Abstract
Background
Observational healthcare data offer the potential to enable identification of risks of medical products, and the medical literature is replete with analyses that aim to accomplish this objective. A number of established analytic methods dominate the literature but their operating characteristics in real-world settings remain unknown.
Objectives
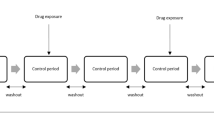
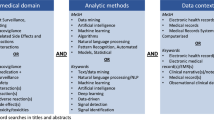
To compare the performance of seven methods (new user cohort, case control, self-controlled case series, self-controlled cohort, disproportionality analysis, temporal pattern discovery, and longitudinal gamma poisson shrinker) as tools for risk identification in observational healthcare data.
Research Design
The experiment applied each method to 399 drug-outcome scenarios (165 positive controls and 234 negative controls across 4 health outcomes of interest) in 5 real observational databases (4 administrative claims and 1 electronic health record).
Measures
Method performance was evaluated through Area Under the receiver operator characteristics Curve (AUC), bias, mean square error, and confidence interval coverage probability.
Results
Multiple methods offer strong predictive accuracy, with AUC > 0.70 achievable for all outcomes and databases with more than one analytical approach. Self-controlled methods (self-controlled case series, temporal pattern discovery, self-controlled cohort) had higher predictive accuracy than cohort and case–control methods across all databases and outcomes. Methods differed in the expected value and variance of the error distribution. All methods had lower coverage probability than the expected nominal properties.
Conclusions
Observational healthcare data can inform risk identification of medical product effects on acute liver injury, acute myocardial infarction, acute renal failure and gastrointestinal bleeding. However, effect estimates from all methods require calibration to address inconsistency in method operating characteristics. Further empirical evaluation is required to gauge the generalizability of these findings to other databases and outcomes.


Similar content being viewed by others
References
Atkins D, Best D, Briss PA, Eccles M, Falck-Ytter Y, Flottorp S, et al. Grading quality of evidence and strength of recommendations. BMJ. 2004;328(7454):1490.
Berlin JA, Glasser SC, Ellenberg SS. Adverse event detection in drug development: recommendations and obligations beyond phase 3. Am J Public Health. 2008;98(8):1366–71.
Waller PC, Evans SJ. A model for the future conduct of pharmacovigilance. Pharmacoepidemiol Drug Saf. 2003;12(1):17–29.
Ioannidis JP. Why most published research findings are false. PLoS Med. 2005;2(8):e124.
Food and Drug Administration Amendments Act of 2007. p. Public Law 110-85, 21 STAT. 823 (2007).
FDA. The Sentinel Initiative: A National Strategy for Monitoring Medical Product Safety. May 2008 [cited 2012 September 15]. http://www.fda.gov/Safety/FDAsSentinelInitiative/ucm089474.htm.
FDA Drug Safety Communication: Update on the risk for serious bleeding events with the anticoagulant Pradaxa (dabigatran). November 2, 2012 [cited 2012 December 1]. http://www.fda.gov/Drugs/DrugSafety/ucm326580.htm.
DuMouchel B, Ryan PB, Schuemie MJ, Madigan D. Evaluation of disproportionality safety signaling applied to health care databases. Drug Saf (in this supplement issue).doi:10.1007/s40264-013-0106-y.
Madigan D, Schuemie MJ, Ryan PB. Empirical performance of the case–control method: lessons for developing a risk identification and analysis system. Drug Saf (in this supplement issue). doi:10.1007/s40264-013-0105-z.
Norén GN, Bergvall T, Ryan PB, Juhlin K, Schuemie MJ, Madigna D. Empirical performance of the calibrated self-controlled cohort analysis within Temporal Pattern Discovery: lessons for developing a risk identification and analysis system. Drug Saf (in this supplement issue). doi:10.1007/s40264-013-0095-x.
Ryan PB, Schuemie MJ, Gruber S, Zorych I, Madigan D. Empirical performance of a new user cohort method: lessons for developing a risk identification and analysis system. Drug Saf (in this supplement issue). doi:10.1007/s40264-013-0099-6.
Ryan PB, Schuemie MJ, Madigan D. Empirical performance of a self-controlled cohort method: lessons for developing a risk identification and analysis system. Drug Saf (in this supplement issue). doi:10.1007/s40264-013-0101-3.
Schuemie MJ, Madigan D, Ryan PB. Empirical performance of Longitudinal Gamma Poisson Shrinker (LGPS) and Longitudinal Evaluation of Observational Profiles of Adverse events Related to Drugs (LEOPARD): lessons for developing a risk identification and analysis system. Drug Saf (in this supplement issue). doi:10.1007/s40264-013-0107-x.
