Abstract
Introduction
iGlarLixi is a titratable, fixed-ratio combination of insulin glargine (100 units/mL) and lixisenatide (33 μg/mL). This review evaluates the overall safety and adverse event (AE) profile of iGlarLixi in patients with type 2 diabetes.
Methods
We collated patient-level data from the phase 2 LixiLan proof-of-concept trial and the phase 3 LixiLan-L (insulin-experienced patients) and LixiLan-O (insulin-naïve patients) trials to evaluate AEs associated with iGlarLixi. We also describe data from the ELIXA study to examine pancreatitis and pancreatic cancer, and the ELIXA and ORIGIN studies for cardiovascular safety data.
Results
Patients treated with iGlarLixi had improved glycemic control with a similar incidence of documented symptomatic hypoglycemia (plasma glucose ≤ 70 mg/dL) compared with iGlar. Incidence of severe hypoglycemia (an event requiring third-party assistance) was low in all treatment arms in both LixiLan-L and LixiLan-O. Rates of gastrointestinal AEs in patients treated with iGlarLixi tended to be lower compared with lixisenatide alone, but higher than those treated with iGlar alone. Gastrointestinal AEs were generally mild to moderate in intensity and transient. Antibodies formed in response to iGlarLixi did not have any significant clinical impact, with similar safety observed for antibody-positive and antibody-negative populations. Rates of allergic reactions, malignancy, renal impairment, and cardiovascular events were low and comparable between treatment groups. Older age (≥ 65 years) and gender did not affect efficacy or safety.
Conclusion
iGlarLixi has a safety profile that is consistent with that of its two active components insulin glargine and lixisenatide, with no signals for pancreatitis or thyroid C cell tumors, and no black-box warning for iGlarLixi. There were no unexpected safety findings; iGlarLixi had beneficial effects on glycemic control, with no increased risk of hypoglycemia, despite a greater glycated hemoglobin A1c reduction. In addition, there were also fewer gastrointestinal AEs associated with iGlarLixi compared with lixisenatide alone.
Funding
Sanofi US Inc.
Similar content being viewed by others
Introduction
The addition of a glucagon-like peptide-1 receptor agonist (GLP-1 RA) to basal insulin in patients with type 2 diabetes (T2D) who are unable to achieve and/or sustain adequate control of glycated hemoglobin A1c (A1C) is an important treatment option. Treatment with a GLP-1 RA and basal insulin has a favorable adverse event (AE) profile and comparable A1C reduction, with lower rates of documented symptomatic hypoglycemia (plasma glucose ≤ 70 mg/dL) and greater weight loss compared with treatment intensification with prandial insulin [1,2,3,4,5,6,7]. Real-world evidence has shown that escalation of therapy beyond basal insulin often takes a median time of 3.7 years, and only occurs in 31% of eligible patients [8]. In addition, if patients have not achieved a glycemic target of less than 7.0% at 12 months on basal insulin, the conditional probability of achieving glycemic goals thereafter drops substantially [9]. The American Diabetes Association/European Association for the Study of Diabetes guidelines suggest that when basal insulin is insufficient to achieve control in T2D patients, GLP-1 RAs and rapid-acting insulins are the agents most commonly added to achieve glycemic control [5]. Typically, as treatment regimens become more complex, there is increased potential for drug-specific side effects to occur. This, combined with patient fears of weight gain, hypoglycemia, increased injection burden, and associated pain, often leads to failure to intensify therapy, treatment non-adherence, and glycemic targets not being reached [10, 11]. These factors may be addressed with the use of titratable fixed-ratio combinations (FRCs), as the complications associated with use of the individual components can be minimized [12].
iGlarLixi (Soliqua 100/33®/Suliqua®) is a titratable FRC of insulin glargine 100 units/mL (Lantus® [referred to as insulin glargine in the remainder of this paper]) and the GLP-1 RA lixisenatide (33 μg/mL; Adlyxin®/Lyxumia®) [13,14,15], delivered as a once-daily subcutaneous injection, which was approved for use in the USA (Soliqua 100/33®) in November 2016 and in Europe (Suliqua®) in January 2017 [15,16,17]. The safety of the two individual components is well established in T2D. The landmark ORIGIN trial showed that insulin glargine does not influence the occurrence of cardiovascular events and only resulted in a small number of hypoglycemia episodes and slight weight gain [18]. Similarly, the ELIXA trial found that the addition of lixisenatide to usual care in patients with T2D and acute coronary syndrome within 180 days of an event had a neutral effect on cardiovascular outcomes, with no difference in the rates of serious AEs or severe hypoglycemia compared with placebo [19].
