Abstract
Introduction
The aim of this study was to observe the effect of stress caused by neuropathic pain on serum cortisol concentration and expression of 11β-hydroxysteroid dehydrogenase type I enzyme (11βHSD1) in spinal cord and dorsal root ganglions (DRG) and investigate the role and mechanism of curcumin in the neuropathic pain of stressful rats. Neuropathic pain is a prevalent disease that greatly impairs the patients’ quality of life. A lack of the understanding of its etiology, inadequate relief, development of tolerance and potential toxicity of classical antinociceptives warrant the investigation of the newer agents to relieve this pain. The aim of the present study was to explore the antinociceptive effect of curcumin and its effect on expression of 11β-hydroxysteroid dehydrogenase type I enzyme (11βHSD1) in spinal dorsal horn and DRG in chronic constriction injury (CCI) mode of neuropathic pain of rats.
Methods
Seventy-two male Sprague-Dawley rats were randomized into four groups with 18 rats in each: sham operation group (Sham), chronic constrictive injury group (CCI), solvent contrast group (SC), and curcumin-treated group (Cur100). Curcumin, 100 mg/kg/day intraperitoneal, was given for 14 days starting from the first day after operation in the Cur100 group. Paw thermal withdrawal latency (PTWL) and paw mechanical withdrawal threshold (PMWT) of rats were measured 2 days pre-operative, and 1, 3, 5, 7, 10, and 14 days post-operative. The animals were deeply anesthetized and blood was taken from the heart, the lumbar segment (L4, 5) of the spinal cord and DRG were dissected out and homogenized. The change of cortisol was measured by enzyme-linked immunosorbent assay and the change of 11βHSD1 expression was determined by immunochemistry and Western blot.
Results
Compared with sham group, PTWL and PMWT significantly decrease after operation in the CCI group; serum cortisol concentration was significantly increased and the expression of 11βHSD1 was significantly increased in the CCI group. Comparing with CCI group, the PMWT and PTWL were increased and the serum cortisol concentration was decreased and the expression of 11βHSD1 was inhibited in Cur100 group.
Conclusion
Stress caused by neuropathic pain triggers release of cortisol to the blood and expression of 11βHSD1 would increase at the same time. Curcumin could alleviate thermal and mechanical hyperalgesia induced by CCI and inhibit the serum cortisol concentration and expression of 11βHSD1 in the spinal cord and DRG.
Similar content being viewed by others
Introduction
Neuropathic pain can be considered a form of chronic stress, and neuropathic pain patients often have disturbance of the hypothalamic–pituitary–adrenal (HPA) axis, including abnormal cortisol levels [1]. In addition, the 11β-hydroxysteroid dehydrogenase type I enzyme (11βHSD1) is the key enzyme that converts cortisone to cortisol in humans, and 11-dehydrocorticosterone to corticosterone in rodents [2]. Glucocorticoid that includes cortisol and corticosterone has its effect through glucocorticoid receptors (GRs). A previous study has shown that central GRs play an important role in development and maintenance of neuropathic pain by participating and regulating the expression and function of N-methyl-d-aspartate receptor [3]. The authors and other previous studies have shown that curcumin can attenuate thermal and mechanical hyperalgesia in a diabetic mouse model of neuropathic pain [4, 5].
The current study employs a rodent neuropathic pain model [chronic constriction injury (CCI) of the sciatic nerve] to assess the effect of chronic stress on the releasing of cortisol in the serum and expression of 11βHSD1 in spinal dorsal horn and dorsal root ganglion (DRG). In addition, we explore the effect of curcumin on thermal hyperalgesia and mechanical allodynia and its effect on expression of 11βHSD1 in spinal dorsal horn and DRG.
Methods
Procedure for Chronic Constriction Injury
Chronic constriction injury rats were produced by loosely ligating a common sciatic nerve according to the method of Bennett and Xie [6]. Rats were anesthetized with sodium pentobarbital (40 mg/kg, intraperitoneal). The common sciatic nerve was exposed at the level of the middle of the thigh by blunt dissection through biceps femoris, 4 ligatures (4-0 chromic gut suture) were tied loosely around it with about 1 mm spacing. The incision was closed in layers. The success of the modeling was confirmed by detecting thermal and mechanical hyperalgesia.
