Abstract
Purpose
Hematopoietic PBX interacting protein (HPIP), a scaffold protein, is known to regulate the proliferation, migration and invasion in different cancer cell types. The aim of this study was to assess the role of HPIP in ovarian cancer cell migration, invasion and epithelial-mesenchymal transition (EMT), and to unravel the mechanism by which it regulates these processes.
Methods
HPIP expression was assessed by immunohistochemistry of tissue microarrays containing primary ovarian tumor samples of different grades. OAW42, an ovarian carcinoma-derived cell line exhibiting a high HPIP expression, was used to study the role of HPIP in cell migration, invasion and EMT. HPIP knockdown in these cells was achieved using a small hairpin RNA (shRNA) approach. Cell migration and invasion were assessed using scratch wound and transwell invasion assays, respectively. The extent of EMT was assessed by determining the expression levels of Snail, Vimentin and E-cadherin using Western blotting. The effect of HPIP expression on AKT and MAPK activation was also investigated by Western blotting. Cell viabilities in response to cisplatin treatment were assessed using a MTT assay, whereas apoptosis was assessed by determining caspase-3 and PARP cleavage in ovarian carcinoma-derived SKOV3 cells.
Results
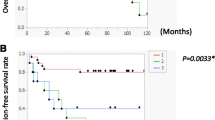
We found that HPIP is highly expressed in high-grade primary ovarian tumors. In addition, we found that HPIP promotes the migration, invasion and EMT in OAW42 cells and induces EMT in these cells via activation of the PI3K/AKT pathway. The latter was found to lead to stabilization of the Snail protein and to repression of E-cadherin expression through inactivation of GSK-3β. We also found that HPIP expression confers cisplatin resistance to SKOV3 cells after prolonged exposure and that its subsequent knockdown decreases the viability of these cells and increases caspase-3 activation and PARP proteolysis in these cells following cisplatin treatment.
Conclusions
From these results we conclude that HPIP expression is associated with high-grade ovarian tumors and may promote their migration, invasion and EMT, a process that is associated with metastasis. In addition, we conclude that HPIP may serve as a potential therapeutic target for cisplatin resistant ovarian tumors.





Similar content being viewed by others
Abbreviations
- HPIP/PBXIP1:
-
Hematopoietic PBX interacting protein/ pre B-cell leukemia homeobox interacting protein
- EMT:
-
Epithelial-mesenchymal transition
- GSK-3β:
-
Glycogen synthase kinase-3β
- PI3K:
-
Phosphatidylinositol 3-kinase
- MAPK:
-
Mitogen-activated protein kinase
- ERK½:
-
Extracellular signal-regulated kinase ½
- OCC:
-
Ovarian cystadenocarcinoma
References
R.P. Perez, A.K. Godwin, T.C. Hamilton, R.F. Ozols, Ovarian cancer biology. Semin Oncol 18, 186–204 (1991)
K.R. Cho, M. Shih Ie, Ovarian cancer. Ann Rev Pathol 4, 287–313 (2009). doi:10.1146/annurev.pathol.4.110807.092246
T.A. Yap, C.P. Carden, S.B. Kaye, Beyond chemotherapy: targeted therapies in ovarian cancer. Nat Rev Cancer 9, 167–181 (2009). doi:10.1038/nrc2583
N. Colombo, T. Van Gorp, G. Parma, F. Amant, G. Gatta, C. Sessa, I. Vergote, Ovarian cancer. Crit Rev Oncol Hematol 60, 159–179 (2006). doi:10.1016/j.critrevonc.2006.03.004
S. Patel, L. Kumar, N. Singh, Metformin and epithelial ovarian cancer therapeutics. Cell Oncol 38, 365–375 (2015). doi:10.1007/s13402-015-0235-7
