Abstract
Introduction
The Japanese government’s current policy is to encourage hospitals to discharge hospital patients with schizophrenia earlier and provide them with community care. This study aims to analyze clinical and economic outcomes of different discharge strategies in psychiatric hospitals in Japan.
Methods
A simulation was conducted to compare patient relapse and hospital revenues for different discharge plans. We constructed a decision tree where each tree consists of a different Markov chain that models hospital revenue for four different discharge plans: discharge of the patient after 1, 2, or 3 months, or 4 months or more. The simulation also included variations in the medical treatment regimen in an outpatient setting as part of the discharge strategy. In particular, we looked at the choice between risperidone long-acting injectable (RLAI) and generic risperidone (RIS GE).
Results
The use of RLAI in an outpatient setting reduced the number of rehospitalizations compared to generic risperidone use under all discharge plans. Different discharge plans were associated with differences in economic outcomes as well. One of the key revenue drivers for the hospital was the continuation of treatment in the outpatient setting after discharge.
Conclusion
The use of RLAI in an outpatient setting could help to prevent rehospitalization, thereby contributing to better community care.
Funding
The Rapid Service Fee was funded by Janssen KK.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Avoid common mistakes on your manuscript.
Introduction
Schizophrenia is a serious mental illness with considerable economic impact and is regarded as the most expensive illness among all psychiatric disorders in terms of health care expenditure per patient [1]. A recent Japanese study estimated the annual financial burden caused by the disease to exceed 3.5 million Japanese yens (JPY) per patient (approximately US $30,000) [2]. Most of the costs can be attributed to the loss of working ability, as patients with schizophrenia face a higher likelihood of being unemployed [3]. Hospitalization has been identified as another significant cost driver in Japan, the United States, [4, 5] and Europe [6, 7].
The Japanese population is covered by the mandatory Japanese universal health insurance (UHI), which allows equal access to primary care and hospital services. However, significant co-insurance rates apply, meaning that a big share of the medical bill must be paid out of pocket by the patient themselves. For people below the age of 70, the co-insurance rates are 30% and decrease to 10% when a patient turns 70. To promote equal access to the health care system, the absolute out-of-pocket amounts are capped with ceilings dependent on income. The ceiling for low income households, for example, is JPY 35,400 (USD 307) per month. The main features of Japanese psychiatric care are the large number of psychiatric hospital beds and very long lengths of stay for schizophrenia patients, which differ from the care provided in other industrialized countries. Official estimates report an average hospital stay to last 298 days, down from 496 in 1989 [8], which is by far the longest worldwide [9]. A survey of 139 Japanese hospitals revealed that 46.8% of the patients hospitalized with schizophrenia had already spent more than 5 years hospitalized [10]. Another, more recent observational study of 8000 Japanese schizophrenia patients reported an average hospitalization period of 3242 days [11].
Why are Japanese patients not discharged into the community sooner? One reason might be that families prefer their relatives to stay in a hospital due to the negative perception of mental illness in the community. Stigmatizing attitudes in response to mental disorders are reported to be severe in Japan [12], which might be linked to the old Japanese character for the word schizophrenia, which literally reads as “the disease of disorganized mind” or “Seishin Bunretsu Byou” [13]. In 2002, this Japanese term was changed to “Togo Shitcho Sho” or “integration disorder” to reduce discrimination and stigmatization [14]. Stigmatization is such an issue that only 7% of Japanese psychiatrists inform their patients about a diagnosis of schizophrenia; often, patients remain uncertain about the disease they are suffering from [15]. Moreover, households with a family member who is suffering from schizophrenia are afraid of domestic abuse and violence. A recent survey among 302 Japanese citizens found that 27% of the respondents had already experienced an incident where a patient with schizophrenia had become violent with a family member [16].
