Abstract
Background
CER-001 comprises recombinant human apolipoprotein A-I complexed with phospholipids that mimics natural, nascent, pre-β high-density lipoprotein (HDL). We present animal model data showing dose-dependent increases in cholesterol efflux with CER-001 and its subsequent elimination by reverse lipid transport, together with inhibition of atherosclerotic plaque progression. We report the first phase I study results with CER-001 in humans, starting at 0.25 mg/kg, which is 1/80th of the safe dose (20 mg/kg) established in 4-week multiple-dose animal studies dosed every second day.
Methods
Healthy volunteers, 18–55 years old with a low-density lipoprotein-cholesterol:HDL-cholesterol ratio greater than 3.0, received single intravenous escalating doses of CER-001 (0.25–45.0 mg/kg) and placebo in a double-blind randomised cross-over fashion. Subjects were followed up for 3 weeks post-dose. Assessments included adverse event monitoring, blood sampling, and clinical laboratory measurements.
Results
Thirty-two subjects were enrolled. All CER-001 doses (0.25–45 mg/kg) were safe and well tolerated, with an adverse event profile similar to placebo. Effects on clinical chemistry, haematology and coagulation parameters were comparable to placebo. No adverse effects of CER-001 on electrocardiograms were observed. No antibodies to apolipoprotein A-I were detected following single-dose administration of CER-001. Plasma apolipoprotein A-I levels increased in a dose-related manner and returned to baseline by 24 h post-dose for doses up to 10 mg/kg but remained in circulation for >72 h post-dose for doses >10 mg/kg. CER-001 caused elevations in plasma cholesterol and total and unesterified cholesterol in the HDL fraction. Mobilisation of unesterified cholesterol in the HDL fraction was seen with CER-001 at doses as low as 2 mg/kg.
Conclusion
CER-001 is well tolerated when administered to humans as single doses up to 45 mg/kg and mobilises and eliminates cholesterol via reverse lipid transport.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
CER-001 is well tolerated when administered to humans as single doses up to 45 mg/kg. |
CER-001 mobilises cholesterol and increases its elimination via reverse lipid transport. |
CER-001 inhibits atherosclerotic plaque progression, providing considerable optimism that it may address the residual risk of cardiovascular events that remains after maximum clinical benefit has been achieved using low-density lipoprotein-cholesterol-lowering therapies. |
1 Introduction
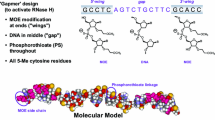
CER-001 is a negatively charged, engineered, pre-β high-density lipoprotein (HDL) particle that contains the natural HDL protein, human recombinant apolipoprotein A-I (ApoA-I) together with natural phospholipids, combined into a single small discoidal particle. As such, CER-001 mimics the structure, the charge and function of nascent HDL. The phospholipid species used in CER-001 were selected for their ability to form a discoidal complex with a strong affinity for cholesterol [1, 2], a negative charge to slow clearance by the kidney [3] and to trigger recognition by the liver [4], together with the high stability of the complexes in the circulation.
CER-001 possesses all the structural and functional biological properties of nascent HDL, including the ability to penetrate atherosclerotic plaque, to collect cholesterol, transport it from the plaque and then be recognised by HDL receptors in the liver where cholesterol is eliminated. In low-density lipoprotein (LDL)-deficient mice fed a high-cholesterol diet, CER-001 has been shown to stimulate reverse lipid transport and atherosclerosis regression [5]. In a recent study using radiolabelled CER-001, Zheng and co-workers [6] demonstrated that CER-001 enhances plasma cholesterol efflux capacity and accesses advanced atherosclerotic plaques in patients with atherosclerotic carotid artery disease.
CER-001 is an intravenous therapy currently in development for the secondary prevention of cardiovascular events after an acute coronary syndrome [7, 8], familial hypercholesterolaemia [9] and for rare severe genetic deficiencies in HDL particle synthesis/maturation (familial primary hypoalphalipoproteinaemia) [10], for which two separate orphan designations have been granted by the European Medicines Agency, specifically apolipoprotein A-I (ApoA-I) deficiency and ATP-binding cassette transporter 1 (ABCA1) deficiency.