M. Zou, X. Zhang, C. Xu, IL6-induced metastasis modulators p-STAT3, MMP-2 and MMP-9 are targets of 3,3'-diindolylmethane in ovarian cancer cells. Cell Oncol 39, 47–57 (2016). doi:10.1007/s13402-015-0251-7
R.C. Bast Jr., B. Hennessy, G.B. Mills, The biology of ovarian cancer: new opportunities for translation. Nat Rev Cancer 9, 415–428 (2009). doi:10.1038/nrc2644
H. Naora, D.J. Montell, Ovarian cancer metastasis: integrating insights from disparate model organisms. Nat Rev Cancer 5, 355–366 (2005). doi:10.1038/nrc1611
J. Mikula-Pietrasik, P. Uruski, K. Matuszkiewicz, S. Szubert, R. Moszynski, D. Szpurek, S. Sajdak, A. Tykarski, K. Ksiazek, Ovarian cancer-derived ascitic fluids induce a senescence-dependent pro-cancerogenic phenotype in normal peritoneal mesothelial cells. Cell Oncol 39, 473–481 (2016). doi:10.1007/s13402-016-0289-1
Y. Kuwabara, T. Yamada, K. Yamazaki, W.L. Du, K. Banno, D. Aoki, M. Sakamoto, Establishment of an ovarian metastasis model and possible involvement of E-cadherin down-regulation in the metastasis. Cancer Sci 99, 1933–1939 (2008). doi:10.1111/j.1349-7006.2008.00946.x
D. Vergara, B. Merlot, J.P. Lucot, P. Collinet, D. Vinatier, I. Fournier, M. Salzet, Epithelial-mesenchymal transition in ovarian cancer. Cancer Lett 291, 59–66 (2010). doi:10.1016/j.canlet.2009.09.017
B.T. Hennessy, D.L. Smith, P.T. Ram, Y. Lu, G.B. Mills, Exploiting the PI3K/AKT pathway for cancer drug discovery. Nat Rev Drug Discov 4, 988–1004 (2005). doi:10.1038/nrd1902
I. Vivanco, C.L. Sawyers, The phosphatidylinositol 3-kinase AKT pathway in human cancer. Nat Rev Cancer 2, 489–501 (2002). doi:10.1038/nrc839
B. Manavathi, F. Acconcia, S.K. Rayala, R. Kumar, An inherent role of microtubule network in the action of nuclear receptor. Proc Natl Acad Sci U S A 103, 15981–15986 (2006). doi:10.1073/pnas.0607445103
X. Xu, Z. Fan, L. Kang, J. Han, C. Jiang, X. Zheng, Z. Zhu, H. Jiao, J. Lin, K. Jiang, L. Ding, H. Zhang, L. Cheng, H. Fu, Y. Song, Y. Jiang, J. Liu, R. Wang, N. Du, Q. Ye, Hepatitis B virus X protein represses miRNA-148a to enhance tumorigenesis. J Clin Invest 123, 630–645 (2013). doi:10.1172/JCI64265
S. Bugide, D. David, A. Nair, N. Kannan, V.S. Samanthapudi, J. Prabhakar, B. Manavathi, Hematopoietic PBX-interacting protein (HPIP) is over expressed in breast infiltrative ductal carcinoma and regulates cell adhesion and migration through modulation of focal adhesion dynamics. Oncogene 34, 4601–4612 (2015). doi:10.1038/onc.2014.389
Y. Feng, X. Xu, Y. Zhang, J. Ding, Y. Wang, X. Zhang, Z. Wu, L. Kang, Y. Liang, L. Zhou, S. Song, K. Zhao, Q. Ye, HPIP is upregulated in colorectal cancer and regulates colorectal cancer cell proliferation, apoptosis and invasion. Sci Rep 5, 9429 (2015). doi:10.1038/srep09429
Y. Feng, L. Li, X. Zhang, Y. Zhang, Y. Liang, J. Lv, Z. Fan, J. Guo, T. Hong, B. Ji, Q. Ji, G. Mei, L. Ding, S. Zhang, X. Xu, Q. Ye, HPIP is overexpressed in gastric cancer and promotes gastric cancer cell proliferation, migration and invasion. Cancer Sci 106, 1313–1322 (2015). doi:10.1111/cas.12754
J. Pan, Y. Qin, M. Zhang, HPIP promotes non-small cell lung cancer cell proliferation, migration and invasion through regulation of the sonic hedgehog signaling pathway. Biomed Pharmacother 77, 176–181 (2016). doi:10.1016/j.biopha.2015.12.012
