Abstract
Background
There have been no studies examining the association between antihypertensive medications and progression of diastolic dysfunction. The purpose of this study is to determine whether there is an association between class of antihypertensive medication and diastolic dysfunction progression in an African American population.
Methods
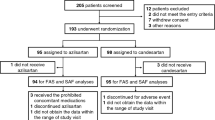
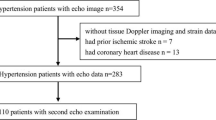
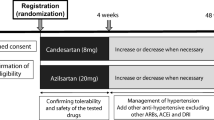
A retrospective cohort study of African American patients with at least two echocardiograms demonstrating diastolic dysfunction drawn from an echocardiogram database at an academic medical center. The main outcome measures were change in diastolic function grade as a function of time and association with hypertension medication classification.
Results
There were 96 African American patients in the database with 2 or more echocardiograms demonstrating diastolic dysfunction; representing 302 echocardiograms. The mean time between echocardiograms was 2.6 years. The mean age was 64.2 (±10.1) years, 78 % were women, and mean BMI 31.2 (±7.4) kg/m2. The majority of subjects had Grade I diastolic dysfunction at their initial examination [N = 87 (90.6 %)]. Approximately 22.9 % (n = 22) of the study cohort demonstrated diastolic dysfunction progression. In multivariate analysis use of calcium channel blockers (CCB) was protective against diastolic dysfunction progression (OR for CCB users vs. non-users 0.28, 95 % confidence interval, 0.09–0.90, p < 0.05).
Conclusions
These findings suggest that use of calcium channel blockers may have a protective effect against progression of diastolic dysfunction among African American patients. Further studies are required to confirm these findings and identify specific factors that can mediate disease progression among African American individuals with hypertension, who face substantial risk of complications such as diastolic heart failure.
Similar content being viewed by others
References
Ferdinand K, Armani A. The management of hypertension in African Americans. Crit Pathw Cardiol. 2007;6:67–71.
Garg N, Senthilkumar A, Nusair M, et al. Heart Failure with a normal left ventricular ejection fraction: epidemiology, pathophysiology, diagnosis and management. Am J Med Sci. 2013;346:129–36.
Shah S. Heart failure with preserved ejection fraction in African Americans. Ethn Dis. 2012;22:432–8.
Aljaroudi W, Thomas J, Rodriguez L. et al. Prognostic Value of diastolic dysfunction: a state of the art review. Cardiol Rev. 2014;22:79–90.
Von Lueder T, Krum H. RAAS inhibitors and cardiovascular protection in large scale trials. Cardiovasc Drugs Ther. 2013;27:171–9.
James P, Oparil S, Carter B, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC-8). JAMA. 2014;311:507–20.
Sussman J, Vijan S, Hayward R. Using benefit-based tailored treatment to improve the use of antihypertensive medications. Circulation. 2013;128:2309–17.
Prendergast H, Dudley S, Kane J, et al. Progression of left ventricular diastolic dysfunction in ethnic minorities. High Blood Press Cardiovasc Prevention. 2013. [Epub ahead of print].
Recommendations for Chamber Quantification: A Report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, Developed in Conjunction with the European Association of Echocardiography, a Branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005;18:1440–63.
Flack J, Sica D, Bakris G, et al. Management of high blood pressure in blacks: an update of the international society on hypertension in blacks consensus statement. Hypertension. 2010;56:780–800.
Ozkor M, Rahman A, Murrow J, et al. Differences in vascular nitric oxide and endothelium-derived hyperpolarizing factor bioavailability in blacks and whites. Arterioscler Thromb Vasc Biol. 2014;34:1320-27.
Ding Y, Vaziri N. Nifedipine and diltiazem but not verapamil up-regulate endothelial nitric-oxide synthase expression. JPET. 2000;292:606–9.
Ding Y, Vaziri N. Calcium channel blockade enhances nitric oxide synthase expression by cultured endothelial cells. Hypertension. 1998;32:718–23.
Tabrizchi R. Amlodipine and endothelial nitric oxide synthase activity. Cardiovasc Res. 2003;53:807–9.
Brener S, Ivanc T, Poloszczuk R, et al. Antihypertensive therapy and regression of coronary artery disease: insights from the Comparison of Amlodipine versus Enalapril to Limit Occurrences of Thrombosis(CAMELOT) and Norvasc for Regression of Manifest Atherosclerotic Lesions by Intravascular Sonographic Evaluation (NORMALISE) trials. Am Heart J. 2006;15:1059–63.
Wood P, Piran S, Liu P. Diastolic heart failure: progress, treatment challenges, and prevention. Can J Cardiol. 2011;27:302–10.
Gradman A, Basile J, Carter B, et al. Combination therapy in hypertension. JASH. 2010;4:90–8.
Bruasoulis A, Agarwal V, Tousoulis D, et al. Effects of antihypertensive treatment in patients over 65 years of age: a meta-analysis of randomized controlled studies. Heart. 2014;100:317–23.
Joffe S, Phillips R. Treating hypertension in patients with left ventricular dysfunction: hitting the fairway and avoiding the rough. Curr Heart Fail Rep. 2013;10:157–64.
Glezeva N, Baugh J. Role of inflammation in the pathogenesis of heart failure with preserved ejection fraction and its potential as a therapeutic target. Heart Fail Rev. 2013. Sept 5. [Epub ahead of print].
Glezeva N, Baugh J. Role of inflammation in the pathogenesis of heart failure with preserved ejection fraction and its potential as a therapeutic target. Heart Fail Rev. 2013. Sept 5. [Epub ahead of print].
Acknowledgments
The project described was supported by the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant UL1TR000050. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Prendergast, H.M., Dudley, S., Brown, M. et al. Antihypertensive Medications and Diastolic Dysfunction Progression in an African American Population. High Blood Press Cardiovasc Prev 21, 269–274 (2014). https://doi.org/10.1007/s40292-014-0064-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40292-014-0064-1