While clinical evidence on the effectiveness of CER-001 and similar therapies continues to increase, very limited data are available showing the key information used in the dose selection process. Here, we present key in vitro/in vivo findings and steps in the development of CER-001, focusing specifically on dose selection data, together with the first phase I clinical study results with the product in humans.
2 Methods
2.1 Key Preclinical Pharmacology Studies
2.1.1 Cholesterol Mobilisation
In a fasted New Zealand White rabbit, cholesterol mobilisation model, CER-001 or phosphate/sucrose buffered saline vehicle control was infused intravenously at a rate of 1 mL/min into fasted animals in an infusion volume of 5 mL/kg; the final doses of CER-001 were 2.5, 5, 10 and 20 mg/kg, with three animals per dose group. Venous blood was collected via a permanent catheter that was placed the day before the experiment in the marginal vein of the ear and reached the jugular vein lumen. Blood samples were collected at baseline, then at 12 min (end of infusion), 30 min, 45 min, 1, 2, 4, 6, 8, 30 and 34 h after initiating the infusion. Plasma lipoprotein levels were determined by high-performance liquid chromatography (HPLC) size exclusion fractionation with inline unesterified and total cholesterol detection (see Online Supplementary Material) [11]. The area under each of the main HPLC peaks corresponding to lipoproteins with the sizes of very low-density lipoprotein (VLDL), LDL and HDL was integrated. The percent of the total unesterified and total cholesterol area in each lipoprotein fraction was multiplied by the total plasma cholesterol or unesterified cholesterol to determine the level of cholesterol in each lipoprotein fraction. Cholesterol ester levels in each fraction were determined by subtracting the unesterified cholesterol from the total cholesterol in each fraction. In this model, increases in plasma or HDL-cholesterol levels are indicative of tissue cholesterol mobilisation by HDL. Data are presented as mean values of each timepoint in each treatment group; results at each timepoint are also expressed as the change from baseline by subtracting the baseline value from the value at that particular timepoint.
2.1.2 Attenuated Inhibition of Atherosclerotic Plaque Progression
There is evidence in the literature for a trend towards decreased efficacy with higher doses of different HDL mimetics (i.e. ETC-216, CER-001) in clinical trials [7, 12]. The dose–response effect of CER-001 and HDL3 was assessed in vivo on plaque formation in the ligatured carotids of apolipoprotein E (ApoE)−/− mice fed a high-cholesterol diet. The left carotid was ligated in anaesthetised ApoE−/− mice and groups of mice (n = 12) were subsequently fed with a high-cholesterol diet and treated (retro-orbital injection) every second day with different dose levels of CER-001 (2–50 mg/kg) or HDL3 (5–50 mg/kg) for 2 weeks. After eight infusions, mice were anaesthetised [intraperitoneal injection of a mixture of ketamine (100 mg/kg) and xylazine (10 mg/kg)] and the carotids were excised and stored at −80 °C until analysed. For each group, the lipids were extracted from each excised carotid and the cholesterol level determined by HPLC (see Online Supplementary Material). Data are presented as mean (±standard error of the mean) values of each treatment group by dose and compared with the control group.
2.2 Phase I Single Rising-Dose Clinical Study
This was a randomised, double-blind, placebo-controlled, cross-over, single rising-dose study design in healthy male and female volunteers, 18–55 years of age, with an LDL-cholesterol:HDL-cholesterol ratio >3.0. The objectives of the study were to assess the safety, tolerability, pharmacokinetics and pharmacodynamics of CER-001 when administered as a single intravenous dose in healthy dyslipidaemic volunteers.