S. Okada, T. Irie, J. Tanaka, R. Yasuhara, G. Yamamoto, T. Isobe, C. Hokazono, T. Tachikawa, Y. Kohno, K. Mishima, Potential role of hematopoietic pre-B-cell leukemia transcription factor-interacting protein in oral carcinogenesis. J Oral Pathol Med 44, 115–125 (2015). doi:10.1111/jop.12210
S.C. Wang, D.S. Chai, C.B. Chen, Z.Y. Wang, L. Wang, HPIP promotes thyroid cancer cell growth, migration and EMT through activating PI3K/AKT signaling pathway. Biomed Pharmacother 75, 33–39 (2015). doi:10.1016/j.biopha.2015.08.027
D.G. van Vuurden, E. Aronica, E. Hulleman, L.E. Wedekind, D. Biesmans, A. Malekzadeh, M. Bugiani, D. Geerts, D.P. Noske, W.P. Vandertop, G.J. Kaspers, J. Cloos, T. Wurdinger, P.P. van der Stoop, Pre-B-cell leukemia homeobox interacting protein 1 is overexpressed in astrocytoma and promotes tumor cell growth and migration. Neuro-Oncology 16, 946–959 (2014). doi:10.1093/neuonc/not308
K. Shostak, F. Patrascu, S.I. Goktuna, P. Close, L. Borgs, L. Nguyen, F. Olivier, A. Rammal, H. Brinkhaus, M. Bentires-Alj, J.C. Marine, A. Chariot, MDM2 restrains estrogen-mediated AKT activation by promoting TBK1-dependent HPIP degradation. Cell Death Differ 21, 811–824 (2014). doi:10.1038/cdd.2014.2
V.N. Gajulapalli, V.S. Samanthapudi, M. Pulaganti, S.S. Khumukcham, V.L. Malisetty, L. Guruprasad, S.K. Chitta, B. Manavathi, A transcriptional repressive role for epithelial-specific ETS factor ELF3 on oestrogen receptor alpha in breast cancer cells. Biochem J 473, 1047–1061 (2016). doi:10.1042/BCJ20160019
G.R. Sareddy, B.C. Nair, S.K. Krishnan, V.K. Gonugunta, Q.G. Zhang, T. Suzuki, N. Miyata, A.J. Brenner, D.W. Brann, R.K. Vadlamudi, KDM1 is a novel therapeutic target for the treatment of gliomas. Oncotarget 4, 18–28 (2013). doi:10.18632/oncotarget.725
T. Bonome, D.A. Levine, J. Shih, M. Randonovich, C.A. Pise-Masison, F. Bogomolniy, L. Ozbun, J. Brady, J.C. Barrett, J. Boyd, M.J. Birrer, A gene signature predicting for survival in suboptimally debulked patients with ovarian cancer. Cancer Res 68, 5478–5486 (2008). doi:10.1158/0008-5472.CAN-07-6595
R. Kalluri, R.A. Weinberg, The basics of epithelial-mesenchymal transition. J Clin Invest 119, 1420–1428 (2009). doi:10.1172/JCI39104
C.L. Chaffer, R.A. Weinberg, A perspective on cancer cell metastasis. Science 331, 1559–1564 (2011). doi:10.1126/science.1203543
E. Batlle, E. Sancho, C. Franci, D. Dominguez, M. Monfar, J. Baulida, A. Garcia De Herreros, The transcription factor snail is a repressor of E-cadherin gene expression in epithelial tumour cells. Nat Cell Biol 2, 84–89 (2000). doi:10.1038/35000034
J.P. Thiery, H. Acloque, R.Y. Huang, M.A. Nieto, Epithelial-mesenchymal transitions in development and disease. Cell 139, 871–890 (2009). doi:10.1016/j.cell.2009.11.007
B.P. Zhou, J. Deng, W. Xia, J. Xu, Y.M. Li, M. Gunduz, M.C. Hung, Dual regulation of snail by GSK-3beta-mediated phosphorylation in control of epithelial-mesenchymal transition. Nat Cell Biol 6, 931–940 (2004). doi:10.1038/ncb1173
D.A. Cross, D.R. Alessi, P. Cohen, M. Andjelkovich, B.A. Hemmings, Inhibition of glycogen synthase kinase-3 by insulin mediated by protein kinase B. Nature 378, 785–789 (1995). doi:10.1038/378785a0
A. Cano, M.A. Perez-Moreno, I. Rodrigo, A. Locascio, M.J. Blanco, M.G. del Barrio, F. Portillo, M.A. Nieto, The transcription factor snail controls epithelial-mesenchymal transitions by repressing E-cadherin expression. Nat Cell Biol 2, 76–83 (2000). doi:10.1038/35000025
