Abstract
Idiopathic pulmonary fibrosis (IPF) is a chronic progressive fatal disorder that remains difficult to treat. In this review, we examine non-pharmacological treatment modalities, including lung transplantation, pulmonary rehabilitation and palliation. Lung transplantation, the only therapeutic intervention that offers survival benefit, should be considered in all IPF patients with progressive disease who meet the International Society for Heart and Lung transplantation guidelines. Pulmonary rehabilitation improves exercise capacity, reduces dyspnoea and improves quality of life in IPF patients, and should be made available to patients. For those patients with advanced disease, palliative services offer symptom management, improved quality of life and psychological support for patients and their caregivers.
Similar content being viewed by others
Introduction
Idiopathic pulmonary fibrosis (IPF) is a progressive, debilitating and fatal disease. It is characterized by cough, unrelenting breathlessness and loss of lung function. Over a short period of time, older adults (with median age of 66 years) become housebound, oxygen dependent and increasingly debilitated. IPF causes respiratory insufficiency and eventually death. The estimated 5-year survival rate is 20–30 % after 5 years and carries a worse prognosis than many cancers [1••].
It is essential that a definitive diagnosis of IPF be made by a multidisciplinary team integrating clinical, laboratory, radiological, and pathological data [1••]. Medical therapies that will be tolerated by patients may be considered, albeit these have not shown to improve survival, or conclusively slow the progression of the illness [1••, 2••]. Patients should be offered access to clinical trials where they are available and followed up in a timely manner (every 3–6 months). Physicians should be mindful of changes in symptoms that could be indicative of infective exacerbations, pulmonary emboli or the development of pulmonary hypertension. Patients should be assessed for oxygen therapy and have access to pulmonary rehabilitation programs. Those patients who meet the eligibility criteria should be considered for lung transplantation. Referral to palliative services should be made for those patients who fail medical treatment, continue to progress and are not candidates for transplantation.
In this article, we focus on approaches of pulmonary rehabilitation, palliative care and lung transplantation for these patients.
Lung transplantation
Lung allocation score
The first successful lung transplantation in a patient with IPF patient was performed by the Toronto group in 1983. In the 1990s, it had become evident that many patients with IPF died awaiting transplant. Before May 2005, lungs were allocated in the United States by the time spent on the waiting list, without regard for the severity of the illness or likelihood of survival. With waiting times averaging 2 years, patients were referred early so that they could accumulate “waiting time”. The United Network for Organ Sharing (UNOS) introduced measures whereby patients with IPF who had accrued 6 months “waiting time” could be prioritized. Due to the growing number of patients on the waiting list, the increasing numbers of deaths while on the waiting list, and the scarcity of organ, a lung-allocation score (LAS) was developed by UNOS. Under the LAS system, a waiting list urgency measure (expected number of days lived without a transplant during an additional year on the waitlist) and a post-transplant benefit measure (expected number of days lived during the first year post-transplant) are calculated using an individual candidate’s clinical and physiological characteristics and the statistical models [3]. The LAS is defined as the transplant benefit measure minus the waiting list urgency measure. It is a score between 1 and 100, with higher score representing urgency and a greater transplant benefit. Even before the introduction of the LAS, numbers of transplanted IPF patients were increasing; numbers gradually increased from 16 % in 2000 to 28 % in 2009 [4••]. LAS appears to be achieving its objectives by reducing waitlist time for patients with IPF [5]; waiting list mortality has been reduced from 47 % [6] to 15 % [7•]. However, IPF patients still have the highest death rate among the diagnostic groups on the transplant waiting list [8••, 9].
Disease severity
Even before the response to initial medical therapy has been determined, early referral for transplant evaluation is preferred. No definitive staging system exists for assessing the severity of IPF, although patients usually progress from mild to moderate to severe respiratory limitation. Disease severity is assessed on the basis of underlying pathological features, high resolution computed tomography (HRCT) features, pulmonary function tests, 6-minute walk tests (6MWT) and coexistent pulmonary hypertension.
It is possible to perform detailed scoring of individual histopathological features that correlate with outcomes. Usual interstitial pneumonia (UIP) is characterized histopathologically by a temporal heterogeneity and has a poor prognosis. The number of fibroblastic foci, which are one of the pathologic characteristics in UIP, is a significant prognostic factor; a higher number of fibroblastic foci have also been associated with a decline of forced vital capacity (FVC) and diffusing capacity of the lung for carbon monoxide (DLCO) over the course of a year [10]. Nonspecific interstitial pneumonia (NSIP) is characterized histopathologically by temporally uniform interstitial pneumonia, and is associated with different clinical characteristics and prognoses [11, 12]. NSIP is divided into two subtypes, cellular and fibrotic; the former has an excellent prognosis compared to the latter [12].