Another explanation relates to the institutional setting of the health care market. Inpatient medical fees accounted for approximately 80% of psychiatric hospital revenue in 2013 [17]. General psychiatric beds are financed by a “fee-for-service system”, which may not offer incentives for the early discharge of patients. Therefore, the Japanese health care market creates an environment in which earlier discharge of schizophrenia patients is indirectly discouraged. Under a fee-for-service system, hospitals could benefit from selling medicine and taking advantage of the margin between the official reimbursement price and the wholesale price. The high degree of polypharmacy (i.e. medical treatment with more than one drug in one indication) and over-adherence (i.e. collection of more than one prescription of the same drug) is also a significant issue that might be related to the institutional framework. A recent observational study reported that more than 60% of patients with schizophrenia received antipsychotic polypharmacy [18]. Polypharmacy is more common in hospitals that operate under a fee-for-service system compared to those that operate under a flat fee remuneration system [19]. In addition, a claims data analysis of Japanese health insurance data revealed that more than 50% of patients were over-adherent to their medication [20].
The Japanese government is aware of the health care system’s institutional problems and has attempted to incentivize hospitals to discharge their patients earlier. In the course of reforming policy for mental health and welfare, the Ministry of Health, Labour and Welfare has developed a policy in which the treatment tier is differentiated based on its function and role in hospital care in order to encourage earlier discharge of patients with mental disorders [21]. At the same time, the government has made efforts to reduce the number of psychiatric hospital beds. Under the same bill, the government has also expressed its commitment to removing the stigma of mental disorders and promoting community-based care to facilitate patient discharge.
The Japanese government has also adjusted the financial incentive for psychiatric hospitals in order to achieve an earlier discharge and more extensive outpatient care. For example, it has put emphasis on psychiatric emergency and acute treatment beds where patients can be discharged as soon as possible while receiving efficient care. Under this scheme, psychiatric hospitals are encouraged to discharge patients sooner, because the medical fee decreases as the length of hospital stay increases. Psychiatric hospitals that strategically promote patient discharge can claim additional medical fees such as the so-called “discharge coordination” fee.
The aim of this paper is to analyze the aspect of relapses in patients with schizophrenia and the related economic ramifications they have in psychiatric hospitals in Japan. In particular, we seek to investigate whether the above-mentioned incentives are enough to encourage early discharge and relapse prevention. For this purpose, we simulated hospital decisions and calculated revenues for four different discharge plans (discharge within 1, 2, or 3 months, or 4 months or more). We also studied the economic consequences of alternative medical treatment strategies, namely risperidone long-acting injectable (RLAI)and generic risperidone. This step was executed by means of an economic simulation, since a simulation can help to identify critical functional and relational aspects in complex systems [22].
Methods
Model Overview and Assumptions
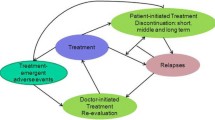
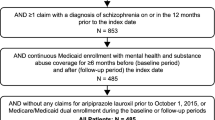
The patient flow was simulated by means of a decision tree (Fig. 1), where each tree consists of a different Markov model that models both outcomes and hospital income for four different discharge plans: discharge of the patient after 1, 2, or 3 months, or 4 months or later (Fig. 2). For each strategy, comparisons were made based on the difference between the prescription of either RLAI or generic risperidone (RIS GE) in outpatient settings, which represent two different typical medical treatment options. While RLAI is administered by a physician every 2 weeks by means of an injection, RIS GE is self-administrated orally on a daily or bi-daily basis. The list price for a monthly treatment of RLAI is JPY 8111 compared with JPY 781 for generic risperidone. On the other hand, significant cost offsets exist for LAIs in general with regard to hospitalizations due to better medication adherence [23].
The model was based on several assumptions for treatment-specific rehospitalization rates and the patient flow between inpatient and outpatient medical care. The Markov state-transition was characterized by the treatment-setting transitions. For each 1-month cycle, patients transitioned between or remained in the following treatment stages: acute psychiatric bed admission, basic psychiatric bed admission, outpatient visit, and treatment discontinuation. The difference between acute and basic psychiatric admission is that acute psychiatric bed admission is more care intensive and, therefore, reimbursed at a higher price than basic psychiatric bed admission. According to Japanese regulation, patients need to be moved from acute to basic psychiatric bed admission.