S. Lee, E.J. Choi, C. Jin, D.H. Kim, Activation of PI3K/Akt pathway by PTEN reduction and PIK3CA mRNA amplification contributes to cisplatin resistance in an ovarian cancer cell line. Gynecol Oncol 97, 26–34 (2005). doi:10.1016/j.ygyno.2004.11.051
H. Asechi, E. Hatano, T. Nitta, M. Tada, K. Iwaisako, N. Tamaki, H. Nagata, M. Narita, A. Yanagida, I. Ikai, S. Uemoto, Resistance to cisplatin-induced apoptosis via PI3K-dependent survivin expression in a rat hepatoma cell line. Int J Oncol 37, 89–96 (2010)
E. Lengyel, Ovarian cancer development and metastasis. Am J Pathol 177, 1053–1064 (2010). doi:10.2353/ajpath.2010.100105
R.J. Kurman, M. Shih Ie, Molecular pathogenesis and extraovarian origin of epithelial ovarian cancer--shifting the paradigm. Hum Pathol 42, 918–931 (2011). doi:10.1016/j.humpath.2011.03.003
J.L. Brun, A. Feyler, G. Chene, J. Saurel, G. Brun, C. Hocke, Long-term results and prognostic factors in patients with epithelial ovarian cancer. Gynecol Oncol 78, 21–27 (2000). doi:10.1006/gyno.2000.5805
R.G. Verhaak, P. Tamayo, J.Y. Yang, D. Hubbard, H. Zhang, C.J. Creighton, S. Fereday, M. Lawrence, S.L. Carter, C.H. Mermel, A.D. Kostic, D. Etemadmoghadam, G. Saksena, K. Cibulskis, S. Duraisamy, K. Levanon, C. Sougnez, A. Tsherniak, S. Gomez, R. Onofrio, S. Gabriel, L. Chin, N. Zhang, P.T. Spellman, Y. Zhang, R. Akbani, K.A. Hoadley, A. Kahn, M. Kobel, D. Huntsman, R.A. Soslow, A. Defazio, M.J. Birrer, J.W. Gray, J.N. Weinstein, D.D. Bowtell, R. Drapkin, J.P. Mesirov, G. Getz, D.A. Levine, M. Meyerson, Cancer genome atlas research, Prognostically relevant gene signatures of high-grade serous ovarian carcinoma. J Clin Invest 123, 517–525 (2013). doi:10.1172/JCI65833
M. Osaki, M. Oshimura, H. Ito, PI3K-Akt pathway: its functions and alterations in human cancer. Apoptosis 9, 667–676 (2004). doi:10.1023/B:APPT.0000045801.15585.dd
D.A. Altomare, H.Q. Wang, K.L. Skele, A. De Rienzo, A.J. Klein-Szanto, A.K. Godwin, J.R. Testa, AKT and mTOR phosphorylation is frequently detected in ovarian cancer and can be targeted to disrupt ovarian tumor cell growth. Oncogene 23, 5853–5857 (2004). doi:10.1038/sj.onc.1207721
A.J. Hanrahan, N. Schultz, M.L. Westfal, R.A. Sakr, D.D. Giri, S. Scarperi, M. Janakiraman, N. Olvera, E.V. Stevens, Q.B. She, C. Aghajanian, T.A. King, E. Stanchina, D.R. Spriggs, A. Heguy, B.S. Taylor, C. Sander, N. Rosen, D.A. Levine, D.B. Solit, Genomic complexity and AKT dependence in serous ovarian cancer. Cancer Discov 2, 56–67 (2012). doi:10.1158/2159-8290.CD-11-0170
K. Kurose, X.P. Zhou, T. Araki, S.A. Cannistra, E.R. Maher, C. Eng, Frequent loss of PTEN expression is linked to elevated phosphorylated Akt levels, but not associated with p27 and cyclin D1 expression, in primary epithelial ovarian carcinomas. Am J Pathol 158, 2097–2106 (2001). doi:10.1016/S0002-9440(10)64681-0
M. Sun, G. Wang, J.E. Paciga, R.I. Feldman, Z.Q. Yuan, X.L. Ma, S.A. Shelley, R. Jove, P.N. Tsichlis, S.V. Nicosia, J.Q. Cheng, AKT1/PKBalpha kinase is frequently elevated in human cancers and its constitutive activation is required for oncogenic transformation in NIH3T3 cells. Am J Pathol 159, 431–437 (2001)
Z.Q. Yuan, M. Sun, R.I. Feldman, G. Wang, X. Ma, C. Jiang, D. Coppola, S.V. Nicosia, J.Q. Cheng, Frequent activation of AKT2 and induction of apoptosis by inhibition of phosphoinositide-3-OH kinase/Akt pathway in human ovarian cancer. Oncogene 19, 2324–2330 (2000). doi:10.1038/sj.onc.1203598