Experimental Animal and Grouping
Male Sprague-Dawley rats were obtained from the Animal Center of Wenzhou Medical College (Zhejiang, China) and were housed in groups of 2–4 in 40 × 60 × 30 cm plastic cages with soft bedding under a 12/12 h day/night cycle; water and food pellets were available ad libitum. Experiments were conducted with the approval of the Animal Care Committee of Wenzhou Medical College and according to the guidelines for investigations of experimental pain in animals published by the International Association for the Study of Pain [7]. Sham and CCI rats were randomly selected and divided in four groups with six animals in each. The first group consisted of sham rats, the second group was the CCI control rats, the third group was the solvent control (SC) group, and the fourth group consisted of the CCI rats (Cur100) which were treated with curcumin 100 mg/kg/day by peritoneal injection for 14 days starting from the first day after the CCI operation. The sham and solvent control groups received the vehicle of curcumin [dimethyl sulfoxide (DMSO)], and the CCI group was treated with nothing.
Behavioral Studies
Paw thermal withdrawal latency (PTWL) and paw withdrawal mechanical threshold (PWMT) of rats were measured 2 days pre-operative and 1, 3, 5, 7, 10, and days 14 post-operative. Mechanical allodynia was assessed by use of von Frey filaments. Rats were placed in individual plastic boxes (20 × 25 × 15 cm) on a metal mesh floor and allowed to acclimatize for 30 min. The filaments were presented, in ascending order of strength, perpendicular to the plantar surface with sufficient force to cause slight bending against the paw and held for 6–8 s. Brisk withdrawal or paw flinching were considered as positive responses. The PWMT was determined by sequentially increasing and decreasing the stimulus strength (the “up-and-down” method) [8], and the data were analyzed using the nonparametric method of Dixon, as described by Chaplan et al. [8].
Thermal hyperalgesia was assessed with the PTWL to radiant heat according to the protocol of Hargreaves et al. [9]. Rats were placed in clear plastic cages on an elevated glass plate and allowed to acclimatize for 30 min before testing. A radiant thermal stimulator was focused onto the plantar surface of the hind paw through the glass plate. The nociceptive endpoints in the radiant heat test were the characteristic lifting or licking of the hind paw, and the time to the endpoint was considered the PTWL. To avoid tissue damage, a cut-off time of 30 s was used [10]. There were five trials per rat with 5-min intervals between trials. The mean PTWL was obtained from the final three stimuli [11].
Enzyme-Linked Immunosorbent Assay
Enzyme-linked immunosorbent assay (ELISA) was used to detect serum cortisol concentration. On 3, 7, and 14 days post-operative, the blood was taken from the heart of the rats with pentobarbital sodium (40 mg/kg) and centrifuged to get supernatant between 10 a.m. and noon to minimize the variation of the plasma cortisol level. The cortisol ELISA-kit was purchased from Boyun Biotechnology Company (Shanghai, China). The standard curve was generated using the reference standard set supplied in the kit. The samples were measured according to the instructions accompanying the kit. The results were read using a microplate reader (Elx-800, Bio-Tek instruments, Inc, Winooski, VT, USA) at wavelengths of 450 nm. The plasma cortisol concentration was calculated based on the standard curve and presented in nanograms per milliliter.
Immunohistochemical Staining
Immunohistochemistry was used to detect 11βHSD1 immunoreactivities in spinal dorsal horn and DRG. On 3, 7, and 14 days post-operative, rats anesthetized with pentobarbital sodium (40 mg/kg, intraperitoneal) were perfused through the ascending aorta with 0.9% NaCl, followed by freshly prepared 4% paraformaldehyde in 0.1 M phosphate-buffered saline (PBS; pH 7.4). The lumbosacral spinal cords and L4–5 DRG which were ipsilateral to the operation were carefully dissected out, embedded in paraffin. Five-micron-thick cross-sections of paraffin-embedded tissue were cut and mounted on Vectabond adhesive-coated slides. Sections were dewaxed in xylene and rehydrated in ethanol, then washed in PBS, sections were incubated with the primary antibody (11βHSD1, 1:500, Experimental Center of Rockefeller University, USA) dilution at 4 °C for 24 h. Sections were washed twice with PBS and incubated in goat anti-rabbit serum (1:200) (Chemicon Group, USA) for 1 h. This step was followed by three washes in PBS and staining using the ABC kit. The DAB chromogenic reaction was monitored carefully for about 5 min and PBS was used to stop the reaction in time.