HRCT has an important diagnostic role in the diagnosis of the subtype of IPF [13]. Reticular opacities and areas of honeycombing limited to sub-pleural and basilar areas are seen in IPF [14]. A ground-glass/consolidation predominant pattern is seen in NSIP [15]. HRCT may have important role in the prognostic significance in IPF [15, 16]. The presence of honeycombing predicts poor survival, and the extent of consolidation and ground-glass opacity correlates with serial time changes in lung function in fibrotic NSIP [15, 17].
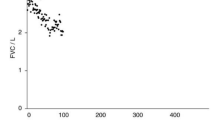
Pulmonary function tests are important in IPF to establish disease severity and as a prognostic indicator. A reduction in FVC and DLCO is associated with shorter survival. A DLCO of <35 % predicted at referral is highly predictive of mortality in IPF and NSIP [18–20], irrespective of the histological diagnosis [21]. Egan et al. have proposed a simple stratification system characterizing patients with IPF and patients with NSIP as having advanced disease if the baseline DLCO <39 % predicted, and limited disease if the DLCO is >40 % predicted [22]. A fall of >10 % in FVC or >15 % in DLCO in the first 6–12 months is associated with greater mortality [23•]. The composite physiological index (CPI) formulated by Wells et al. was constructed against the morphological severity of the disease in order to calibrate disease severity using PFTs in isolation [24]. The CPI score was a determinant of outcome in patients with IPF [21].
Exercise testing is utilized to evaluate the level of exercise intolerance in patients with cardiorespiratory diseases. Cardiopulmonary exercise testing (CPET) is considered the gold standard to study a patient’s level of exercise limitation and its causes. Fell and colleagues examined the role of maximal oxygen uptake during CPET as a predictor of mortality in 117 IPF patients. Patients with baseline maximal oxygen uptake less than 8.3 ml/kg/min during CPET had an increased risk of death, although they were unable to define a unit change in maximal oxygen uptake that predicted survival in their cohort of patients [25]. 6MWT parameters are considered to be important predictors of mortality among patients listed for lung transplantation. Oxygen desaturation to 88 % or less while breathing room air and the distance of less than 207 meters during 6MWT have been associated with a higher risk of death in IPF patients [26, 27]. Abnormal heart recovery in patients with IPF after a 6MWT is also predictive of poor survival [28].
Patients with advanced IPF have a high prevalence of pulmonary hypertension [29, 30]: 31–46 % of patients have a mean pulmonary arterial pressure (PAP) >25 mmHg at right-sided heart catheterization on evaluation for lung transplantation [30, 31] and 86 % at the time of transplantation [32]. In retrospective studies, poor outcomes have been identified in patients with IPF and concomitant pulmonary hypertension [29, 33, 34]; premature mortality post lung transplantation has been reported [35]. Pulmonary hypertension is also associated with the development of acute exacerbations and with poor survival in patients with IPF [36•].
Patient selection
IPF patients failing medical therapy should be carefully selected for transplantation (see Table 1). They must fulfill the general indications and have no contraindications. The older patient has a comparatively shorter survival time, which is likely attributable to comorbidities [9]. The median survival after transplantation for those >60 years and <50 years is approximately 3.5 and 5 years respectively. As a result an upper age limit of 65 has been utilized in eligibility criteria in many transplant centers; however, current evidence suggests that older patients are being considered for transplantation [9]. Of all lung transplants performed worldwide between 2000 and 2005, 5.3 % were for recipients older than 65 years [9].
Nutritional status of patients has been highlighted an important factor. Recipients with a BMI greater than 30 kg/m2 are at increased risk for 90-day mortality post transplantation [37]. A trend to higher 90-day mortality is seen among recipients with a BMI <17 kg/m2 [9, 38].
Potential recipients should be screened for occult disease during their pre-transplant evaluation. The age, smoking history and other risk factors predisposes these patients to chronic illnesses. Chronic medical conditions that may be adequately controlled and have not resulted in end-organ damage are acceptable in lung transplant candidates, e.g. hypertension. Optimization of certain diseases may be essential, including osteoporosis, diabetes, advanced cardiovascular disease and left ventricular dysfunction. For example, studies have shown satisfactory results for percutaneous revascularization or concomitant bypass surgery at the time of transplantation [39, 40].
Patients with malignancy in the last 2 years, except for cutaneous squamous and basal cell carcinoma, should not be considered for transplantation. A further absolute contradiction is active chronic viral hepatitis B, hepatitis C or AIDS. Patients with significant chest wall or spinal deformity; noncompliance with medication; current substance addiction (nicotine, alcohol or drugs) or that are active less than 6 months; untreatable psychosocial or psychiatric conditions; and poor rehabilitation potential should not be considered for transplantation [8••].