Suchard MA, Zorych I, Simpson SE, Schuemie MJ, Ryan PB, Madigan D. Empirical performance of the self-controlled case series design: lessons for developing a risk identification and analysis system. Drug Saf (in this supplement issue).doi:10.1007/s40264-013-0100-4.
Schuemie MJ, Ryan PB, DuMouchel W, Suchard MA, Madigan D. Interpreting observational studies: why empirical calibration is needed to correct p-values. Stat Med. 2013. doi:10.1002/sim.5925.
Ryan PB, Schuemie MJ, Welebob E, Duke J, Valentine S, Hartzema AG. Defining a reference set to support methodological research in drug safety. Drug Saf (in this supplement issue). doi:10.1007/s40264-013-0097-8.
Greenland S. Confounding and exposure trends in case-crossover and case-time-control designs. Epidemiology. 1996;7(3):231–9.
Maclure M. The case-crossover design: a method for studying transient effects on the risk of acute events. Am J Epidemiol. 1991;133(2):144–53.
Maclure M, Fireman B, Nelson JC, Hua W, Shoaibi A, Paredes A, et al. When should case-only designs be used for safety monitoring of medical products? Pharmacoepidemiol Drug Saf. 2012;21 Suppl 1:50–61.
Gagne JJ, Fireman B, Ryan PB, Maclure M, Gerhard T, Toh S, et al. Design considerations in an active medical product safety monitoring system. Pharmacoepidemiol Drug Saf. 2012;21(Suppl 1):32–40.
Bombardier C, Laine L, Reicin A, Shapiro D, Burgos-Vargas R, Davis B, et al. Comparison of upper gastrointestinal toxicity of rofecoxib and naproxen in patients with rheumatoid arthritis. VIGOR Study Group. N Engl J Med. 2000;343(21):1520–8 (2 p following 8).
Bresalier RS, Sandler RS, Quan H, Bolognese JA, Oxenius B, Horgan K, et al. Cardiovascular events associated with rofecoxib in a colorectal adenoma chemoprevention trial. N Engl J Med. 2005;352(11):1092–102.
Nissen SE, Wolski K. Effect of rosiglitazone on the risk of myocardial infarction and death from cardiovascular causes. N Engl J Med. 2007;356(24):2457–71.
Cunnington M, Webb D, Qizilbash N, Blum D, Mander A, Funk MJ, et al. Risk of ischaemic cardiovascular events from selective cyclooxygenase-2 inhibitors in osteoarthritis. Pharmacoepidemiol Drug Saf. 2008;17(6):601–8.
Graham DJ, Campen D, Hui R, Spence M, Cheetham C, Levy G, et al. Risk of acute myocardial infarction and sudden cardiac death in patients treated with cyclo-oxygenase 2 selective and non-selective non-steroidal anti-inflammatory drugs: nested case–control study. Lancet. 2005;365(9458):475–81.
Brown JS, Kulldorff M, Chan KA, Davis RL, Graham D, Pettus PT, et al. Early detection of adverse drug events within population-based health networks: application of sequential testing methods. Pharmacoepidemiol Drug Saf. 2007;16(12):1275–84.
Brownstein JS, Sordo M, Kohane IS, Mandl KD. The tell-tale heart: population-based surveillance reveals an association of rofecoxib and celecoxib with myocardial infarction. PLoS ONE. 2007;2(9):e840.
Brownstein JS, Murphy SN, Goldfine AB, Grant RW, Sordo M, Gainer V, et al. Rapid identification of myocardial infarction risk associated with diabetes medications using electronic medical records. Diabetes Care. 2010;33(3):526–31.
Graham DJ, Ouellet-Hellstrom R, MaCurdy TE, Ali F, Sholley C, Worrall C, et al. Risk of acute myocardial infarction, stroke, heart failure, and death in elderly Medicare patients treated with rosiglitazone or pioglitazone. JAMA. 2010;304(4):411–8.
Ryan PB, Madigan D, Stang PE, Marc Overhage J, Racoosin JA, Hartzema AG. Empirical assessment of methods for risk identification in healthcare data: results from the experiments of the Observational Medical Outcomes Partnership. Stat Med. 2012;31(30):4401–15.
Schuemie MJ, Coloma PM, Straatman H, Herings RM, Trifirò G, Matthews JN, et al. Using electronic health care records for drug safety signal detection: a comparative evaluation of statistical methods. Med Care. 2012.
Coloma PM, Avillach P, Salvo F, Schuemie MJ, Ferrajolo C, Pariente A, et al. A reference standard for evaluation of methods for drug safety signal detection using electronic healthcare record databases. Drug Saf. 2013;36(1):13–23.
Glanz JM, McClure DL, Xu S, Hambidge SJ, Lee M, Kolczak MS, et al. Four different study designs to evaluate vaccine safety were equally validated with contrasting limitations. J Clin Epidemiol. 2006;59(8):808–18.
