Abstract
Introduction
To investigate the demographics, acute management and compliance rates of severe chemical eye burn cases that presented to the largest eye hospital in the United Kingdom (UK).
Methods
All patients presenting to the Moorfields Eye Hospital emergency department are registered on the electronic patient administration system (PAS). A search of the PAS for patients assigned a preset diagnosis of ‘chemical injury’ was performed for the period from 1 January to 31 March 2016. The results of the PAS search and handwritten clerking notes were reviewed. Eyes that were found to have ≥ 33% limbal ischaemia or limbal staining, or corneal haze that obscured the details of the iris, were recorded as having severe chemical injuries.
Results
55 patients had mild chemical eye burns, and 11 eyes of 10 patients had severe burns. Average patient age was 37 years (SD 22 years) and 22 years (SD 10 years) for mild and severe chemical injuries, respectively. 53% of the mild injuries and 90% of the severe injuries were in males. 7 (70%) of the 10 severe injuries were assault-related. In the severe chemical injuries group, first presentation to the emergency department was 24 h or more postinjury in 50% of the patients, 33% stopped ascorbate and citrate drops (ocular pain), 40% stopped attending clinical follow-up sessions, and 45% of the eyes had a final best corrected visual acuity (BCVA) of 6/18 or worse.
Conclusion
A significant proportion of the severe ocular chemical burns were assault-related. Delayed presentation and poor treatment adherence and follow-up attendance rates are significant challenges in patients with severe chemical burns. Patient education and public health awareness are important strategies. These findings also raise the question of whether these patients, who are mostly young males, should be admitted to improve treatment adherence rates and visual outcome.
Similar content being viewed by others
Introduction
Severe ocular chemical burns are an ophthalmic emergency requiring immediate treatment. First-aid measures such as immediate irrigation of the ocular surface are essential to minimise the burden of disease. An ophthalmologist’s input at each stage of the disease process is important for minimising long-term complications and improving visual outcomes.
About two-thirds to three-quarters of all severe chemical eye injuries are due to alkalis and occur at work, affecting people of working age [1, 2]. Men are much more commonly affected (by 3–8:1) than women [1,2,3,4]
A rising trend in assault-related chemical eye burns over the last few years has recently been reported [5]. The British Ophthalmological Surveillance Unit (BOSU) reported that assault accounted for 33% of the severe chemical ocular injuries that occurred between December 2005 and November 2006 [6]. This is concerning due to the poor prognosis associated with assault-related ocular burns. In contrast to those with work-related burns, patients with assault-related burns do not have immediate access to first-aid equipment or guidelines. Furthermore, a chemical used for assault (commonly ammonia) is likely to be highly toxic, whereas in the workplace there can be exposure to a wider range of chemicals. Finally, assault victims do not wear protective eyewear. All of these factors contribute to the poor prognosis of assault-related chemical eye burns.
The study reported in the present paper was carried out because the authors noted that patients with severe chemical eye burns appeared to have poor adherence to treatment. We sought to investigate the rates of compliance of severe ocular chemical burn patients with both treatment and clinical follow-up attendance. A secondary aim of this study was to consider the proportion of such injuries that resulted from an assault, and to identify any increasing trend in assault-related chemical burns.
Methods
All patients presenting to the Moorfields Eye Hospital emergency department are registered on the electronic patient administration system (PAS). The diagnosis and management of each patient are entered and recorded on the PAS. Written patient notes detailing presentation, findings and management are also provided for all patients.
The PAS requires doctors to choose from a range of preset diagnoses for each patient. One of these preset diagnoses is ‘chemical injury’. This enabled a search of the PAS to be performed in order to identify all patients diagnosed with chemical injury between 1 January 2016 and 31 March 2016. The written notes were then reviewed for these patients, and required preset data were inputted.
Chemical injuries were categorised as mild or severe. Cases where the diagnosis of chemical injury was incorrect were recorded as having no chemical injury.
Chemical burns with no limbal staining, no limbal ischaemia and no corneal haze were recorded as mild chemical injuries. For mild injuries, the presence/absence of an epithelial defect was recorded, and whether the setting was work-related.