To each of these four discharge plans, we assigned a homogeneous patient cohort of 30 schizophrenia patients. In the Markov phase, we assumed that all patients in the cohort were first admitted to the hospital for acute psychiatric bed admission. After the first admission, each cohort was subjected to a different discharge plan. It is to be noted that as we model a homogeneous patient population, time of discharge is independent of specific patient characteristics. After discharge, patients continued their treatment as an outpatient of the same hospital. After this stage, two scenarios were possible: (1) the patient experienced a relapse that required rehospitalization, or (2) the patient discontinued their treatment at this hospital and left the model. Rehospitalization can occur either as a basic psychiatric bed admission or as an acute psychiatric bed admission, depending on the time since the last hospital discharge. A rehospitalization within 3 months is reimbursed at the lower basic psychiatric bed admission rate.
Transition Probabilities
The probabilities for transitions per month both for the RIS GE and RLAI cases in the Markov model are presented in Table 1.
Transition probabilities between the psychiatric hospital treatment phases (S1–S3) and between some outpatient phases (S4–S6) were 1, as these are tunnel states with different medical fees covering a 1-month cycle. In outpatient phases, patients were at risk of a schizophrenia relapse. Transition probabilities for patients in outpatient settings (from S4, S5, S6–S8) were derived from the literature [24]. The transition probabilities for patients discontinuing their treatment (from S4, S5, S6, S7–S9) were based on the expert opinion of one of the authors, which in turn was based on the systematic observation of 37 patients in a hospital in Saitama, Japan. The transitions from S4, S5, S6–S7 represent the probability that an outpatient continues the treatment as an outpatient, meaning there no is relapse which requires a hospitalization nor does the patient leave the model by discontinuing the treatment at this hospital. In those states, both relapse probability as well as the expert opinion on treatment discontinuation is taken into consideration. Lengths of stay after a rehospitalization was modeled using data cited in the literature [25]. Annual rates were converted into monthly rates using the following formula: monthly rate = [(1 + annual rate)1/12] − 1.
Model Inputs
The model assumed the patient as well as the hospital perspectives. Hospital revenues were derived from the medical fee schedule applicable in Japan. Table 2 provides an overview of the Japanese reimbursement scheme for psychiatric hospitals, which provides for varying fees depending on care intensity (doctor and nurses per bed) or the type of hospital.
For our model, patients were assumed to have received psychotherapy I three times per month in an acute treatment bed, or psychotherapy II two times per month in a basic psychiatric bed. The two kinds of psychotherapy differ with respect to the qualification of the respective therapist. We assumed that each patient visited the hospital twice per month after discharge and then received psychotherapy. In the outpatient settings, day-care charges were claimed for each weekday, meaning they were claimed five times per week. These treatment schedules were constructed based on expert opinion. Table 3 provides an overview of the revenue and cost inputs that were incorporated into the model. All fees are in Japanese yens, and medical fee schedules are based on 2015 levels.
Hospital revenue comprised the fee for inpatient bed, inpatient services, outpatient visit, outpatient services, and drug administration. In the hospitalization states, hospitals claimed either psychiatric acute treatment admission fee I or the basic psychiatric admission fee. During the hospital stay, the fee for inpatient psychotherapy I or inpatient psychotherapy II can be claimed. After discharge, the fees for outpatient visits and psychotherapy visit were claimed. We further assumed that the day-care fees were claimed in outpatient settings.