Nicholas JM, Grieve AP, Gulliford MC. Within-person study designs had lower precision and greater susceptibility to bias because of trends in exposure than cohort and nested case–control designs. J Clin Epidemiol. 2012;65(4):384–93.
Ramsay EN, Pratt NL, Ryan P, Roughead EE. Proton pump inhibitors and the risk of pneumonia: a comparison of cohort and self-controlled case series designs. BMC Med Res Methodol. 2013;13(1):82.
Hubbard R, Farrington P, Smith C, Smeeth L, Tattersfield A. Exposure to tricyclic and selective serotonin reuptake inhibitor antidepressants and the risk of hip fracture. Am J Epidemiol. 2003;158(1):77–84.
Tata LJ, Fortun PJ, Hubbard RB, Smeeth L, Hawkey CJ, Smith CJ, et al. Does concurrent prescription of selective serotonin reuptake inhibitors and non-steroidal anti-inflammatory drugs substantially increase the risk of upper gastrointestinal bleeding? Aliment Pharmacol Ther. 2005;22(3):175–81.
Schneeweiss S. A basic study design for expedited safety signal evaluation based on electronic healthcare data. Pharmacoepidemiol Drug Saf. 2010;19(8):858–68.
Pearce N. Classification of epidemiological study designs. Int J Epidemiol. 2012;41(2):393–7.
Trifirò G, Pariente A, Coloma PM, Kors JA, Polimeni G, Miremont-Salame G, et al. Data mining on electronic health record databases for signal detection in pharmacovigilance: which events to monitor? Pharmacoepidemiol Drug Saf. 2009;18(12):1176–84.
Tisdale J, Miller D. Drug-induced diseases: prevention, detection, and management. 2nd ed. American Society of Health-System Pharmacists; 2010.
Acknowledgments
The Observational Medical Outcomes Partnership is funded by the Foundation for the National Institutes of Health (FNIH) through generous contributions from the following: Abbott, Amgen Inc., AstraZeneca, Bayer Healthcare Pharmaceuticals, Inc., Biogen Idec, Bristol-Myers Squibb, Eli Lilly & Company, GlaxoSmithKline, Janssen Research and Development, Lundbeck, Inc., Merck & Co., Inc., Novartis Pharmaceuticals Corporation, Pfizer Inc, Pharmaceutical Research Manufacturers of America (PhRMA), Roche, Sanofi-aventis, Schering-Plough Corporation, and Takeda. Drs. Ryan, Stang and Schuemie are employees of Janssen Research and Development. Dr. Schuemie received a fellowship from the Office of Medical Policy, Center for Drug Evaluation and Research, Food and Drug Administration. Drs. Schuemie, Suchard, Madigan, and Hartzema have received a grant previously from FNIH. Dr. DuMouchel is an employee of Oracle Health Sciences. Dr. Overhage is an employee of Siemens. Christian Reich is an employee of Astra-Zeneca.
This article was published in a supplement sponsored by the Foundation for the National Institutes of Health (FNIH). The supplement was guest edited by Stephen J.W. Evans. It was peer reviewed by Olaf H. Klungel who received a small honorarium to cover out-of-pocket expenses. S.J.W.E has received travel funding from the FNIH to travel to the OMOP symposium and received a fee from FNIH for the review of a protocol for OMOP. O.H.K has received funding for the IMI–PROTECT project from the Innovative Medicines Initiative Joint Undertaking (http://www.imi.europa.eu) under Grant Agreement no 115004, resources of which are composed of financial contribution from the European Union’s Seventh Framework Programme (FP7/2007–2013) and EFPIA companies’ in kind contribution.
Author information
Authors and Affiliations
Corresponding author
Additional information
The OMOP research used data from Truven Health Analytics (formerly the Health Business of Thomson Reuters), and includes MarketScan® Research Databases, represented with MarketScan Lab Supplemental (MSLR, 1.2 m persons), MarketScan Medicare Supplemental Beneficiaries (MDCR, 4.6 m persons), MarketScan Multi-State Medicaid (MDCD, 10.8 m persons), MarketScan Commercial Claims and Encounters (CCAE, 46.5 m persons). Data also provided by Quintiles® Practice Research Database (formerly General Electric’s Electronic Health Record, 11.2 m persons) database. GE is an electronic health record database while the other four databases contain administrative claims data.
Rights and permissions
About this article
Cite this article
Ryan, P.B., Stang, P.E., Overhage, J.M. et al. A Comparison of the Empirical Performance of Methods for a Risk Identification System. Drug Saf 36 (Suppl 1), 143–158 (2013). https://doi.org/10.1007/s40264-013-0108-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40264-013-0108-9