Western Blot Analysis
Western blot was used to detect 11βHSD1 expression in spinal dorsal horn and DRG. Rats were rapidly (<1 min) killed through decapitation after being anesthetized with pentobarbital (50 mg/kg, intraperitoneal). The lumbosacral spinal cords and L4,5 DRG which were ipsilateral to the operation were carefully dissected out and homogenized in SDS sample buffer containing a mixture of proteinase inhibitors. The lumbar segments and corresponding DRG were harvested because CCI has the major impact at these spinal segments. Protein samples and the loading β-actin were separated via 10% gel electrophoresis and electroblotted onto polyvinylidene fluoride (PVDF) membranes. Nonspecific binding sites were blocked by incubating PVDF membranes for 1 h in PBS containing 5% low-fat dry milk. Membranes were incubated overnight at 4 °C with primary antibodies (11βHSD1, 1:3,000; Rockefeller University, New York, NY, USA) and for 1 h at room temperature with anti-rabbit secondary antibodies (1:1,000; Chemicon Group, New York, USA). Blots were developed using an enhanced chemiluminescence detection system (ECL; Amersham Pharmacia Biotech, Piscataway, NJ, USA) according to the manufacture’s instruction. The Western analysis was made in triplicates. The density of specific bands was measured with a computer-assisted imaging analysis system and normalized against loading controls. Differences were compared using repeated measures one-way analysis of variance (ANOVA) followed by post hoc Newman–Keuls tests.
Statistical Analysis
Results were expressed as the mean ± SE of at least three separate experiments and analyzed using the SPSS16.0 statistical program (SAS Institute Inc, Cary, North Carolina). The behavior data were analyzed by using repeated measures ANOVA followed by the Fisher’s least significant difference (LSD) test. Differences with P values of <0.05 were considered significant.
Results
The Change of PWMT and PTWL Baseline in Each Group
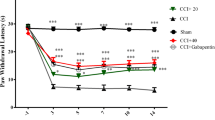
There was no statistical difference of PWMT and PTWL baseline among the groups. After operation, the sham group exhibited no significant difference of PWMT and PTWL at different time points. PWMT and PTWL of CCI group began to decline from day 1 after the operation and reached the minimum value (52.6% of basal value) on day 10, then recovered slowly, but it was still lower than the basic value on day 14. The CCI group exhibited a significant decrease of PWMT and PTWL compared with sham group (P < 0.01) (Fig. 1). There was no difference between CCI group and SC group (P > 0.05) (Fig. 1).
Effect of curcumin treatment on the paw withdrawal thermal latency in CCI rats (n = 6 rats/group; mean ± SD; **P < 0.01 vs. sham group; # P < 0.05 vs. CCI group; △ P < 0.05 vs. SC group). sham operation group (Sham), chronic constrictive injury group (CCI), solvent contrast group (SC), and curcumin-treated group (Cur100)
Effect of Chronic Curcumin Treatment on Nociceptive Threshold of PWMT and PTWL
When curcumin treatment started from the day 1 after the operation for 14 days, no statistic difference of PWMT and PTwL was exhibited between the Cur100 group and CCI group on 1, 3, and 5 days after operation. However, PWMT and PTWL of the Cur100 group were improved as compared to CCI group on day 7 (P < 0.05) (Fig. 1). On day 10 after the operation, PWMT and PTWL of Cur100 was improved compared to the CCI group (P < 0.05) (Fig. 1). On day 14, PWMT and PTWL of Cur100 group was significantly improved as compared to CCI group and SC group (P < 0.05) (Figs. 1, 2).
Effect of curcumin treatment on the paw withdrawal mechanical threshold with von Frey filaments in CCI rats (n = 6 rats/group; mean ± SD; **P < 0.01 vs. sham group; # P < 0.05 vs. CCI group; △ P < 0.05 vs. SC group). Sham operation group (Sham), chronic constrictive injury group (CCI), solvent contrast group (SC), and curcumin-treated group (Cur100)
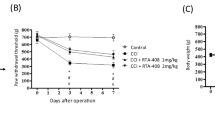
The Change of Serum Cortisol Concentration in Each Group
After operation, the sham group exhibited no significant difference of serum cortisol concentration at different time points (P > 0.05); compared with sham group, serum cortisol concentration of CCI and SC groups increased significantly on day 3 (P < 0.01), reached a peak point on day 7 (36.32 ± 15.71) and on day 14 it was still higher than sham group (P < 0.05). Compared with CCI group, serum cortisol concentration of Cur100 group declined (P < 0.05) (Fig. 3).