This review discusses the safety profile and AEs associated with iGlarLixi and the individual components in the FRC using data reported in key clinical cardiovascular outcome trials, such as ORIGIN and ELIXA.
iGlarLixi Clinical Development Program
The rationale for combining insulin glargine and lixisenatide in the same titratable FRC lies in their complementary mechanisms of action. According to DeFronzo et al., the combination of insulin and a GLP-1 RA targets seven of the eight pathophysiologic defects which lead to hyperglycemia [20]. Insulin glargine primarily reduces hepatic glucose production and increases glucose uptake in skeletal muscle and adipose tissues, lowering fasting plasma glucose levels. Lixisenatide primarily acts through a delay in gastric emptying; it increases glucose-dependent insulin secretion and decreases glucagon, which results in reduced prandial glycemic excursion [5, 21, 22]. The complementary actions of both agents are summarized in Fig. 1 [23]. The most common AE associated with insulin glargine is hypoglycemia, while those most commonly associated AEs with lixisenatide are gastrointestinal (GI)-related [24,25,26], with other events less commonly related.

Adapted from Rosenstock et al. [23]
iGlarLixi combines the complementary actions of insulin glargine (which targets fasting plasma glucose) and lixisenatide (which targets postprandial glucose).
The efficacy and safety of iGlarLixi was first demonstrated in a phase 2, 24-week, randomized, open-label, active-controlled, proof-of-concept study [23], which compared the combination of insulin glargine and lixisenatide with insulin glargine in insulin-naïve adults with T2D inadequately controlled on metformin. The combination consisted of insulin glargine and lixisenatide in a 2:1 ratio (at a maximum dose of insulin glargine 60 units/day and lixisenatide 30 µg/day) compared with insulin glargine alone with no upper limit on the dose of insulin glargine. In this study, iGlarLixi significantly reduced A1C to a greater extent compared with insulin glargine alone, with comparable rates of hypoglycemia and significant weight loss. Two subsequent open-label, randomized, parallel-group, multicenter, phase 3 trials, LixiLan-L [14] and LixiLan-O [13], further demonstrated the efficacy and safety of iGlarLixi. In these trials, the maximum dose of insulin glargine was capped to 60 units/day, with the insulin glargine to lixisenatide ratios being either 2:1 (Pen A) or 3:1 (Pen B). The primary efficacy endpoint was change in A1C from baseline to week 30 in both trials. Both trials also had a run-in period, either optimizing the glargine dose (LixiLan-L) or metformin dose (LixiLan-O), prior to randomization. LixiLan-L compared iGlarLixi with insulin glargine in patients inadequately controlled on basal insulin with or without up to two oral antidiabetes drugs (OADs). In LixiLan-L, iGlarLixi showed greater reductions in A1C from baseline compared with insulin glargine alone (− 1.1% vs − 0.6%, P < 0.0001) and significantly more patients treated with iGlarLixi reached a target A1C of less than 7.0% (55% vs 30%, respectively; P < 0.001). In addition, iGlarLixi was superior to insulin glargine in achieving the composite endpoint of A1C < 7.0% with no weight gain and with no documented symptomatic hypoglycemia (20% vs 9%, respectively; P < 0.001) at week 30 [14]. LixiLan-O compared iGlarLixi with its components insulin glargine or lixisenatide in patients inadequately controlled on metformin, with or without a second OAD, which was subsequently discontinued. As in LixiLan-L, greater reductions in A1C from baseline were achieved with iGlarLixi compared with insulin glargine (− 1.6% vs − 1.3%, respectively; P < 0.0001) and significantly more patients treated with iGlarLixi compared with insulin glargine achieved target A1C < 7.0% (74% vs 59%, respectively; P < 0.0001) and met the composite endpoint of A1C < 7.0% with no weight gain and with no documented symptomatic hypoglycemia (32% vs 19%, respectively; P < 0.0001). iGlarLixi also induced fewer GI AEs compared with lixisenatide alone (27.1% vs 36.9%, respectively) [13]. As one might expect, patients in the LixiLan-L study had different characteristics to those in the LixiLan-O study, such as a longer duration of diabetes (mean duration 12 years and 8.8 years, respectively) and more advanced disease requiring basal insulin treatment [13, 14]. Overall, the LixiLan studies demonstrated that iGlarLixi significantly improved glycemic control compared with the individual components, with a risk of hypoglycemia comparable to insulin glargine, mitigation of weight gain compared with insulin glargine, and reduced GI AEs compared with lixisenatide.