Subjects were treated in four cohorts of eight, with each subject receiving a single dose of CER-001 and a single dose of placebo in a randomised cross-over fashion. Escalating doses of 0.25, 0.75, 2.0, 5.0, 10.0, 15.0, 30.0 and 45.0 mg/kg were studied. Study medication was infused intravenously over 1 h for doses up to 30 mg/kg and over 2 h for doses of 45 mg/kg. The eight subjects included at each dose level were treated as follows: two subjects (one active/one placebo) were dosed on the first day; after 24 h, two additional subjects (one active/one placebo) were dosed; and after an additional 24 h, the remaining four subjects in the cohort (two active/two placebo) were dosed. During each study period, subjects remained in the clinic for 72 h following dose administration on day 1 and then returned to the clinic for outpatient follow-up visits on days 8, 15 and 22. Dose escalation for each dose level above 0.25 mg/kg was made after careful review of all available safety, tolerance and pharmacokinetic/pharmacodynamic data for previous doses and in consultation with the investigator.
Study assessments included adverse event (AE) monitoring, routine clinical chemistry, haematology and coagulation measurements, electrocardiograms, physical examination and monitoring of vital signs. For the pharmacokinetic assessment, clinical chemistry, ApoA-I levels were measured using an automated turbidimetric immunoassay method (Pentra 400 autoanalyzer, manufactured by Horiba ABX SAS, Montpellier, France). Pharmacodynamic effect was determined by serial determinations of lipoprotein profiles (LDL, HDL and VLDL fractions) in total and unesterified cholesterol using a validated HPLC method.
3 Results
3.1 Key Preclinical Pharmacology Studies
3.1.1 Cholesterol Mobilisation
In this rabbit cholesterol mobilisation model, intravenous administration of CER-001 at doses of 2.5, 5, 10 and 20 mg/kg increased plasma phospholipids and ApoA-I, and mobilised cholesterol in a dose-dependent manner, with effects being observed at the 2.5-mg/kg dose (Fig. 1). The majority of the cholesterol increase was in the form of unesterified cholesterol (Fig. 1b), although a CER-001-dependent increase in plasma cholesterol ester was observed (Fig. 1c). Plasma phospholipids and cholesterol returned to baseline levels within 30–34 h of treatment initiation (Table 1) [animals had free access to food 8 h after administration of CER-001]. The presence of human ApoA-I in the HDL fraction after HPLC fractionation suggests that the cholesterol-loaded CER-001 complexes remain stable (i.e. in the range of the HDL size) throughout the cholesterol mobilisation process in rabbits. It is worth noting that similar dose-dependent increases in cholesterol mobilisation were also observed in rat and primate models (data not shown).
Increase in mean plasma a total cholesterol, b unesterified (free) cholesterol and c esterified cholesterol following intravenous infusion of CER-001 into fasted rabbits. CER-001 doses: 0 (squares), 2.5 (triangles), 5 (inverted triangles), 10 (diamonds) or 20 (circles) mg/kg. There were three animals per group. At various times post-dose, plasma total, unesterified and esterified cholesterol levels were measured. Baseline values were subtracted to determine the increase in cholesterol levels. Baseline total cholesterol: 0.41–1.08 g/L; unesterified cholesterol: 0.13–0.3 g/L; esterified cholesterol 0.28–0.78 g/L
3.1.2 Attenuated Inhibition of Atherosclerotic Plaque Progression
We observed a gradually greater decrease for unesterified and total cholesterol content in ligatured carotids as the dose of CER-001 or HDL3 increased from 2 to 5 to 10 mg/kg (Fig. 2a, b). For CER-001 dose levels above 10 mg/kg, the cholesterol content did not decrease but was at the same level as that of untreated mice (i.e. a U-shaped dose–response curve was observed). The ABCA1 protein content in the ligatured carotids paralleled that of the cholesterol content in a similar dose-related manner (Fig. 2c). We observed that at doses for which plaque formation in carotid (5 mg/kg of CER-001 and HDL3) is maximally inhibited, carotid artery ABCA1 protein levels are similar to those of untreated animals. In contrast, at the 50-mg/kg dose of CER-001 or HDL3, the carotid cholesterol content of plaque burden is similar to that of untreated animals, and the carotid artery ABCA1 protein level is decreased by half compared with untreated animals. Thus, down-regulation of macrophage ABCA1 induced by elevated concentrations of CER-001 or HDL3 appears to have attenuated the efficacy of the infused HDL to inhibit plaque formation in the ApoE−/− mouse ligatured carotid model. However, at the lower doses, increasing the dose of CER-001 and HDL3 up to that observed threshold slowed progression of carotid plaque while maintaining normal levels of ABCA1 expression.