Effect of Neuropathic Pain of CCI Mode on Expression of 11βHSD1 in Spinal Dorsal Horn and DRG
The effect of neuropathic pain on 11βHSD1 expression was determined in the superficial dorsal horn laminae I–III of the lumbar enlargement and DRG, which are areas that are involved in the transmission of nociceptive inputs and sympathetic outflow. In the current study, constitutive 11βHSD1 expression was weak to absent in the sham group. In association with the development of neuropathic pain in CCI group, there was a time-dependent upregulation of 11βHSD1 within the superficial dorsal horn laminae I–III of the lumbar enlargement and DRG compared with sham group (P < 0.01), as revealed by immunohistochemical staining and Western blot. Spinal 11βHSD1 expression began to increase on day 3 and continue to rise on day 7 and day 14 of the experimental period as compared with the sham group (P < 0.01) (Figs. 4, 5, 6, 7, 8, 9, 10, 11).
Effect of curcumin on the expression of 11βHSD1 in dorsal root ganglion after CCI operation (mean ± SD, n = 6). **P < 0.01 vs. sham group; # P < 0.05 vs. CCI group. Sham operation group (Sham), 11β-hydroxysteroid dehydrogenase type I enzyme (11βHSD 1 ), chronic constrictive injury group (CCI), solvent contrast group (SC), and curcumin-treated group (Cur100)
Effect of curcumin on the expression of 11βHSD1 in spinal dorsal horn after CCI operation (mean ± SD, n = 6). **P < 0.01 vs. sham group; # P < 0.05 vs. CCI group. 11β-hydroxysteroid dehydrogenase type I enzyme (11βHSD 1 ), sham operation group (Sham), chronic constrictive injury group (CCI), solvent contrast group (SC), and curcumin-treated group (Cur100)
Effect of curcumin on the expression of 11βHSD1 in spinal dorsal horn after CCI operation (mean ± SD, n = 6). **P < 0.01 vs. Sham group; # P < 0.05 vs. CCI group. Sham operation group (Sham), 11β-hydroxysteroid dehydrogenase type I enzyme (11βHSD 1 ), chronic constrictive injury group (CCI), solvent contrast group (SC), and curcumin-treated group (Cur100)
Effect of curcumin on the expression of 11βHSD1 in dorsal root ganglion after CCI operation (mean ± SD, n = 6). **P < 0.01 vs. Sham group; # P < 0.05 vs. CCI group. Sham operation group (Sham), 11β-hydroxysteroid dehydrogenase type I enzyme (11βHSD 1 ), chronic constrictive injury group (CCI), solvent contrast group (SC), and curcumin-treated group (Cur100)
Effect of curcumin 100 mg/kg intraperitoneal on expression of 11βHSD1 in spinal dorsal horn on day 7 after CCI operation. From the left to the right Sham group, CCI group, SC group, Cur100 group (×400). Sham operation group (Sham), 11β-hydroxysteroid dehydrogenase type I enzyme (11βHSD 1 ), chronic constrictive injury group (CCI), solvent contrast group (SC), and curcumin-treated group (Cur100)
Effect of curcumin 100 mg/kg intraperitoneal on expression of 11βHSD1 in DRG on day 7 after CCI operation. From the left to the right Sham group, CCI group, SC group, Cur100 group (×200). Sham operation group (Sham), 11β-hydroxysteroid dehydrogenase type I enzyme (11βHSD 1 ), chronic constrictive injury group (CCI), solvent contrast group (SC), and curcumin-treated group (Cur100)
Semi-quantitative value of 11βHSD1 expression within the spinal dorsal horn after CCI on 3, 7, and 14 days post-operative. From right to left Sham group, SC group, CCI group, Cur100 group. Sham operation group (Sham), 11β-hydroxysteroid dehydrogenase type I enzyme (11βHSD 1 ), chronic constrictive injury group (CCI), solvent contrast group (SC), and curcumin-treated group (Cur100)
Semi-quantitative value of 11βHSD1 expression within the spinal dorsal horn after CCI on 3, 7, and 14 days post-operative. From right to left Sham group, SC group, CCI group, Cur100 group. Sham operation group (Sham), 11β-hydroxysteroid dehydrogenase type I enzyme (11βHSD 1 ), chronic constrictive injury group (CCI), solvent contrast group (SC), and curcumin-treated group (Cur100)
Effect of Chronic Curcumin Treatment on Expression of 11βHSD1 in Spinal Dorsal Horn and DRG
The result from this experiment showed that upregulation of 11βHSD1 expression within the spinal dorsal horn and DRG was blocked by the administration of curcumin on days 3, 7, and 14 by both immunohistochemical staining and Western blot in the Cur100 group compared with the CCI group (P < 0.05) (Figs. 4,5, 6, 7, 8, 9, 10, 11).