Revenues from prescribing drugs were generated under the fee-for-service treatment settings: basic psychiatric bed and outpatient visit. The revenue was estimated by multiplying the drug price by the average drug margin, called yakka-saeki, that arises from the difference between wholesale prices and official list prices at which doctors and hospitals are reimbursed by health insurance providers [28]. Alternatively, prescription drugs were considered as a cost item under the bundled payment setting: psychiatric acute treatment bed. The cost was estimated by multiplying the drug price by 1 minus the drug margin. We assumed the average drug margin to be 8.8%, based on the value in September 2015 [29].
In addition to the hospital income, we recorded the number of rehospitalizations in the model as patient outcome. Rehospitalizations were counted if patients relapsed while in the outpatient setting (S4–S6) and returned to the inpatient setting (S1 or S8). Drug-specific relapse, discharge, and discontinuation rates are shown in Table 4.
Time Horizon and Discounts
The model simulated a 2-year time horizon to cover the typical duration of an episode of schizophrenia. In Japan, the mean lengths of untreated psychosis (DUP) for schizophrenia patients was 13.7 months [30]. The model did not assume the discount rate, because the interest rate in Japan was almost zero in 2015 [31].
Sensitivity Analysis
To test the robustness of the base-case results and identify factors influencing hospital income, a deterministic sensitivity analysis was conducted for treatment with RLAI. Various parameters were examined that are subject to a high degree of uncertainty including the probability of dropout from RIS GE regimen (±25%), discharge from psychiatric basic admission (±25%), and relapse in outpatient settings (24% using the price of olanzapine to a maximum of 40%, based on the price of conventional antipsychotics) [24].
Compliance with Ethics Guidelines
This study is based on a model that uses published data as well as the expert opinion of one of the authors as input variables. Therefore, ethical approval was not necessary.
Results
Patient Outcomes
For all discharge plans, the number of relapses over a 2-year period in simulated patients was lower in the patient cohort using RLAI than in the RIS GE (Table 5). Our model predicted 16 rehospitalizations within this 2-year period for the cohort consisting of 30 patients when treated with generic risperidone and discharged after 1 month. This numbers decreases to 10 if patients were treated with RLAI, which corresponds to a decrease of 38%. The number decreased with the length of the first hospital stay, as patients could stay on as outpatients for shorter periods of time during the model’s time horizon. For this reason, the model predicts a total of 14 hospitalization for generic risperidone patients when they are discharged after 3 month and the corresponding number for RLAI is 10 (−29%).
Economic Outcome
The 2-year revenue per patient increased as the lengths of hospital stays increased in both cohorts (RIS GE and RLAI; Table 6). The revenue per patient using RIS GE was JPY 3,897,715 for discharge after 30 days, JPY 4,418,599 for discharge after 2 months, JPY 4,917,610 for discharge after 3 months, and JPY 5,399,859 for discharge after 4 months or later. On the other hand, the revenue per patient using RLAI was JPY 4,181,432 for discharge after 30 days, JPY 4,638,366 for discharge after 2 months, JPY 5,082,435 for discharge after 3 months, and JPY 5,469,710 for discharge after 4 months or later.
In the comparison between treatment with RIS GE and treatment with RLAI in outpatient settings, we found the 2-year revenue was higher for the RLAI treatment group in all discharge plans (Fig. 3). The incremental revenue per patient was JPY 284,550 (7.3% increase) for discharge after 30 days, JPY 220,559 (5% increase) for discharge after 2 months, JPY 165,576 (3.4% increase) for discharge after 3 months, and JPY 70,481 (1.3% increase) for discharge after 4 months or later. We observed a decreasing incremental revenue as the hospital stay grew longer.
Sensitivity Analysis
Figure 4 presents the results of the deterministic sensitivity analysis for the cohort treated with RIS GE in the outpatient settings. The figure also highlights three parameters that had the strongest influence on hospital income for each discharge plan. A high probability of discontinuing treatment was negatively related to hospital revenue. Conversely, a high probability of relapse in outpatient settings and discharge from the psychiatric basic admission were positively related to the hospital revenue.