L. Shayesteh, Y. Lu, W.L. Kuo, R. Baldocchi, T. Godfrey, C. Collins, D. Pinkel, B. Powell, G.B. Mills, J.W. Gray, PIK3CA is implicated as an oncogene in ovarian cancer. Nat Genet 21, 99–102 (1999). doi:10.1038/5042
K.E. Sheppard, C. Cullinane, K.M. Hannan, M. Wall, J. Chan, F. Barber, J. Foo, D. Cameron, A. Neilsen, P. Ng, J. Ellul, M. Kleinschmidt, K.M. Kinross, D.D. Bowtell, J.G. Christensen, R.J. Hicks, R.W. Johnstone, G.A. McArthur, R.D. Hannan, W.A. Phillips, R.B. Pearson, Synergistic inhibition of ovarian cancer cell growth by combining selective PI3K/mTOR and RAS/ERK pathway inhibitors. Eur J Cancer 49, 3936–3944 (2013). doi:10.1016/j.ejca.2013.08.007
N. Cancer, Genome atlas research, integrated genomic analyses of ovarian carcinoma. Nature 474, 609–615 (2011). doi:10.1038/nature10166
V. Auner, G. Kriegshauser, D. Tong, R. Horvat, A. Reinthaller, A. Mustea, R. Zeillinger, KRAS mutation analysis in ovarian samples using a high sensitivity biochip assay. BMC Cancer 9, 111 (2009). doi:10.1186/1471-2407-9-111
G. Singer, R. Oldt 3rd, Y. Cohen, B.G. Wang, D. Sidransky, R.J. Kurman, M. Shih Ie, Mutations in BRAF and KRAS characterize the development of low-grade ovarian serous carcinoma. J Natl Cancer Inst 95, 484–486 (2003)
A. Bagnato, L. Rosano, Epithelial-mesenchymal transition in ovarian cancer progression: a crucial role for the endothelin axis. Cells Tissues Organs 185, 85–94 (2007). doi:10.1159/000101307
Y. Yang, J. Zhang, Y. Zhu, Z. Zhang, H. Sun, Y. Feng, Follicle-stimulating hormone induced epithelial-mesenchymal transition of epithelial ovarian cancer cells through follicle-stimulating hormone receptor PI3K/Akt-snail signaling pathway. Int J Gynecol Cancer 24, 1564–1574 (2014). doi:10.1097/IGC.0000000000000279
G.Y. Zhang, A.H. Liu, G.M. Li, J.R. Wang, HPIP silencing prevents epithelial-mesenchymal transition induced by TGF-beta1 in human ovarian cancer cells. Oncol Res 24, 33–39 (2016). doi:10.3727/096504016X14575597858654
L. Galluzzi, L. Senovilla, I. Vitale, J. Michels, I. Martins, O. Kepp, M. Castedo, G. Kroemer, Molecular mechanisms of cisplatin resistance. Oncogene 31, 1869–1883 (2012). doi:10.1038/onc.2011.384
J. Chien, R. Kuang, C. Landen, V. Shridhar, Platinum-sensitive recurrence in ovarian cancer: the role of tumor microenvironment. Front Oncol 3, 251 (2013). doi:10.3389/fonc.2013.00251
Y. Zhang, C. Bao, Q. Mu, J. Chen, J. Wang, Y. Mi, A.J. Sayari, Y. Chen, M. Guo, Reversal of cisplatin resistance by inhibiting PI3K/Akt signal pathway in human lung cancer cells. Neoplasma 63, 362–370 (2016). doi:10.4149/304_150806N433
C.F. Hu, Y.Y. Huang, Y.J. Wang, F.G. Gao, Upregulation of ABCG2 via the PI3K-Akt pathway contributes to acidic microenvironment-induced cisplatin resistance in A549 and LTEP-a-2 lung cancer cells. Oncol Rep 36, 455–461 (2016). doi:10.3892/or.2016.4827
Acknowledgments
This work was supported by the Department of Biotechnology (DBT), India grants No- BT/MED/30/SP11273/2015; BT/PR8764/MED/97/104/2013, BT/PR7672/BRB/10/1173/2013, BT/01/IYBA/2009 (to BM), and the Department of Science and Technology (DST) grant No- SB/SO/BB/013/2013, India (to BM). We acknowledge DST-PURSE, UOH-DBT-CREBB, UGC-UPE2, UGC-DRS and DST-FIST for providing the research facilities at the University of Hyderabad. The authors thank Prof. Nagini Siddavaram, Annamalai University, India for critical reviewing and editing the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest to disclose.