Guidelines for transplantation (see Table 2), as per International Society for Heart and Lung Transplant (ISHLT) [8••], include histological or radiographic evidence of UIP or with at least one of the following: (1) DLCO <39 % of predicted (2) A decrement in FVC >10 % during 6 months of follow up (3) a decrease in pulse oximetry below 88 % saturation during a 6MWT or (4) Honeycombing on HRCT (fibrosis score >2). For patients with NSIP, in conjunction with histological evidence there has to be (1) a DLCO <35 % predicted, or (2) a 10 % decrement in FVC or 15 % in DLCO during 6 months of follow up.
Transplant outcomes
Transplant procedures for IPF have steadily increased during the past decade, rising from 16 % of all procedures performed in 2000 to 28 % in 2009, approaching the proportion of the most common cause for the transplantation, chronic obstructive pulmonary disease (COPD) (30 %) [4••].
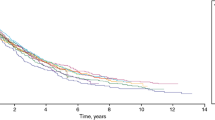
The overall median survival for all adult lung recipients is 5.5 years [4••]. The 3-month post transplant mortality is 15 % in patients with IPF, compared to 9 % in patients with COPD. In contrast to overall survival rates, median survival for IPF recipients is 6.9 years, 6.8 years for COPD recipients, and 10.4 years for cystic fibrosis recipients. Age at transplant and comorbidities in IPF and COPD patients may be attributable to the difference in survival compared to other diagnostic groups. The one-year survival for IPF patients with higher LAS (range 52–94.1) was 74 % compared to 84 % to lower LAS (range 31.1–37.8) [7•].
The decision to perform single lung transplantation (SLT), as opposed to bilateral lung transplantation (BLT), varies between centers. It has been shown that patients listed for only BLT, as opposed to SLT or BLT, are more likely to die on the waiting list [41•]. The scarcity of organs may be a determining factor. Previously, SLT were opted for, due to it being a limited operation with less cardiac manipulation, leading to reduced complication rates [7•]. However, surgical techniques have been refined, and at present there is a trend for increase in the number of bilateral procedures, with BLT accounting for 72 % of all transplants procedures across all diagnoses; over 50 % of IPF patients received BLTs [4••]. There is also a trend for BLT to be associated with better long-term survival than SLT in IPF recipients [42, 43].
In summary, lung transplantation may be an option for patients with progressive disease, minimal comorbidities and who fulfill ISHLT guidelines. We recommend early referral for lung transplantation evaluation rather than waiting until the patient has developed advanced disease.
Oxygen therapy
Dyspnoea is a determining factor in decline in the quality of life of patients. Experience of oxygen prescribing in IPF is extrapolated from two clinical trials in COPD patients, the Nocturnal Oxygen Therapy Trial (NOTT) and Medical Research Council (MRC) study [44, 45]. No clinical trials for the use of oxygen therapy in IPF patients have been performed. However, recent guidelines strongly recommend use of oxygen in patients showing clinical resting hypoxaemia (SpO2 of <88 %, PaO2 of 55–65 mmHg) [1••]. Patients demonstrating exertional hypoxaemia on 6MWT would benefit from ambulatory oxygen. Sleep-related hypoxaemia as assessed by overnight pulse oximetry should be managed with overnight oxygen. Finally, patients should undertake ‘fitness to fly’ test and oxygen should be organized for air travel [46•]. Patients should be reassessed regularly and oxygen prescriptions should be altered as oxygen demands change.
Pulmonary rehabilitation
In IPF impaired gas exchange occurs as a result of destruction of the pulmonary capillary bed, resulting in ventilation-perfusion mismatch and oxygen diffusion limitation. IPF patients report exertional breathlessness, hypoxaemia and fatigue that result in low physical activity. This leads to worsening exercise capacity, muscle deconditioning and worsening symptoms. Furthermore, immunosuppressive agents and corticosteroids lead to progressive myopathy. To break this self-perpetuating cycle, pulmonary rehabilitation (PR) may offer benefit in these patients. The consensus statement by the ATS/ERS defined PR as ‘an evidence-based, multidisciplinary, and comprehensive intervention for patients with chronic respiratory diseases who are symptomatic and often have decreased daily life activities. Integrated into the individualized treatment of the patient, PR is designed to reduce symptoms, optimize functional status, increase participation, and reduce health care costs through stabilizing or reversing systemic manifestations of the disease’ [47].
PR is proven to be beneficial in alleviating most symptoms of patients with COPD [48]. Until recently, most evidences for PR in IPF have been extrapolated from the data in COPD studies. The British Thoracic Society guidelines recommended that the patients with ILD should have access to a local PR programme using the same criteria for referral as for the patients with COPD [23•]. In recent years, there has been a concerted effort to generate evidence for PR in IPF patients.