Overall, the hospital income ranged from JPY 3,854,112 to 3,972,794 for the discharge plan after 30 days, JPY 4,352,636 to 4,489,364 for the discharge plan after 2 months, JPY 4,834,186 to 4,985,630 for the discharge plan after 3 months, and JPY 4,642,067 to 6,183,856 for the discharge plan after 4 months or later. The precise factor which had the greatest impact on hospital revenue differed between the different discharge plans. In the discharge plan after 30 days or 2 months, the probability of treatment discontinuation had the most significant impact on hospital revenue. For the plans with discharge after 3 months and 4 months or later, the strongest influencing factor was the rate of patient discharge from basic admission.
Discussion
Based on a Markov model of schizophrenia patients in the Japanese health care system, we found that revenue-maximizing hospitals still had limited economic incentives for an early discharge of patients. This result remains true despite the significant efforts undertaken by Japanese health policy makers to reduce the lengths of stay in Japanese psychiatric hospitals. On the other hand, our simulation suggests that the choice of medicine in the outpatient setting could reduce relapse rates in patients while maintaining hospital revenue.
Lower relapse rates and higher hospital revenue could be compatible, because RLAI contributed to improved continuity in outpatient care at the same hospital, increasing day-care utilization. The results were robust to parameter changes. Our simulation results are also supported by empirical studies. A recent analysis of Japanese claims data showed that, after adjusting for age, gender, and comorbidity, the use of LAIs was associated with a reduction of the number of rehospitalizations compared to oral treatment (incidence rate ratio = 0.38) [32].
To give hospitals better incentives for discharging patients sooner, new methods of community care should be strengthened. A study by Keio University evaluated an early program that encouraged discharge into the community with the support from an assigned social worker. The results indicated that the majority (79%) of patients re-integrated into the community successfully [33]. The authors argued that the success of this program in a metropolitan city like Tokyo calls for a broader roll out. A more recent Japanese study followed 78 patients who were reintroduced into the community after the closure of a psychiatric hospital. The follow-up period was 5 years and during this time span patients underwent annual examinations that included measures of cognition, psychiatric symptoms, and social functioning. The results suggested that even schizophrenia patients who had been hospitalized for longer periods showed improvement in cognitive deficits after discharge from the hospital [34].
Although the community model is, in our view, key for any new concept of the care of schizophrenia sufferers in Japan, the burden on caregivers might also increase in the community model. Research from Japan reported a heavy burden on the caregivers was associated with a reduction of social interests, distress, avoidance, resignation, and a decline in the quality of service of the caregiver role [35]. Annual productivity losses of caregivers amounted to JPY 2.42 million per caregiver [36]. Systematic and extensive support for caregivers should therefore accompany the necessary transition towards the community model.
Limitations
A limitation of our study was that it was based on a simulation, which is necessarily subject to a high degree of uncertainty. Future research should be conducted to validate our conclusions empirically by means of an observational study. An empirical evaluation of the government’s health policy attempts to reduce the number of hospitalizations and the lengths of stay is also urgently required. It is also important to note that our simulation is not a cost-effectiveness analysis seeking to examine the relation between cost and benefits of a medical intervention.
Conclusion
In conclusion, we demonstrated that the use of RLAI in an outpatient setting supported both relapse prevention and hospital revenues, thereby contributing to better community care for schizophrenic patients in Japan.
References
Rössler W, Salize HJ, van Os J, Riecher-Rössler A. Size of burden of schizophrenia and psychotic disorders. Eur Neuropsychopharmacol. 2005;15(4):399–409.
Sado M, Inagaki A, Koreki A, et al. The cost of schizophrenia in Japan. Neuropsychiatr Dis Treat. 2013;9:787–98.
Nakamura Y, Mahlich J. Productivity and deadweight losses due to relapses of schizophrenia in Japan. Neuropsychiatr Dis Treat. 2017;13:1341–8.