Effect of increasing doses of CER-001 and HDL3 on mean (±standard error of the mean) atherosclerotic plaque progression in ligatured carotid of apoE−/− mice. The left carotid of apoE−/− mice (n = 12) was ligatured, fed with a high-cholesterol diet and treated (retro-orbital injection) every second day with CER-001 or HDL3 (eight infusions). The carotids were lipid extracted and cholesterol levels were determined by high-performance liquid chromatography. a Unesterified cholesterol. b Total cholesterol. c Protein level of ABCA1 measured in the ligatured carotids using western blot analysis. *p < 0.05; **p < 0.01; ***p < 0.001; ****p < 0.0001 vs. baseline. ABCA1 ATP-binding cassette transporter 1, apoE apolipoprotein E
3.2 Phase I Single Rising-Dose Clinical Study
The study enrolled 32 subjects and evaluated CER-001 at doses of 0.25–45 mg/kg. Thirty-one (97%) subjects completed the study. One subject was lost to follow-up after period 2 day 14 (subject did not return for the day 22 end-of-study visit and was not reachable at the telephone number provided; this subject did not experience any AEs during the trial). Baseline characteristics were similar across cohorts and dosing sequences (Table 2). Subjects were predominantly male (94%), Caucasian (88%), had a mean age of 34 years and a mean body mass index of 28 kg/m2. Mean baseline LDL-cholesterol was 136 mg/dL, mean HDL-cholesterol was 36 mg/dL and the mean LDL:HDL ratio was 3.9. Subjects had no chronic health problems and were not taking any concomitant therapies.
Plasma levels of ApoA-I and sphingomyelin increased in a dose-related manner. ApoA-I levels returned to baseline by 24 h post-dose for doses up to 10 mg/kg and by 72 h post-dose for doses above 10 mg/kg (Fig. 3). Sphingomyelin levels returned to baseline by 24 h post-dose for doses up to 5 mg/kg, by 72 h post-dose for doses from 10 to 30 mg/kg and by 7 days post-dose for subjects dosed with 45 mg/kg (data not shown).
CER-001 caused dose-dependent elevations in total plasma cholesterol (data not shown) as well as total and unesterified cholesterol in the HDL fraction (Fig. 4a, b), suggesting increased reverse lipid transport. Mobilisation in the HDL fraction of unesterified cholesterol was seen with a CER-001 dose as low as 2 mg/kg (mean 23% increase from baseline) and increased with dose. Triglyceride levels were transiently increased above levels seen with placebo at doses of 15 mg/kg and above (data not shown). Mobilisation of cholesterol, even at the higher doses, was not associated with significant elevation of liver enzymes (Fig. 5). These data support the further evaluation of CER-001 at a wide range of doses as potential therapy for patients with atherosclerotic diseases.
All doses of CER-001 were safe and well tolerated, with an AE profile similar to that observed with placebo (Table 3). Four of 32 subjects (12.5%) had an AE following a single dose of CER-001 vs. 3 of 32 subjects (9.4%) who had an AE following a single dose of placebo. No subjects had AEs considered by the investigator to be at least possibly related to the study drug and there did not appear to be any dose-related trends in the occurrence or type of AEs. There were no deaths, serious AEs or AEs that led to withdrawal from the study or study treatment.
The effects of CER-001 on clinical chemistry, haematology and coagulation parameters were comparable to placebo, including the effects on liver enzymes. No adverse effects of CER-001 on electrocardiograms were observed. No antibodies to ApoA-I were detected following single-dose administration of CER-001.