PR has been associated with improvement in 6MWT distance, dyspnoea, and health-related quality of life parameters without improvement in pulmonary function [47, 49, 50]. The benefit seen is only modest when compared to COPD patients. Moreover, it was not sustained and did not improve health status [51•]. The lack of benefit may be due to lack of standardized protocol for PR, unknown optimal duration and absence of formal after care programme in IPF patients.
The duration of the PR may be an important factor. Many studies have ranged from 4 to 12 weeks. Salhi and colleagues demonstrated significant clinical improvement in patients with restrictive lung disease in maximal and sub-maximal exercise capacity, muscle force, and quality of life after 12 weeks, with further improvements after 24 weeks. The study grouped together IPF and non-IPF ILD patients, which may explain why the results are at variance with other studies that failed to show any sustained benefits of PR in IPF at 6 months [49, 50, 52•]. This observation calls for the development of an IPF-specific rehabilitation program to achieve the maximum benefit.
Peripheral and respiratory muscles weaknesses are also significant contributors to exercise limitation in IPF patients [53•]. Quadriceps force is related to exercise capacity in patients with IPF [54]. PR consisting of exercise training of muscle of the lower extremities improved overall exercise tolerance in IPF patients.
To date, fatigue in IPF has received little attention, unlike cancer related-fatigue [55]. A recent small pilot study showed that PR improved the mean fatigue level in patients with IPF, and in conjunction, there were trends toward improvement in anxiety, depression, energy level and physical health status. [56•].
A retrospective trial showed more pronounced, clinically significant improvement in 6MWT distance and dyspnoea in patients with the worst baseline walk distances [57]. It seems plausible that the immediate post-exacerbation enrolment of these patients over-estimated the severity in these patients. Two more recent studies contested this observation [58, 59•]. Holland and colleagues demonstrated, in a cohort of 44 patients with ILD (including 25 patients with IPF), a greater benefit of PR in patients with less severe IPF, less exercise-induced oxygen desaturation and lower right ventricular systolic pressure [58]. Kozu et al. have shown that IPF patients with less symptomatic disease and less severe functional limitation (MRC dyspnoea score of 2–3) do benefit from PR [59•]. The severe physical disability may render patients with advanced disease not to perform the PR at full intensity and achieve the maximum benefit. Hence, early referral of IPF patients for PR may be appropriate.
Further large randomized control trials are needed to explore the best IPF-specific PR protocol, optimum duration and after-care to assess long-term benefits.
Palliation
Palliative care aims to reduce the burden of symptoms and provide comfort to patients contemplating the end of life. In conjunction with relief from physical suffering, it improves quality of life by alleviating emotional suffering, acknowledging the goals and values, and giving consideration for psychological and spiritual support for patients and their caregivers [60]. Patients with IPF should have access to palliative services in the hospital, in their own homes and be able to avail of hospice facilities.
Advance care planning, a discussion between a patient and their care providers, should be undertaken when patients have time and are able to make decision about life-prolonging therapies. These discussions should occur in the outpatient department or after admission into hospital [61, 62•, 63•]. With the patient’s agreement, these discussions should be documented, regularly reviewed, and communicated to key persons involved in their care.
Advance directives clarify refusal of treatment or what patients do not wish to happen. This involves assessment of mental competency as the decision can be legally binding. It also strengthens the role of the Lasting Power of Attorney to enable a nominated proxy person to make decisions about medical and social welfare issues [63•]. In contrast, advance statements are not legally binding, but are invaluable in determining future provision of care. The patient’s concerns, their personal goals for care, their comprehension about their illness and prognosis and their preference for care or treatment that may be beneficial in the future are documented [63•].
Discussions with IPF patients should include resuscitation procedures in the event of cardiopulmonary arrest and mechanical ventilation. There is a high rate of mortality, between 87 % [64] and 96 % [65], associated with mechanical ventilation in IPF patients [66, 67]. Non-invasive ventilation has not been evaluated in a palliative care setting. This should be explained to patients and their caregivers [1••].
Palliation requires symptom management. Dyspnoea and cough have been the most frequently reported symptoms in IPF [68, 69]. The cause of breathlessness can be multi-factorial: respiratory (disease progression), cardiovascular (pulmonary hypertension), mechanical (muscle wasting) and psychological (depression and anxiety).
There are a plethora of scales and scores that attempt to quantify the breathlessness [70•, 71], although none has been specifically developed for use either in the IPF population or in the context of palliation. A longitudinal study in IPF reported that the MRC dyspnoea score was the most significant single predictor of survival and was a sensitive tool in detecting IPF progression [72•]. For patients on a palliative care pathway, both oxygen and opioids should be considered. There are no definitive studies examining the role of opioids, with the exception of one small study of 11 patients in the terminal stages of IPF that showed that a low dose of diamorphine improved subjective breathlessness and mean pulse rate [73•].