Lin I, Muser E, Munsell M, Benson C, Menzin J. Economic impact of psychiatric relapse and recidivism among adults with schizophrenia recently released from incarceration: a Markov model analysis. J Med Econ. 2014;26:1–11.
Fitch K, Iwasaki K, Villa K. Resource utilization and cost in a commercially insured population with schizophrenia. Am Health Drug Benefits. 2014;7(1):18–26.
Willis M, Svensson M, Löthgren M, Eriksson B, Berntsson A, Persson U. The impact of schizophrenia-related hospital utilization and cost of switching to long-acting risperidone injections in Sweden. Eur J Health Econ. 2010;11(6):585–94.
Frey S. The economic burden of schizophrenia in Germany: a population-based retrospective cohort study using genetic matching. Eur Psychiatry. 2014;29(8):479–89.
Ministry of Health Labour and Welfare. Individual index of psychiatric care. Tokyo 2011.
OECD. Health data. Paris 2013.
Oshima I, Mino Y, Inmata Y. How many long-stay schizophrenia patients can be discharged in Japan? Psychiatry Clin Neurosci. 2007;61:71–7.
Sugibayashi Y, Yoshimura K, Yamauchi K, Inagaki A, Ikegami N. Influence of patient characteristics on care time in patients hospitalized with schizophrenia. Neuropsychiatr Dis Treat. 2014;10:1577–84.
Griffiths KM, Nakane Y, Christensen H, Yoshioka K, Jorm AF, Nakane H. Stigma in response to mental disorders: a comparison of Australia and Japan. BMC Psychiatry. 2006;6:21.
Kim Y, Berrios GE. Impact of the term schizophrenia on the culture of ideograph: the Japanese experience. Schizophr Bull. 2001;27(2):181–5.
Sato M. Renaming schizophrenia: a Japanese perspective. World Psychiatry. 2006;5(1):53–5.
Ono Y, Satsumi Y, Kim Y, et al. Schizophrenia: is it time to replace the term? Psychiatry Clin Neurosci. 1999;53:335–41.
Kageyama M, Yokoyama K, Nagata S, Kita S, Nakamura Y, Kobayashi S, Solomon P. Rate of family violence among patients with schizophrenia in Japan. Asia Pac J Public Health. 2015;27(6):652–60.
Ministry of Health, Labour and Welfare. Summary of a real-world analysis for hospital administration. Tokyo. 2013.
Nakagawa R, Ohnishi T, Kobayashi H, Wakamatsu A, Tanimura A, Morita K, Yamaoka T, Usui H, Ogawa Y, Fujino A, Yoshizawa K. The social functional outcome of being naturalistically treated with paliperidone extended-release in patients with schizophrenia. Neuropsychiatr Dis Treat. 2015;11:1511–21.
Okumura Y, Noda T, Ito H. Antipsychotic prescribing pattern of patients with schizophrenia in Japan: using the national database of health insurance claim information and specified medical checkups. Jpn J Clin Psychopharmacol. 2013;16:1201–15.
Kuwabara H, Saito Y, Mahlich J. Adherence and re-hospitalizations in patients with schizophrenia: evidence from Japanese claims data. Neuropsychiatr Dis Treat. 2015;11:935–40.
Central Social Insurance Medical Council. Report on the psychiatric care. Tokyo 2011.
Marshall D, Burgos-Liz L, IJzerman M, et al. Applying dynamic simulation modeling methods in health care delivery research—the SIMULATE checklist: report of the ISPOR Simulation Modeling Emerging Good Practices Task Force. Value Health. 2015;18:5–16.
Zeidler J, Mahlich J, Greiner W, Heres S. Cost-effectiveness of paliperidone palmitate for the treatment of schizophrenia in Germany. Appl Health Econ Health Policy. 2013;11(5):509–21.
Mahlich J, Nishi M, Saito Y. Modeling the budget impact of long-acting injectable paliperidone palmitate in the treatment of schizophrenia in Japan. Clin Outcomes Res. 2015;7:267–72.