Eyes found to have any of the following clinical findings were classified as severe ocular chemical burns:
-
≥ 33% (120°) limbal ischaemia
-
Corneal haze causing obscuration of iris details
-
≥ 33% (120°) limbal staining
These injuries correlate to Roper-Hall grade III–IV injuries [7]. Limbal staining was also included as a marker of limbal stem cell injury in accordance with the Dua et al. classification system [8]. Patient demographics, initial clinical findings, initial management, follow-up times and findings, final recorded vision and complications were recorded.
Compliance with Ethics Guidelines
All procedures performed in these patients were approved by the clinical audit department of Moorfields Eye Hospital (reg number: CA16/CEC/16) and were in accordance with the ethical standards of the national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Results
No Chemical Injury
80 patients were retrieved from a search for ‘chemical injury’ in the PAS. Twelve patients were found to have ‘no chemical injury’. Diagnoses of chemical injury were either accidental (i.e., inputted instead of another diagnosis such conjunctivitis/trauma/etc.) or were recorded because the patient had reported contact of the eye with a chemical but there were no abnormal findings on clinical examination. No written records were found for 3 patients.
Mild Chemical Injuries
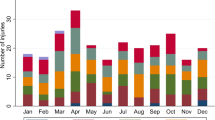
55 patients were found to have mild chemical injuries. 53% of the patients were male and 55% were in the 15–35 year age group. The average age was 37 years (SD: 22 years, range: 1–91 years).
31 patients had a non-work-related injury; 4 had a work-related injury. In the other 15 patients, it was not possible to determine if the nature of the injury was work-related.
29% had an epithelial defect (ED), 67% had no ED, and no comment was made about the presence or absence of an ED in the other 4%.
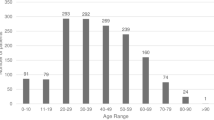
66% of the patients presented within 12 h of the chemical burn, and 87% of patients presented within 24 h (Fig. 1).
Severe Chemical Injuries
Eleven eyes of 10 patients were found to have severe chemical injuries. 90% of patients were male and 80% were in the 15–35 years age group. The average age was 23 years (range 2–39 years, SD 10 years), and there was only one female patient.
The initial presentation findings that led to the categorisation of these eyes into the severe chemical injuries group are summarised in Table 1.
The clinical notes with the initial clinical findings were not found for patient 5; only the findings at first follow-up, performed 6 days postinjury, were available for this patient.
Patients 6 and 8 presented to the emergency department 4 days after the eye had been splashed with ammonia, and the initial clinical findings were first recorded on day 4. The extent of the injury (e.g. limbal staining) may have been worse in the 24 h following injury.
Five out of 10 (50%) patients presented within 12 hours of the chemical burn. Three patients presented at 48 hours, and 2 patients presented 4 days following the chemical burn (Fig. 1).
Cause of Injury
The chemical burns were due to assault in 7 out of 10 patients. In 3 of those 7 assault cases, ammonia was confirmed as the causative chemical agent. The agent was not known in the other 4 assault cases, but was documented as an alkali in 1 case. In the 3 non-assault-related cases, the chemicals were washing machine detergent liquid (accidental injury), methyl ethyl ketone peroxide (alkali, work-related injury), and unknown, respectively.
Treatment: Prescription and Compliance
All patients were treated in line with the Moorfields Eye Hospital NHS Foundation Trust protocol for severe ocular chemical burns. This is summarised in Table 2.
Nine out of 10 patients were treated according to the hospital protocol. However, a child was initially treated with chloramphenicol eye drops only; following the first follow-up appointment, prednisolone 0.5% four times daily was added.
Most patients were prescribed all the medications in the protocol, as shown in Table 3. Two of the patients were prescribed lower doses of ascorbic acid tablets and doxycycline tablets than the protocol. The reason for this was not documented.
One patient had poor compliance with the medication due to pain and polypharmacy. Three patients could not tolerate the burning sensation with citrate and ascorbate eye drops, and 1 patient stopped cyclopentolate drops due to pain.
Visual Outcomes
The recorded visual acuity at first and last presentation are shown in Table 4. The best-corrected visual acuity (BCVA) improved to 6/6 or better in 4 out of 9 eyes. Five eyes had a vision of 6/18 or worse, for reasons mentioned below. It was not possible to test visual acuity in the child, but the epithelial defect and inflammation resolved fully, and there was no evidence of residual complications.