4 Discussion
4.1 Preclinical Findings
Dose-dependent increases in serum cholesterol levels occurred at all doses of CER-001 tested in the preclinical pharmacology and toxicity studies, which is the expected pharmacological effect of CER-001 administration. CER-001 at 20 mg/kg was considered the no adverse-effect level. Minimal adverse effects observed at doses of 50 and 100 mg/kg were considered secondary to increased cholesterol levels following CER-001 administration and were completely reversible during the treatment-free period. In a cardiovascular and respiratory primate safety study, CER-001 at doses up to 100 mg/kg was devoid of any adverse effects on blood pressure, heart rate and body temperature. A small but statistically significant increase in heart rate at the 100-mg/kg dose was considered loss of diurnal rhythm (data not shown). In the first single-dose clinical study, the starting dose was 0.25 mg/kg, as this was 1/80th of the safe dose (20 mg/kg) as established in the 4-week multiple-dose animal studies dosed every second day.
4.2 Phase I Single Rising-Dose Clinical Study Findings
In this phase I clinical study, following administration of CER-001, plasma ApoA-I levels increased in a dose-related manner, returning to baseline by 24 h post-dose for doses up to 10 mg/kg and remaining in circulation longer than 72 h post-dose for doses ≥10 mg/kg, suggesting a longer residence time of CER-001 in plasma. The administration of CER-001 caused elevations in plasma cholesterol, as well as total and unesterified cholesterol in the HDL fraction, suggesting increased reverse lipid transport. The mobilisation of unesterified cholesterol in the HDL fraction was seen with CER-001 doses as low as 2 mg/kg, indicating efficacy at very low doses and supporting the evaluation of a wide range of doses as potential therapy for patients with atherosclerotic disease.
CER-001 was well tolerated at all doses in all subjects with an adverse-event profile similar to that observed with placebo. CER-001 did not appear to affect clinical chemistry, haematology or coagulation parameters differently from placebo. No adverse effects of CER-001 were observed on electrocardiograms and no antibodies to ApoA-I were detected following single-dose administration of CER-001.
Overall, this article presents a series of preclinical and human volunteer data in which the initial preclinical findings with CER-001 have allowed accurate estimation of the human clinical dose level. The subsequent effectiveness observed with CER-001 in patients parallels that reported during the early development of the compound. At dose levels ≥2 mg/kg, CER-001 increased cholesterol mobilisation into the HDL fraction (up to sevenfold) and significant HDL increases were demonstrated. No drug-related AEs were observed at any dose. Importantly, there were no increases in hepatic enzymes despite a maximum cholesterol mobilisation ten times greater than that observed with prior HDL mimetics.
Clinical effectiveness of CER-001 has now been reported in phase II studies in patients with acute coronary syndrome, with higher doses being less effective than lower doses [7]—this reflects findings in the preclinical studies reported here and elsewhere [13] and can be explained by the down-regulation of ABCA1. Despite this concern of a down-regulation at higher doses, the clinical effectiveness of CER-001 has also been observed in plaque regression in patients with genetic dyslipidaemia or acute coronary syndrome [8–10].
HDL-directed therapy is a strategy intended to supplement LDL-cholesterol-lowering treatment. Proof of concept of the efficacy of CER-001 in the reverse lipid transport pathway and for regression of atherosclerotic burden in patients across the spectrum of defects in cholesterol homeostasis has now been demonstrated. This offers considerable optimism that CER-001 may address the residual risk of cardiovascular events that remains after maximum clinical benefit has been achieved using LDL-cholesterol-lowering therapies; the results of further studies involving CER-001 are eagerly awaited.
5 Conclusion
Preclinical pharmacological studies have shown that CER-001 produces dose-dependent increases in serum cholesterol levels, while the phase I study has demonstrated it to be well tolerated when administered to humans as a single dose up to 45 mg/kg and that it mobilises and eliminates cholesterol via reverse lipid transport.