Discussion
The present study demonstrates that: (1) the CCI group exhibited a significant decrease of PWMT and PTWL compared with sham group, this is in line with observation of Bennett and Xie [6]; (2) serum cortisol concentration was significantly increased and the expression of 11βHSD1 was significantly increased in the CCI group; (3) chronic treatment with curcumin significantly attenuated mechanical and thermal hyperplasia; (4) curcumin reduced the serum cortisol concentration and inhibited the expression of neuronal 11βHSD1 within the superficial spinal dorsal horn and DRG that were ipsilateral to the operation.
These findings indicate that curcumin prevents neuropathic pain through reducing the expression of neuronal 11βHSD1 within the superficial spinal dorsal horn and DRG. 11β-Hydroxysteroid dehydrogenases (11βHSDs) are the key enzymes that catalyze the interconversion of glucocorticoids (corticosterone in rodents) and their 11-keto-metabolites (11-dehydrocorticosterone). 11βHSD1 type 1 acts predominantly as a reductase in vivo, catalyzing the regeneration of active glucocorticoids and thereby promoting activation of GRs in target tissues [2]. The analysis of cloned gene sequence has discovered that CTGATACAG sequences are located in the promoter of 11βHSD1 gene-197–190 base-pairs; it strongly prompts that glucocorticoid is regulated by promoter of 11βHSD1 gene. It is also reported that glucocorticoid has induced effects on 11βHSD1 [12].
Neuropathic pain is a form of chronic stress and the HPA axis is activated; the hypothalamus secretes corticotrophin-releasing hormone (CRH) under the influence of serotonin from the amygdale. Subsequently, CRH stimulates the pituitary to release adrenocorticotropic hormone, which results in the production of glucocorticoid (cortisol) in the adrenal cortex. It has demonstrated that altered GR expression in limbic brain regions, adrenal gland hypertrophy in response to enhanced adrenocortical stimulation, chronic pain patients often have disturbances of the HPA axis and limbic system (e.g., hippocampus and amygdale) [1]; in addition, clinical studies suggest that chronic pain-induced dysfunction of the HPA axis may be involved in reduced sensitivity of GRs to glucocorticoid negative feedback [13].
Peripheral GRs play a significant role in the anti-inflammatory effects of glucocorticoids; however, GRs have also been located in spinal cord dorsal horn neurons. It has been found that activation of neuron GRs contributes to central changes related to neuronal injury [14]. In a previous study, the rats exposure to acute stress immediately prior to nerve injury increased neuropathic pain and rats treated with corticosterone exhibited increased allodynia compared to rats treated with the vehicle [15]. Another study has found that adrenalectomized CCI rats failed to develop neuropathic pain behaviors; however, the development of neuropathic pain behaviors after CCI is restored in adrenalectomy ADL rats when treated with dexamethasone [16]. Glucocorticoid action in cells is mediated by a specific receptor protein, the GR; the GR level increases in the CNS and it plays important role in the neuropathic pain. Inhibition of GRs with the GR antagonist RU38483 attenuates the development of neuropathic pain [16].
The present study has shown that stress caused by neuropathic pain triggers release of cortisol to the blood and expression of 11βHSD1 would increase at the same time. Curcumin could alleviate thermal and mechanical hyperalgesia induced by CCI and inhibit the serum cortisol concentration and expression of 11βHSD1 in spinal cord and DRG. Upregulation of 11βHSDs will activate glucocorticoid and promote activation of GRs. Glucocorticoid and GRs have been proven to be the key element in the neuropathic pain [3, 16]. It demonstrates that that curcumin’s attenuation of neuropathic pain is related to inhibition of the expression of 11βHSD1 in spinal dorsal horn and DRG. Curcumin has been used in Asian medicine for more than 4,000 years for the treatment of wounds, tumors, and inflammatory conditions. It is a very potent drug as a therapeutic or preventive agent for several major human diseases. Curcumin has been proven to inhibit p-Jun N-terminal kinase p-JNK and c-jun [5] in neuropathic pain model and inhibit tumor necrosis factor TNF-α and nitrogen monoxide (NO) in a diabetic mouse model of neuropathic pain [4].