For many patients with IPF, cough is more debilitating than breathlessness. Cough can be difficult to treat and can be attributed to the illness itself, exacerbations, gastro-oesophageal symptoms and difficulty with sleeping. Recurrent wakening can impact quality of life. The Leicester Cough questionnaire is the most frequently used measure of cough associated with IPF. It is a 21-item questionnaire that is subdivided into three domains: social, psychological and physical. It has been found to correlate well with objective cough counts in patients with IPF [73•]. Codeine and opioids are effective antitussives; however, no trials support their routine use in IPF [74]. Thalidomide has been shown to suppress cough [75] and improve the quality of life [76•].
Anxiety and depression are also prevalent symptoms in IPF patients [77]. These can be precipitated by the chronic symptoms, inability to cope with the illness and the poor prognosis itself. Qualitative studies with patients with COPD and ILD describe patients’ understanding of acute dyspnoea as an experience inextricably related to anxiety and emotional functioning. The Hospital Anxiety and Depression Scale (HADS) is frequently used in patients with IPF. Whether depression and anxiety are experienced as separate entities in IPF in relation to ongoing symptoms requires further exploration. Patients should be offered psychological and counselling support, and antidepressants should be considered in patients who do not respond to above measures.
The UK Regional Study of Care for the Dying identified that patients with chronic lung disease at the end-of-life had physical and psychological needs similar to those with lung cancer [78]. End-of-life studies in IPF are urgently needed to determine the physical and psychological burden of this disease and to improve palliative care provision.
Conclusion
It is of paramount importance that IPF patients have access to both pharmacological and non-pharmacological therapies. Patients should be assessed on a regular basis and treatments should be evaluated and adjusted accordingly. Those who are eligible should be referred for clinical trials. Patients with progressive disease and who meet the ISHLT guidelines should be referred for lung transplantation. Supportive measures including oxygen and pulmonary rehabilitation should be made available. For those patients with advanced disease, referrals to palliative services should be made.
References
Papers of particular interest, published recently, have been highlighted as:• Of importance •• Of major importance
•• Raghu G, Collard HR, Egan JJ, et al. An official ATS/ERS/JRS/ALAT statement: idiopathic pulmonary fibrosis: evidence-based guidelines for diagnosis and management. Am J Respir Crit Care Med. 2011;183:788–824. Reference guidelines for the management of IPF.
•• Adamali HI, Maher TM. A review of current and novel therapies for Idiopathic Pulmonary Fibrosis. Drug Des Devel Ther. 2012 (in press) Comprehensive review on pirfenidone and promising upcoming therapies.
Davis SQ, Garrity Jr ER. Organ allocation in lung transplant. Chest. 2007;132:1646–51.
•• Christie JD, Edwards LB, Kucheryavaya AY, et al. The Registry of the International Society for Heart and Lung Transplantation: Twenty-eighth Adult Lung and Heart–Lung Transplant Report—2011. J Heart Lung Transplant. 2011;30:1123–32. Excellent resource to show trends for all diagnostic groups that underwent transplantation.
Osaki S, Maloney JD, Meyer KC, et al. The impact of the lung allocation scoring system at the single national Veterans Affairs Hospital lung transplantation program. Eur J Cardiothorac Surg. 2009;36:497–501.
Meyers BF, Lynch JP, Battafarano RJ, et al. Lung transplantation is warranted for stable, ventilator-dependent recipients. Ann Thorac Surg. 2000;70:1675–8.
• Weiss ES, Allen JG, Merlo CA, et al. Lung allocation score predicts survival in lung transplantation patients with pulmonary fibrosis. Ann Thorac Surg. 2009;88:1757–64. Excellent paper looking at the role of LAS.
•• Orens JB, Estenne M, Arcasoy S, et al. International guidelines for the selection of lung transplant candidates: 2006 update—a consensus report from the Pulmonary Scientific Council of the International Society for Heart and Lung Transplantation. J Heart Lung Transplant. 2006;25:745–55. A very good resource.
Trulock EP, Christie JD, Edwards LB, et al. Registry of the International Society for Heart and Lung Transplantation: twenty-fourth official adult lung and heart-lung transplantation report—2007. J Heart Lung Transplant. 2007;26:782–95.
Enomoto N, Suda T, Kato M, et al. Quantitative analysis of fibroblastic foci in usual interstitial pneumonia. Chest. 2006;130:22–9.
Nicholson AG, Fulford LG, Colby TV, et al. The relationship between individual histologic features and disease progression in idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2002;15(166):173–7.
Travis WD, Matsui K, Moss J, Ferrans VJ. Idiopathic nonspecific interstitial pneumonia: prognostic significance of cellular and fibrosing patterns: survival comparison with usual interstitial pneumonia and desquamative interstitial pneumonia. Am J Surg Pathol. 2000;24:19–33.