Patient 2 was only followed up for 14 days, as he failed to attend further appointments. His vision at 14 days was poor due to persistent corneal haze.
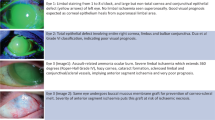
Patient 5 had a severe assault-related chemical burn from from ammonia, and developed poor vision due to limbal stem cell failure (corneal neovascularisation/conjunctivalisation), corneal scarring and cataract formation. Vision at 5 months was still counting fingers.
Patient 7 had a visual acuity of 6/18 at 1 month postinjury due to anterior stromal and subepithelial scarring of the cornea.
Patient 9 only attended one follow-up visit, in which his visual acuity (VA) was 6/36 and the corneal epithelial defect edges were opposing (i.e. a closed epithelial defect). It is not known if he suffered long-term complications (namely, limbal stem cell deficiency) due to 9 clock hours of limbal staining at presentation.
Although patient 8 attained a vision of 6/6 at last follow-up, there was inferior corneal conjunctivalisation due to inferior limbal stem cell failure.
Patient 10 developed left upper lid cicatricial entropion, cornea conjunctivalisation, persistent corneal epithelial defect, fungal keratitis and left cornea perforation. The BCVA was therefore hand movements. Vision in the less severely affected eye was 6/6 at last follow-up, and the only complication was mild upper lid entropion.
The number of patients was too small to permit any meaningful statistical analysis of visual outcomes. It is worth noting, however, that the 2 cases (patient 5 and the left eye of patient 10) with the worst initial BCVA ended up with very poor vision.
Follow-Up Attendance
Four (40%) out of 10 patients failed to attend follow-up visits, despite only one of them having a visual acuity of 6/6 and the others having last recorded visual acuities of 6/18, 6/24 and 6/36. Patients who did not attend were not called, and it is not known why these patients failed to attend. All 4 of these patients were victims of alleged assault. The time to first emergency department presentation was 48 h or more in 3 of those 4 patients.
Of the 4 patients who failed to attend, one attended 3 follow-up visits (up to 14 days postinjury) and 2 attended 4 follow-up visits (up to 1 month following injury). One attended only 1 follow-up visit 4 days postinjury.
Discussion
There are different phases in the pathophysiology of ocular chemical burns [9]. Adequate and timely treatment at each phase helps to minimise complications at the next phase. Compliance with treatment is therefore of the utmost importance for reducing short-term and long-term complications. As far as we know, the rates of compliance with treatment and clinical follow-up following ocular chemical burns have not previously been investigated. We therefore sought to investigate the adherence rates of a 3-month cohort of severe ocular chemical burn patients who attended the largest ophthalmological emergency department in the UK.
The notable findings of this study are delayed first presentation to the emergency department, reduced adherence to treatment and reduced follow-up attendance in patients with severe ocular chemical burns. Reduced treatment adherence is a recognised challenge in young adults, with factors such as reduced understanding of medication benefits, reduced family support and psychosocial difficulties contributing to this [10, 11]. These factors may explain the late presentation to the emergency department. Patients may have reduced awareness of the severity of their chemical injuries, or the benefit of timely treatment. Level of education or socioeconomic status may be factors that contribute to late presentation, although our study did not explore this. In terms of compliance with treatment, the most notable finding was compliance with ascorbate and citrate eye drops. It was found that 3 out of 9 patients with severe ocular chemical injuries did not take topical ascorbate and citrate drops due to the ocular pain caused by these drops. As this is a retrospective study, it was not possible to ascertain if these patients were given adequate information about the clinical benefit of using the prescribed eye drops. Patients who feel significant pain due to drops may stop using the drops because they are concerned about causing further damage to the eye, or because of poor pain tolerance. Patient education can be used as one of several strategies to facilitate improvements in adherence rates as well as to simplify medication regimens. We also advocate warning the patients about the pain caused by these drops, and that such pain is to be expected. The pain caused by drops such as potassium ascorbate (i.e. ascorbic acid) can result in reduced treatment adherence. Studies investigating alternative ocular delivery routes of ascorbic acid to the eye are encouraged. Systemic ascorbic acid on its own does not appear to be sufficient to replenish depleted aqueous humour levels. Animal studies show that systemic ascorbic acid is not sufficient to prevent corneal melts, unlike topical ascorbic acid [12].