Conclusion
Based on the present preliminary results, we conclude that stress caused by neuropathic pain triggers release of cortisol to the blood and expression of 11βHSD1 would increase in the spinal cord and DRG at the same time. Curcumin could alleviate thermal and mechanical hyperalgesia induced by CCI and inhibit the serum cortisol concentration and expression of 11βHSD1 in spinal cord and DRG. Further studies are warranted to explore the exact mechanism of curcumin’s antinociceptive effect.
References
Ulrich-Lai YM, Xie W, Meij JT, Dolgas CM, Yu L, Herman JP. Limbic and HPA axis function in an animal model of chronic neuropathic pain. Physiol Behav. 2006;88(1–2):67–76.
Dover AR, Hadoke PW, Macdonald LJ, Miller E, Newby DE, Walker BR. Intravascular glucocorticoid metabolism during inflammation and injury in mice. Endocrinology. 2007;148(1):166–72.
Wang S, Lim G, Zeng Q, Sung B, Yang L, Mao J. Central glucocorticoid receptors modulate the expression and function of spinal NMDA receptors after peripheral nerve injury. Neuroscience. 2005;25(2):488–95.
Sharma S, Kulkarni SK, Agrewala JN, Chopra K. Curcumin attenuates thermal hyperalgesia in a diabetic mouse model of neuropathic pain. Eur J Pharmacol. 2006;536(3):256–61.
He L, Cao H, He D, Li X, Li J, Lian Q. Effect of curcumin on neuropathic pain in rats. China J Anesthesiol. 2008;28(9):790–3.
Bennett GJ, Xie YK. A peripheral mononeuropathy in rat that produces disorders of pain sensation like those seen in man. Pain. 1988;33(1):87–107.
Zimmermann M. Ethical guidelines for the investigations of experimental pain in conscious animals. Pain. 1983;16:109–10.
Chaplan SR, Bach FW. Quantitative assessment of tactile allodynia in the rat paw. J Neurosci Meth. 1994;53:55–63.
Hargreaves K, Dubner R, Brown F, Flores C, Joris J. Hyperalgesia. Pain. 1988;32:77–88.
Ji GC, Ma F, Zhang YQ, Wu GC. Thermal hyperalgesic effects induced by intracerebroventricular injection of interleukin-1beta in rats. Sheng Li Xue Bao. 2002;54:325–8.
Sun YY, Luo C, Li Z, Chen J. Differential actions of intrathecal nociceptin on persistent spontaneous nociception, hyperalgesia and inflammation produced by subcutaneous bee venom injection in conscious rats. Sheng Li Xue Bao. 2004;56:321–7.
Armario A, Restrepo C, Castellanos JM, Balasch J. Dissociation between adrenocorticotropin and corticosterone responses to restraint after previous chronic exposure. Life Sci. 1985;36(22):2085–92.
Blumer D, Zorick F, Heilbronn M, Roth T. Biological markers for depression in chronic pain. J Nerv Ment Dis. 1982;170:425–8.
Cameron SA, Dutia MB. Lesion-induced plasticity in rat vestibular nucleus is dependent on glucocorticoid receptor activation. J Physiol. 1999;518:151–8.
Alexander JK, DeVries AC, Popovich PG. Stress-induced enhancement of neuropathic pain is mediated by corticosterone. Brain Behav. Immun. 2006;20:e1–e6.
Wang S, Lim G, Zeng Q, Sung B, Ai Y, Guo G, et al. Expression of central glucocorticoid receptors after peripheral nerve injury contributes to neuropathic pain behaviors in rats. J Neurosci. 2004;24(39):8595–605.
Acknowledgments
All named authors have met the ICMJE criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval for the version to be published.
This study was supported by the external cooperation program of Wenzhou Science and Technology Bureau (Zhejiang, China).
Conflict of interest
Y. Xiang Di, C. Hong, L. Jun and G. Renshan declare no conflict of interest.
Compliance with ethics guidelines
Experiments were conducted with the approval of the Animal Care Committee of Wenzhou Medical College and according to the guidelines for investigations of experimental pain in animals published by the International Association for the Study of Pain.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0), which permits use, duplication, adaptation, distribution, and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Di, Y.X., Hong, C., Jun, L. et al. Curcumin Attenuates Mechanical and Thermal Hyperalgesia in Chronic Constrictive Injury Model of Neuropathic Pain. Pain Ther 3, 59–69 (2014). https://doi.org/10.1007/s40122-014-0024-4
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40122-014-0024-4