative mortality following bariatric surgery among patients with cirrhosis. Clin Gastroenterol Hepatol. 2011;9(10):897–901.
Mumtaz K, et al. Bariatric surgery in patients with cirrhosis: careful patient and surgery-type selection is key to improving outcomes. Obes Surg. 2020;30:3444–52.
Zamora-Valdes D, et al. Long-term outcomes of patients undergoing simultaneous liver transplantation and sleeve gastrectomy. Hepatology. 2018;68(2):485–95.
Nesher E, et al. Simultaneous liver transplantation and sleeve gastrectomy: prohibitive combination or a necessity? Obes Surg. 2017;27(5):1387–90.
Khoraki J, et al. Feasibility and outcomes of laparoscopic sleeve gastrectomy after solid organ transplantation. Surg Obes Relat Dis. 2016;12(1):75–83.
Lin MY, et al. Safety and feasibility of sleeve gastrectomy in morbidly obese patients following liver transplantation. Surg Endosc. 2013;27(1):81–5.
Tsamalaidze L, et al. Laparoscopic sleeve gastrectomy for morbid obesity in patients after orthotopic liver transplant: a matched case-control study. Obes Surg. 2018;28(2):444–50.
Morris MC, et al. Delayed sleeve gastrectomy following liver transplantation: a 5-year experience. Liver Transpl. 2019;25(11):1673–81.
Lopez-Lopez V, et al. Are we ready for bariatric surgery in a liver transplant program? A meta-analysis Obesity Surgery. 2021;31(3):1214–22.
Author information
Authors and Affiliations
Contributions
J.L. and M.Q.K. wrote the main manuscript text and prepared the figures and tables. K.D.W. and T.S.D. provided feedback and edits. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lam, J., Khan, M.Q., Watt, K.D. et al. Optimal Management of Obesity in Transplant Candidates and Recipients. Curr Transpl Rep (2024). https://doi.org/10.1007/s40472-024-00434-8
Accepted:
Published:
DOI: https://doi.org/10.1007/s40472-024-00434-8