The number of drops prescribed following chemical eye burns, as well as oral medications, leads to polypharmacy. Polypharmacy is known to result in reduced compliance [13]. This is perhaps a more marked phenomenon in a younger working-age group where the demands of life conflict with the importance of timely medication management. Preparations which combine multiple agents into one medication may improve compliance in these cases. Better explanation of the seriousness of severe chemical burns and the importance of treatment is encouraged for all patients. Written leaflets are generally available for common disorders, such as conjunctivitis, blepharitis, posterior vitreous detachment, etc. Written information on ocular chemical burns is rare, however, and may be of value. Involving relatives and friends in such discussions may also improve treatment adherence. A combination of these strategies aimed at increasing patient awareness of the severity of this disease and the benefits of treatment may serve to improve compliance levels.
Prescribing drops such as corticosteroids, ascorbate or citrate to be instilled one- to two-hourly may also contribute to reduced compliance. These topical drops are important for minimising inflammation and stromal melts and facilitating stromal healing. However, there is no robust evidence in the literature as to the optimal frequency of use of these drops. Furthermore, the effect of changing the frequency of use of drops (e.g. corticosteroids) in different grades of severe chemical eye burns (e.g. Roper-Hall grade III vs grade IV) has not been adequately investigated. Reducing the frequency of drops that cause pain (e.g. ascorbate) may help improve compliance. Arguably, however, reduced patient compliance may result in the patient using the drops less frequently than prescribed regardless; for example, a patient may be prescribed two-hourly drops but use them only every 4 h, or they may be prescribed drops four times a day but use them only twice a day. Research studies and guidelines to better define the treatment requirements and regimens in different grades of chemical eye injuries would be of value to ophthalmologists.
The compliance rates amongst patients with work-related ocular chemical burns may be different from those with assault-related burns, but we do not have evidence for this. However, this is important to mention, as it is a possible confounding factor. Our study found that the patients who stopped attending planned follow-up sessions were those with assault-related injuries. The rate of severe chemical burns due to assault (70%) is alarming. We advocate considering the admission of patients (who are mostly young males) with severe chemical burns, especially if a risk factor for reduced compliance is suspected.
One of the most notable findings of this study is the high incidence of severe chemical eye burns. Eleven patients were found to have severe chemical burns in our study which looked at patients presenting to one centre over a 3-month period. This compares to 12 patients in a UK population-wide study covering the 12-month period of December 2005 to November 2006 [6]. Although our criteria for a severe chemical ocular burn differ from those used in that study, this comparison is nevertheless alarming, and cannot be explained by the change in the size of the UK population. The emergency department of Moorfields Eye Hospital is in East London, an area closely associated with media reports of chemical assault crimes [5]. The proportion of severe burns sustained due to an alleged assault in our study is high, which is concerning. The proportion of assault-related severe burns is higher in our study (70%) than in the BOSU study (33.3%), which may account for the high incidence of severe burns in a 3-month period. Other reasons for this difference may be that our study was conducted in London, which may not accurately reflect the rest of the UK population due to factors such as differences in population demographics, compliance with safety measures in the workplace or the incidence of assault-related injuries. Another possible reason is that more relevant patients can be identified through retrospective analysis of electronic patient records than by relying on ophthalmologists’ reports of injuries.
There are a few limitations to this study. Firstly, although it includes a large patient cohort for an ocular chemical burns study, the time period studied is relatively short. We are unable to report the visual outcomes of mild chemical burn cases, as almost all such patients are seen just once in the emergency department and then discharged. Another weakness is that some patients who presented during the studied time period may have not been included. This is because there are preset diagnoses in the PAS that doctors must choose from. If the diagnosis is not found on this list of preset diagnoses, then ‘other diagnosis’ can be selected and the diagnosis can be entered manually. Theoretically, therefore, some doctors may have chosen this option and inputted ‘chemical injury’ manually. However, all doctors receive training in the PAS, so we expect this to be a rare occurrence.