Kelly DL. Comparison of discharge rates and drug costs for patients with schizophrenia treated with risperidone or olanzapine. Psychiatr Serv. 2001;52(5):676–8.
Ministry of Health, Labour and Welfare. Revision of the medical payment system in the area of mental disorder. Tokyo 2014.
Ministry of Health, Labour and Welfare. Information about the drug in the National Health Insurance drug price list and generic drug. Tokyo 2014.
Mahlich J, Roediger-Schluga T. Determinants of pharmaceutical R&D: evidence from Japan. Rev Ind Organ. 2006;28(2):145–64.
Central Social Insurance Medical Council. Report on 317th Central Social Insurance Medical Council. 2015.
Yamazawa R, Mizuno M, Nemoto T, Miura Y, Murakami M. Kashima H Duration of untreated psychosis and pathways to psychiatric services in first-episode schizophrenia. Psychiatry Clin Neurosci. 2004;58(1):76–81.
The Bank of Japan. Financial and economic monthly report. Tokyo 2015.
Cheung S, Hamuro Y, Mahlich J, Nakahara T, Sruamsiri R, Tsukazawa S. Drug utilization of japanese patients diagnosed with schizophrenia: an administrative database analysis. Clin Drug Investig. 2017;37(6):559–69.
Noda F, Clark C, Terada H, Hayashi N, Maeda K, Sato M, et al. Community discharge of patients with schizophrenia: a Japanese experience. Psychiatr Rehabil J. 2004;28(2):143–9.
Nemoto T, Niimura H, Ryu Y, Sakuma K, Mizuno M. Long-term course of cognitive function in chronically hospitalized patients with schizophrenia transitioning to community-based living. Schizophr Res. 2014;155(1–3):90–5.
Hanzawa S, Bae J, Tanaka H, Bae Y, Tanaka G, Inadomi H, et al. Caregiver burden and coping strategies for patients with schizophrenia: comparison between Japan and Korea. Psychiatry Clin Neurosci. 2010;64(4):377–86.
Sruamsiri R, Mori Y, Mahlich J. Productivity loss of caregivers of schizophrenia patients: a cross-sectional survey in Japan. J Ment Health. 2019;27(6):583–7.
Acknowledgements
We thank Ludo Croxford for proofreading the manuscript.
Funding
The Rapid Service Fee was funded by Janssen KK. Other than this, the research received no funding.
Authorship
All authors had full access to all of the data in this study and take complete responsibility for the integrity of the data and accuracy of the data analysis. All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
JM and YK designed the study and drafted the manuscript. YN performed the analysis, and IS contributed expert advice and revised it critically for important intellectual content.
Disclosures
Jörg Mahlich was employed at Janssen KK, Tokyo, Japan, during the conduct of the study. Jörg Mahlich moved to Germany to work for Janssen-Cilag. Yusuke Nakamura was employed at Janssen KK, Tokyo, Japan, during the conduct of the study. Yusuke Nakamura is now with Bayer Yakuhin. Isao Shibata has nothing to disclose.
Compliance with Ethics Guidelines
This study is based on a model that uses published data as well as the expert opinion of one of the authors as input variables. Therefore, ethical approval was not necessary.
Data Availability
The model is based on secondary data available in the public domain. The data sets analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Additional information
Enhanced Digital Features
To view enhanced digital features for this article go to https://doi.org/10.6084/m9.figshare.8949116.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License ( http://creativecommons.org/licenses/by-nc/4.0/ ), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Nakamura, Y., Shibata, I. & Mahlich, J. Modeling the Choice Between Risperidone Long-Acting Injectable and Generic Risperidone from the Perspective of a Japanese Hospital. Neurol Ther 8, 433–447 (2019). https://doi.org/10.1007/s40120-019-0147-y
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40120-019-0147-y