Tafti SF, Mokri B, Mohammadi F, et al. Comparison of clinicoradiologic manifestation of nonspecific interstitial pneumonia and usual interstitial pneumonia/idiopathic pulmonary fibrosis: A report from NRITLD. Ann Thorac Med. 2008;3:140–5.
Lynch DA, Godwin JD, Safrin S, et al. High-resolution computed tomography in idiopathic pulmonary fibrosis: diagnosis and prognosis. Am J Respir Crit Care Med. 2005;172:488–93.
Screaton NJ, Hiorns MP, Lee KS, et al. Serial high resolution CT in non-specific interstitial pneumonia: prognostic value of the initial pattern. Clin Radiol. 2005;60:96–104.
Flaherty KR, Thwaite EL, Kazerooni EA, et al. Radiological versus histological diagnosis in UIP and NSIP: survival implications. Thorax. 2003;58:143–8.
Martinez FJ. Idiopathic interstitial pneumonias: usual interstitial pneumonia versus nonspecific interstitial pneumonia. Proc Am Thorac Soc. 2006;3:81–95.
Mogulkoc N, Brutsche M, Bishop P, et al. Pulmonary function in idiopathic pulmonary fibrosis and referral for lung transplantation. Am J Respir Crit Care Med. 2001;164:103–8.
Lynch D, Godwin J, Safrin S, Idiopathic Pulmonary Fibrosis Study Group, et al. High-resolution computed tomography in idiopathic pulmonary fibrosis: diagnosis and prognosis. Am J Respir Crit Care Med. 2005;172:488–93.
Jegal U, Kim DS, Shim TS, et al. Physiology is a stronger predictor of survival than pathology in fibrotic interstitial pneumonia. Am J Respir Crit Care Med. 2005;171:639–44.
Latsi PI, du Bois RM, Nicholson AG, et al. Fibrotic idiopathic interstitial pneumonia: the prognostic value of longitudinal functional trends. Am J Respir Crit Care Med. 2003;168:531–7.
Egan JJ, Martinez FJ, Wells AU, Williams T. Lung function estimates in idiopathic pulmonary fibrosis: the potential for a simple classification. Thorax. 2005;60:270–3.
• Bradley B, Branley HM, Egan JJ, et al. Interstitial lung disease guideline: the British Thoracic Society in collaboration with the Thoracic Society of Australia and New Zealand and the Irish Thoracic Society. Thorax. 2008;63 Suppl 5:v1–v58. Good resource for guidelines. New ones are awaited this year.
Wells AU, Desai SR, Rubens MB, et al. Idiopathic pulmonary fibrosis: a composite physiologic index derived from disease extent observed by computed tomography. Am J Respir Crit Care Med. 2003;167:962–9.
Fell CD, Liu LX, Motika C, et al. The prognostic value of cardiopulmonary exercise testing in idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2009;179:402–7.
Lama V, Flaherty K, Toews G, et al. Prognostic value of desaturation during a 6-minute walk test in idiopathic interstitial pneumonia. Am J Respir Crit Care Med. 2003;168:1084–90.
Kawut SM, O’Shea MK, Bartels MN, et al. Exercise testing determines survival in patients with diffuse parenchymal lung disease evaluated for lung transplantation. Respir Med. 2005;99:1431–9.
Swigris J, Swick J, Wamboldt F, et al. Heart Rate Recovery After 6-Minute Walk Test Predicts Survival in Patients With Idiopathic Pulmonary Fibrosis. Chest. 2009;136:814–8.
Nadrous H, Pellikka P, Krowka M, et al. Pulmonary hypertension in patients with idiopathic pulmonary fibrosis. Chest. 2005;128:2393–9.
Patel N, Lederer D, Borczuk A, Kawut S. Pulmonary hypertension in idiopathic pulmonary fibrosis. Chest. 2007;132:998–1006.
Shorr A, Wainright J, Cors C, et al. Pulmonary hypertension in patients with pulmonary fibrosis awaiting lung transplant. Eur Respir J. 2007;30:715–21.
Nathan S, Shlobin O, Ahmad S, et al. Serial development of pulmonary hypertension in patients with idiopathic pulmonary fibrosis. Respiration. 2008;76:288–94.
Lettieri C, Nathan S, Barnett S, et al. Prevalence and outcomes of pulmonary arterial hypertension in advanced idiopathic pulmonary fibrosis. Chest. 2006;129:746–52.
Hamada K, Nagai S, Tanaka S, et al. Significance of pulmonary arterial pressure and diffusion capacity of the lung as prognosticator in patients with idiopathic pulmonary fibrosis. Chest. 2007;131:650–6.