References
Mattjus P, Slotte JP. Does cholesterol discriminate between sphingomyelin and phosphatidylcholine in mixed monolayers containing both phospholipids? Chem Phys Lipids. 1996;81:69–80.
Ramstedt B, Slotte JP. Interaction of cholesterol with sphingomyelins and acyl-chain-matched phosphatidylcholines: a comparative study of the effect of the chain length. Biophys J. 1999;76:908–15.
Guasch A, Deen WM, Myers BD. Charge selectivity of the glomerular filtration barrier in healthy and nephrotic humans. J Clin Invest. 1993;92:2274–82.
Rigotti A, Acton SL, Krieger M. The class B scavenger receptors SR-BI and CD36 are receptors for anionic phospholipids. J Biol Chem. 1995;270:16221–4.
Tardy C, Goffinet M, Boubekeur N, et al. CER-001, a HDL-mimetic, stimulates the reverse lipid transport and atherosclerosis regression in high cholesterol diet-fed LDL-receptor deficient mice. Atherosclerosis. 2014;232:110–8.
Zheng KH, van der Valk FM, Smits LP, et al. Recombinant human apolipoprotein A-I HDL CER-001 targets plaques in patients with atherosclerotic disease: the LOCATION study. Atherosclerosis. 2016;251:381–8.
Tardif JC, Ballantyne CM, Barter P, et al. Effects of the high-density lipoprotein mimetic agent CER-001 on coronary atherosclerosis in patients with acute coronary syndromes: a randomized trial. Eur Heart J. 2014;35:3277–86.
Kataoka Y, Andrews J, Duong M, et al. Greater regression of coronary atherosclerosis with the pre-beta high-density lipoprotein mimetic CER-001 in patients with more extensive plaque burden. Circulation. 2015;132(Suppl_3):A12156.
Hovingh GK, Smits LP, Stefanutti C, et al. The effect of an apolipoprotein A-I-containing high-density lipoprotein-mimetic particle (CER-001) on carotid artery wall thickness in patients with homozygous familial hypercholesterolemia: the Modifying Orphan Disease Evaluation (MODE) study. Am Heart J. 2015;169(736–42):e1.
Kootte RS, Smits LP, van der Valk FM, et al. Effect of open-label infusion of an apolipoprotein A-I-containing particle (CER-001) on reverse cholesterol transport and artery wall thickness in patients with familial hypo-alphalipoproteinemia. J Lipid Res. 2015;56:703–12.
Usui S, Hara Y, Hosaki S, Okazaki M. A new on-line dual enzymatic method for simultaneous quantification of cholesterol and triglycerides in lipoproteins by HPLC. J Lipid Res. 2002;43:805–14.
Nissen SE, Tsunoda T, Tuzcu EM, et al. Effect of recombinant ApoA-I Milano on coronary atherosclerosis in patients with acute coronary syndromes: a randomized controlled trial. JAMA. 2003;290:2292–300.
Tardy C, Goffinet M, Boubekeur N, et al. HDL and CER-001 inverse-dose dependent inhibition of atherosclerotic plaque formation in apoE−/− mice: Evidence of ABCA1 down-regulation. PLoS One. 2015;10(9):e0137584.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
These studies were funded by Cerenis Therapeutics, France. Editorial support was provided by Greensplash, funded by Cerenis Therapeutics.
Conflict of interest
All authors are in full-time employment with Cerenis Therapeutics, France.
Ethics approval
All procedures in the human phase I study were in accordance with the 1964 Helsinki Declaration (and its amendments) and Good Clinical Practice guidelines, and the local ethics committee approved the study. For the animal studies, all institutional, national and good laboratory practice guidelines for the care of the laboratory animals were followed.
Consent to participate
All participants provided written informed consent prior to entering the study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Keyserling, C.H., Barbaras, R., Benghozi, R. et al. Development of CER-001: Preclinical Dose Selection Through to Phase I Clinical Findings. Clin Drug Investig 37, 483–491 (2017). https://doi.org/10.1007/s40261-017-0506-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40261-017-0506-3