Methods
In this review, we collated patient-level data from the LixiLan proof-of-concept trial, the LixiLan-L trial, and the LixiLan-O trial to evaluate AEs associated with iGlarLixi treatment [13, 14, 23]. A pool of 2222 patients from the LixiLan phase 2/3 studies was used to summarize malignancies, renal AEs, and AEs adjudicated as allergic reactions, major cardiovascular events, injection site reactions, and thyroid disorders. A pool of 1899 patients from the LixiLan phase 3 trials was the primary basis to describe the overall treatment-emergent adverse events (TEAEs), serious TEAEs, TEAEs leading to treatment discontinuation, and adjudicated pancreatic events. The LixiLan-L and LixiLan-O trials were used separately to provide an overview of hypoglycemia rates. We also describe data from the ELIXA study to determine the incidence of pancreatitis and pancreatic cancer, and the ORIGIN and ELIXA studies for cardiovascular safety data [18, 19]. Data reported in this review was collated from studies for which all data is available in the public domain; no novel data was generated.
Results and Discussion
Safety of iGlarLixi
A summary of the AEs reported in the iGlarLixi phase 3 clinical trials is provided in Tables 1 and 2 [27].
Hypoglycemia
Hypoglycemia is one of the most common AEs in patients receiving insulin therapies [28], and poses a major barrier to insulin initiation and treatment intensification. Fear of hypoglycemia often leads to treatment discontinuation, further contributing to suboptimal glycemic control. Hypoglycemia rates reported in clinical trials vary depending on definition of hypoglycemia used, duration of T2D, patient age, renal function, insulin dose, fasting plasma glucose target, intensity of glucose control and background therapy, meaning comparisons between studies can be inconclusive [28]. Therefore, this section discusses the rates of hypoglycemia reported in LixiLan-L and LixiLan-O trials separately.
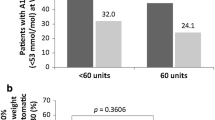
The incidence of documented symptomatic hypoglycemia (plasma glucose ≤ 70 mg/dL) in patients receiving iGlarLixi was 40.0% in the LixiLan-L trial and 25.6% in LixiLan-O trial (Table 3), which compared favorably with the incidence of documented symptomatic hypoglycemia in patients treated with insulin glargine alone (LixiLan-L, 42.5%; LixiLan-O, 23.6%) [13, 14]. Consequently, the number of patients experiencing hypoglycemia within each trial was no higher with iGlarLixi compared with insulin glargine alone, despite a lower A1C in the iGlarLixi groups. The higher incidence of hypoglycemia observed in the LixiLan-L study is likely due to patients having a longer duration of diabetes and longer duration of insulin treatment [29]. In the LixiLan-L trial, the rate of hypoglycemia events was lower with iGlarLixi compared with insulin glargine alone (3.03 vs 4.22 events per patient year, respectively) and was similar between iGlarLixi and insulin glargine alone in LixiLan-O (1.4 vs 1.2 events per patient-year, respectively). These data demonstrate that the risk of symptomatic documented hypoglycemia in patients receiving insulin glargine in combination with lixisenatide (i.e., as iGlarLixi) is lower or comparable to that in patients receiving insulin glargine alone.
The incidence of severe hypoglycemia (an event requiring third-party assistance) was generally low in both the LixiLan-L trial (n = 4 [1.1%] and n = 1 [0.3%] for the iGlarLixi arm and insulin glargine arm, respectively) and in the LixiLan-O trial (n = 0 [0.0%], n = 1 [0.2%], n = 0 [0.0%] in the iGlarLixi, insulin glargine, and lixisenatide arms, respectively) [13, 14].
Gastrointestinal Tolerability
Overall, the LixiLan trials demonstrated a low incidence of GI AEs with low rates of permanent treatment discontinuation when utilizing iGlarLixi compared with lixisenatide alone [30]. The GI events that did arise were mainly mild to moderate in severity, transient, and occurred primarily during the first 8 weeks of treatment [13, 14]. The rates of GI AEs in patients treated with iGlarLixi were lower than those treated with lixisenatide alone, while rates of GI AEs in patients treated with insulin glargine alone were predictably lower than in patients treated with iGlarLixi [13].