Whelan T, Dunitz J, Kelly R, et al. Effect of preoperative pulmonary artery pressure on early survival after lung transplantation for idiopathic pulmonary fibrosis. J Heart Lung Transplant. 2005;24:1269–74.
• Judge EP, Fabre A, Adamali HI, Egan JJ. Acute exacerbations and pulmonary hypertension in advanced idiopathic pulmonary fibrosis. Eur Respir J. 2012;40:93–100. Establishes pulmonary hypertension in IPF predisposes patients to acute exacerbations and decrease survival.
Culver DA, Mazzone PJ, Khandwala F, et al. Discordant utility of ideal body weight and body mass index as predictors of mortality in lung transplant recipients. J Heart Lung Transplant. 2005;24:137–44.
Madill J, Gutierrez C, Grossman J, et al. Nutritional assessment of the lung transplant patient: body mass index as a predictor of 90-day mortality following transplantation. J Heart Lung Transplant. 2001;20:288–96.
Seoane L, Arcement LM, Valentine VG, et al. Long-term survival in lung transplant recipients after successful preoperative coronary revascularization. J Thorac Cardiovasc Surg. 2005;130:538–41.
Lee R, Meyers BF, Sundt TM, et al. Concomitant coronary artery revascularization to allow successful lung transplantation in selected patients with coronary artery disease. J Thorac Cardiovasc Surg. 2002;124:1250–1.
• Nathan SD, Shlobin OA, Ahmad S, et al. Comparison of wait times and mortality for idiopathic pulmonary fibrosis patients listed for single or bilateral lung transplantation. J Heart Lung Transplant. 2010;29:1165–71. Excellent comparison of BLT and SLT in IPF.
Meyer DM, Edwards LB, Torres F, et al. Impact of recipient age and procedure type on survival after lung transplantation for pulmonary fibrosis. Ann Thorac Surg. 2005;79:950–7.
Thabut G, Christie JD, Ravaud P, et al. Survival after bilateral versus single-lung transplantation for idiopathic pulmonary fibrosis. Ann Intern Med. 2009;151:767–74.
Nocturnal Oxygen Therapy Trial Group. Continuous or nocturnal oxygen therapy in hypoxemic chronic lung disease: a clinical trial. Ann Intern Med. 1980;93:391–8.
Medical Research Council Working Party. Long-term domiciliary oxygen therapy in chronic hypoxic cor pulmonale complicating chronic bronchitis and emphysema. Lancet. 1981;1:681–6.
• Ahmedzai S, Balfour-Lynn IM, Bewick T, et al. Managing passengers with stable respiratory disease planning air travel: British Thoracic Society recommendations. Thorax. 2011;66 Suppl 1:i1-30. Excellent guidelines for managing respiratory patients who want to fly.
Nici L, Donner C, ZuWallack R, et al. American Thoracic Society and the European Respiratory Society statement on pulmonary rehabilitation. Am J Resp Crit Care Med. 2006;173:1390–413.
Ries AL, Bauldoff GS, Carlin BW, et al. Pulmonary Rehabilitation: Joint ACCP/AACVPR Evidence-Based Clinical Practice Guidelines. Chest. 2007;131:4–42S.
Nishiyama O, Kondoh Y, Kimura T, et al. Effects of pulmonary rehabilitation in patients with idiopathic pulmonary fibrosis. Respirology. 2008;13(3):394–9.
Holland AE, Hill CJ, Conron M, et al. Short term improvement in exercise capacity and symptoms following exercise training in interstitial lung disease. Thorax. 2008;63:549–54.
• Kozu R, Senjyu H, Jenkins S, et al. Differences in Response to Pulmonary Rehabilitation in Idiopathic Pulmonary Fibrosis and Chronic Obstructive Pulmonary Disease. Respiration. 2011;81:196–205. First prospective controlled trail to compare the benefit of PR in IPF and COPD.
• Salhi B, Troosters T, Behaegel M, et al. Effects of pulmonary rehabilitation in patients with restrictive lung diseases. Chest. 2010;137:273–9. This paper showed sustained improvement in ILD.
• Holland AE. Exercise limitation in interstitial lung disease: mechanisms, significance and therapeutic options. Chron Respir Dis. 2010;7:101–11. Very interesting data to look at different mechanisms of exercise limitations.
Nishiyama O, Taniguchi H, Kondoh Y, et al. Quadriceps weakness is related to exercise capacity in idiopathic pulmonary fibrosis. Chest. 2005;127:2028–33.
Minton O, Richardson A, Sharpe M, et al. Drug therapy for the management of cancer-related fatigue. Cochrane Database Systematic Review. 2010;7(7):CD006704.
• Swigris JJ, Fairclough DL, Morrison M, et al. Benefits of Pulmonary Rehabilitation in Idiopathic Pulmonary Fibrosis. Respir Care. 2011;56(6):783–9. A 6 week pilot study showing improvements in functional capacity and fatigue.