Additional information
Vijay Kumar Gonugunta and Vasudevarao Penugurti contributed equally to this work
Electronic supplementary material
Figure S1
Analysis of HPIP expression in ovarian cancer data obtained from Oncomine database. a. HPIP expression in Borderline Ovarian Serous Neoplasm (10) and Ovarian Serous Adenocarcinoma p < 0.0001(13) (Ref: Gilks et al., 2005; Gynecol Oncol; 2005/03/01) b. HPIP expression in Breast Carcinoma (44), Ovarian Adenocarcinoma (3), Ovarian Brenner Tumor (1), Ovarian Carcinosarcoma (2), Ovarian Clear Cell Adenocarcinoma (6), Ovarian Endometrioid Adenocarcinoma (6), Ovarian Mucinous Adenocarcinoma (7) and Ovarian Serous Adenocarcinoma (71); p < 0.001 (Meyniel et al., 2010; BMC Cancer; 2010/05/21 ). c. HPIP expression in Ovarian Adenocarcinoma (16), Ovarian Clear Cell Adenocarcinoma (3), Ovarian Endometrioid Adenocarcinoma (5),Mixed Ovarian Adenocarcinoma (2) and Ovarian Serous Adenocarcinoma (35); p < 0.0001 (J Natl Cancer Inst; 2002/07/03) d. HPIP expression in Ovarian Clear Cell Adenocarcinoma (8), Ovarian Endometrioid Adenocarcinoma (33), Malignant Ovarian Mixed Epithelial Tumor (9), Ovarian Mucinous Adenocarcinoma (10) and Ovarian Serous Adenocarcinoma (53); p < 0.0001 (Schwartz et al., 2001; Cancer Res; 2002/08/15). (PPTX 110 kb)
Figure S2
HPIP knockdown sensitizes PA-1 cells to cisplatin-induced cell death. a PA-1 cells were cisplatin (0.5 μg/ml) treated for 3 weeks and cisplatin-resistant cells were subjected to Western blotting as indicated. b PA-1 cells were transfected with either control shRNA or HPIP shRNA and treated with cisplatin at various concentrations for 24 h and cell viability was measured by MTT assay. IC50 values were calculated using Sigma plot. Inset, Western blot analysis demonstrating efficient knock down of HPIP in PA-1 cells. c PA-1 cells were transfected with either control shRNA or HPIP shRNA and treated with cisplatin for 24 h and cell lysates were subjected to Western blotting as indicated. (PPTX 1437 kb)
Table S1
Immunohistochemical scores of human ovarian tissue microarrays (hoTMAs). (XLSX 10 kb)
Table S2
Various grades of ovarian tumors used for HPIP expression (XLSX 16 kb)
Rights and permissions
About this article
Cite this article
Bugide, S., Gonugunta, V.K., Penugurti, V. et al. HPIP promotes epithelial-mesenchymal transition and cisplatin resistance in ovarian cancer cells through PI3K/AKT pathway activation. Cell Oncol. 40, 133–144 (2017). https://doi.org/10.1007/s13402-016-0308-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13402-016-0308-2