In the LixiLan-L trial, GI AEs occurred in 17.0% of patients receiving iGlarLixi compared with 7.9% of patients treated with insulin glargine. These AEs were generally mild, with nausea occurring in 10.4% of patients (vs 0.5% insulin glargine), diarrhea in 4.4% of patients (vs 2.7% insulin glargine), and vomiting in 3.6% (vs 0.5% insulin glargine) [14]. In the LixiLan-O trial, the incidence of GI AEs was 21.7% among patients treated with iGlarLixi compared with 12.6% of patients treated with insulin glargine and 36.9% for patients treated with lixisenatide. Nausea was the most common GI AE experienced with iGlarLixi occurring in 9.6% of patients (vs 3.6% insulin glargine, vs 24.0% lixisenatide), 9.0% experiencing diarrhea (vs 4.3% insulin glargine, vs 9.0% lixisenatide), and 3.2% experiencing vomiting (vs 1.5% insulin glargine, vs 6.4% lixisenatide) [13].
The rates of treatment discontinuation due to GI AEs were low in both trials. In LixiLan-L, treatment discontinuation due to GI AEs was observed in 1.1% of patients and was exclusively due to nausea [14]. No GI AEs associated with insulin glargine resulted in treatment discontinuation. In LixiLan-O, treatment discontinuation resulting from GI AEs occurred in 1.0% of iGlarLixi-treated patients overall, with 0.4% of patients discontinuing due to nausea (vs 2.6% lixisenatide), 0.4% due to vomiting (vs 1.7% lixisenatide), and 0.2% due to diarrhea (vs 0.9% lixisenatide) [13]. No GI AEs associated with insulin glargine resulted in treatment discontinuation [13].
The gradual dose increase of lixisenatide occurring simultaneously with up-titration of insulin glargine could explain the lower incidence of GI AEs observed with iGlarLixi when compared with lixisenatide alone [27]. Incidences of nausea and vomiting per week in iGlarLixi vs insulin glargine in LixiLan-L and vs lixisenatide in LixiLan-O, over 30 weeks, are shown in Fig. 2.
Immunogenicity
The synthetic proteins used in the treatment of T2D often activate an immunologic response that results in the production of anti-drug antibodies (ADAs) in patients undergoing treatment. Severe immunologic complications are rare, and although there have been some reports that ADAs can affect glycemic control, the majority of clinical trial data suggest otherwise [31]. The measurement of ADAs is routine in T2D clinical trials, to establish whether or not antibody positivity influences the safety and efficacy of the product. However, incidence rates can vary widely between products, and it is often difficult to perform a direct comparison of ADA incidence because of differences in the methodology and interpretation of data, the product, and the patient population [32]. In the LixiLan-O study, 21% of patients treated with iGlarLixi and 8.9% of patients that received insulin glargine were positive for anti-insulin glargine antibodies after 30 weeks of treatment; while in the LixiLan-L study, the incidence was comparable between the iGlarLixi (26.2%) and insulin glargine (24.8%) treatment groups [27]. There were no substantial differences noted in the efficacy or safety profiles of the antibody-positive and antibody-negative patient populations (for both anti-insulin glargine and anti-lixisenatide patients) in either of the iGlarLixi phase 3 trials [13, 14].
Hypersensitivity Reactions
Local and Injection-Site Reactions
As with any subcutaneous injected peptide, injection-site reactions, including hematoma, pain, hemorrhage, erythema, swelling, and pruritus may be experienced. In the phase 2/3 study pool, 1.7% of patients receiving iGlarLixi and 1.1% of patients receiving insulin glargine alone experienced an injection-site reaction. These events were generally mild, with one patient reporting a moderate event in each group [27].
Allergic Reactions
Subcutaneously injected synthetic peptides, such as GLP-1 RAs, have the potential to cause allergic reactions [33]. For iGlarLixi development, the Allergic Reaction Assessment Committee (ARAC) reviewed all investigator-reported allergic reaction events in a blinded manner, using stringent criteria to determine the severity of the event and whether or not it was related to the study drug. In the phase 3 LixiLan studies, the number of iGlarLixi-treated patients with an event adjudicated by the ARAC as an allergic reaction was 7 (0.7%) in the iGlarLixi group, 5 (0.5%) in the insulin glargine group, and 2 (0.9%) in the lixisenatide group [27]. The majority of patients (9/14) had events that were assessed as not related to study drug. In LixiLan-O, there were 3 (0.3%) patients in the iGlarLixi arm, no patients in the insulin glargine arm, and 2 (0.9%) patients in the lixisenatide arm with events adjudicated as an allergic reaction possibly related to study drug. All events were graded moderate in severity [27].