Ferreira A, Garvey C, Connors GL, et al. Pulmonary rehabilitation in interstitial lung disease: benefits and predictors of response. Chest. 2009;135:442–7. The most robust trial to look at the predictors of benefit in IPF.
Holland AE, Hill C, Glaspole I, et al. Predictors of benefit following pulmonary rehabilitation for interstitial lung disease. Respir Med. 2012;106(3):429–35.
• Kozu R, Jenkins S, Senjyu H, et al. Effect of disability level on response to pulmonary rehabilitation in patients with idiopathic pulmonary fibrosis. Respiration. 2011;16:1196–202. Establishes that patients with less symptomatic disease benefit from PR..
World Health Organization: WHO Definition of Palliative Care—2005. http://who.int/cancer/palliative/definition/en/print.html
Thomas K. Caring for the dying at home-Companions on the journey. Oxford: Radcliffe Medical Press; 2003.
• Department of Heath: Advance care planning: a guide for health and social care staff. http://www.endoflifecareforadults.nhs.uk/ Excellent resource for end of life care programs.
• Tomoas K: The gold standards framework. Advance care planning. http:www.goldstandardsframework.org.uk/AdvanceCarePlanning Excellent resource for advance care planning.
Mallick S. Outcome of patients with idiopathic pulmonary fibrosis. Respir Med. 2008;102:1355–9.
Stern JB, Mal H, Groussard O, et al. Prognosis of patients with advanced idiopathic pulmonary fibrosis requiring mechanical ventilation for acute respiratory failure. Chest. 2001;120:213–9.
Blivet S, Philit F, Sab JM, et al. Outcome of patients with idiopathic pulmonary fibrosis admitted to the ICU for respiratory failure. Chest. 2001;120:209–12.
Saydain G, Islam A, Afessa B, et al. Outcome of patients with idiopathic pulmonary fibrosis admitted to the intensive care unit. Am J Respir Crit Care Med. 2002;166:839–42.
De Vries J, Kessels BLJ, Drent M. Quality of life of idiopathic pulmonary fibrosis patients. Eur Respir J. 2001;17:954–61.
Hope-Gill BDM, Hilldrup S, Davies C. A study of the cough reflex in idiopathic pulmonary fibrosis. Am J Respir Crit Care. 2003;168:995–1002.
• Yorke J, Jones PW, Swigris JJ. Development & Validity Testing of an IPF-specific version of the St George’s Respiratory Questionnaire. Thorax. 2010;65:921–6. Adaptation of a HRQoL tool for specific use in IPF patients.
Mahler D, Weinberg D, Wells C, Feinstein A. The measurement of dyspnoea: contents, inter-observer agreement and physiological correlates of two clinical indexes. Chest. 1984;85:751–8.
• Nishiyama O, Taniguchi H, Kondoh Y, et al. A simple assessment of dyspnoea as a prognostic indicator in idiopathic pulmonary fibrosis. Eur Respir J. 2010;36:1067-72. Establishes the MRC Dyspnoea score as a robust tool.
• Key AL, Holt K, Hamilton A, et al. Objective Cough Frequency in Idiopathic Pulmonary Fibrosis. Cough. 2010;6:4. A good paper that establishes cough as a distressing symptom and patients perception of cough frequency as accurate.
Allen S, Raut S, Woollard J, Vassallo M. Low dose diamorphine reduces breathlessness without causing a fall in oxygen saturation in elderly patients with end-stage idiopathic pulmonary fibrosis. Palliat Med. 2005;19:128–30.
Horton MR, Danoff SK, Lechtzin N. Thalidomide inhibits the intractable cough of idiopathic pulmonary fibrosis. Thorax. 2008;63:749.
• Horton MR, Santopeitro V, Matthew L, et al. Thalidomide for the treatment of cough in idiopathic pulmonary fibrosis. Ann Intern Med. 2012;157:398–406. A promising therapy for a troublesome symptom that is being put through the rigors of clinical trial.
Bausewein C, Farquhar M, Booth S, et al. Measurement of breathlessness in advanced disease: A systematic review. Respir Med. 2007;101:399–410.
Edmonds P, Karlsen S, Khan S, Addington-Hall J. A comparison of the palliative care needs of patients dying from chronic respiratory diseases and lung cancer. Palliat Med. 2001;15:287–95.
Disclosure
No potential conflicts of interest relevant to this article were reported.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Adamali, H.I., Anwar, M.S., Russell, AM. et al. Non-pharmacological treatment of idiopathic pulmonary fibrosis. Curr Respir Care Rep 1, 208–215 (2012). https://doi.org/10.1007/s13665-012-0031-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13665-012-0031-z