Conclusion
A significant proportion of the severe ocular chemical burns considered in this study were assault-related. Delayed presentation and poor treatment adherence and follow-up attendance rates are significant challenges in patients with severe chemical burns. Patient education and public health awareness are important strategies. These findings also raise the question of whether these patients, who are mostly young males, should be admitted to reduce compliance issues and improve visual outcomes.
References
Hong J, Qiu T, Wei A, Sun X, Xu J. Clinical characteristics and visual outcome of severe ocular chemical injuries in Shanghai. Ophthalmology. 2010;117(12):2268–72.
Kuckelkorn R, Kottek A, Schrage N, Reim M. Poor prognosis of severe chemical and thermal eye burns: the need for adequate emergency care and primary prevention. Int Arch Occup Environ Health. 1995;67(4):281–4.
Xie Y, Tan Y, Tang S. Epidemiology of 377 patients with chemical burns in Guangdong province. Burns. 2004;30(6):569–72.
Haring RS, Sheffield ID, Channa R, Canner JK, Schneider EB. Epidemiologic trends of chemical ocular burns in the United States. JAMA Ophthalmol. 2016;134(10):1119–24.
Miller R, Pywell S, Leon-Villapalos J, Atkins J. Chemical burn assaults: is the media coverage representative? Burns. 2018;44(4):1021–2.
Macdonald ECA, Cauchi PA, Azuara-Blanco A, Foot B. Surveillance of severe chemical corneal injuries in the UK. Br J Ophthalmol. 2009;93(9):1177–80.
Roper-Hall MJ. Thermal and chemical burns. Trans Ophthalmol Soc UK. 1965;85:631–53.
Dua HS, King AJ, Joseph A. A new classification of ocular surface burns. Br J Ophthalmol. 2001;85(11):1379–83.
Wagoner MD. Chemical injuries of the eye: current concepts in pathophysiology and therapy. Surv Ophthalmol. 1997;41(4):275–313.
McGrady ME, Brown GA, Pai AL. Medication adherence decision-making among adolescents and young adults with cancer. Eur J Oncol Nurs. 2016;20:207–14.
Bregnballe V, Schiøtz PO, Boisen KA, Pressler T, Thastum M. Barriers to adherence in adolescents and young adults with cystic fibrosis: a questionnaire study in young patients and their parents. Patient Prefer Adher. 2011;5:507–15.
Pfister RR, Paterson CA, Spiers JW, Hayes SA. The efficacy of ascorbate treatment after severe experimental alkali burns depends upon the route of administration. Invest Ophthalmol Vis Sci. 1980;19(12):1526–9.
Marcum ZA, Gellad WF. Medication adherence to multidrug regimens. Clin Geriatr Med. 2012;28(2):287–300.
Acknowledgements
We thank the participants of the study.
Funding
No funding or sponsorship was received for this study or the publication of this article. The article processing charges were funded by the authors.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship of this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Authorship Contributions
Mukhtar Bizrah collected and analysed the data and wrote the manuscript. Ammar Yusuf helped with data analysis and manuscript revision. Sajjad Ahmad supervised the implementation of the study, interpreted data and edited the manuscript. All authors read and approved the final manuscript.
Disclosures
Mukhtar Bizrah, Ammar Yusuf and Sajjad Ahmad declare that they have no personal, financial, commercial, or academic conflicts of interest.
Compliance with Ethics Guidelines
All procedures performed in these patients were approved by the clinical audit department of Moorfields Eye Hospital (reg number: CA16/CEC/16), and were in accordance with the ethical standards of the national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Data Availability
The datasets generated during and/or analysed during the current study are not publicly available due to patient confidentiality, but are available from the corresponding author on reasonable request.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Author information
Authors and Affiliations
Corresponding author
Additional information
Enhanced Digital Features
To view enhanced digital features for this article go to https://doi.org/10.6084/m9.figshare.7751408
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Bizrah, M., Yusuf, A. & Ahmad, S. Adherence to Treatment and Follow-Up in Patients with Severe Chemical Eye Burns. Ophthalmol Ther 8, 251–259 (2019). https://doi.org/10.1007/s40123-019-0173-y
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-019-0173-y