Pancreatitis
The use of GLP-1 RAs has been associated with a risk of developing acute pancreatitis, including fatal and non-fatal hemorrhagic or necrotizing pancreatitis [34]. In the phase 3 LixiLan studies, there were no reported episodes of pancreatitis [13, 14, 27]. Low overall rates of pancreatitis in patients receiving either lixisenatide or placebo were also reported in the ELIXA study (for patients receiving at least one dose of lixisenatide, n = 3031; or placebo, n = 3032, median follow-up period 25 months), with a lower incidence of pancreatitis in the lixisenatide group (n = 5; 0.2%) compared with the placebo group (n = 8; 0.3%) [19, 27].
Malignancy
Pancreatic and Other Cancers
It remains controversial whether or not GLP-1 RA-based therapies increase the risk of developing specific malignant diseases, such as pancreatic carcinoma or thyroid cancer. In a study by Elashoff et al., which analyzed the US Food and Drug Administration (FDA)’s database of reported AEs associated with the GLP-1 RA exenatide, they found the human data to be consistent with animal data, showing that GLP-1 RA therapies were associated with an increased risk of pancreatitis [34]. Since pancreatitis is a risk factor for pancreatic cancer, there was a concern that chronic use of GLP-1 RA-based therapies might therefore be a risk factor for pancreatic cancer in the long term [34]. However, it has been suggested that this analysis was limited by a reporting bias and, therefore, provides insufficient evidence to make this association [35]. Potential malignant pancreatic events and other cancers were also assessed for causality by an adjudication committee for the LixiLan studies (iGlarLixi vs insulin glargine) and the ELIXA trial (lixisenatide vs placebo) specifically [27]. Similar to the incidence of pancreatitis in the LixiLan trials, the incidence of pancreatic cancer was also low. There was a single case of malignant pancreatic neoplasm reported for the insulin glargine group in LixiLan-O that led to permanent treatment discontinuation, but this case was found to be unrelated to the study drug; there were no incidences of pancreatic cancer in the groups receiving iGlarLixi or lixisenatide [13, 27]. A key constraint of the LixiLan trials was their relatively short duration (30 weeks), though this has been solved by the longer-term ELIXA cardiovascular outcomes trials.
The ELIXA study (lixisenatide, n = 3031; placebo, n = 3032), conducted over a median follow-up period of 25 months, confirmed the low rate of malignant pancreatic neoplasms reported in 3 (< 0.1%) patients treated with lixisenatide compared to 9 (0.3%) patients receiving placebo, a similar imbalance to that seen with cases of pancreatitis in favor of lixisenatide [27].
Thyroid Malignancy
In a filing to the FDA, thyroid tumors were reported to be increased in rodents treated with liraglutide and other long-acting GLP-1 RAs [36]. As a result of this preclinical evidence, the use of liraglutide, exenatide extended-release, dulaglutide, and semaglutide is contraindicated in patients with a personal or family history of thyroid carcinoma, and the prescribing information for these long-acting GLP-1 RAs includes a black-box warning in the USA for risk of thyroid C cell tumors [37,38,39,40]. However, as is the case for pancreatic cancer, the evidence supporting the hypothesis that GLP-1 RAs cause (medullary) thyroid cancer is insufficient [35]. To date, no cases of thyroid carcinoma have been identified from clinical trials or through post-marketing surveillance for patients treated with iGlarLixi. Additionally, there were no clinically significant changes in mean calcitonin levels related to treatment with iGlarLixi during the clinical trial program [27].
Renal Function
In the USA and other western countries, T2D is recognized as a leading cause of chronic kidney disease and end-stage renal disease [41]. Acute kidney injury and worsening of chronic renal failure (which are generally due to GI AEs and dehydration [42]) have been observed in patients treated with GLP-1 RAs, such as lixisenatide. These events were also found in patients without any known renal disease [15].
Analysis of pooled data from the LixiLan trials showed that during the on-treatment period, similar proportions of patients treated with iGlarLixi and those treated with insulin glargine had mild and moderate renal impairment based upon creatinine clearance. There were no patients with severe renal impairment in the iGlarLixi or lixisenatide groups, while the proportion was low in the insulin glargine group (0.2%) [27]. A post hoc analysis from the ELIXA trial in patients with T2D without severe renal impairment (estimated glomerular filtration rate [eGFR] > 30 mL/min/1.73 m2), but with a recent acute coronary syndrome event, demonstrated that the addition of lixisenatide to usual care improved the burden of micro- and macroalbuminuria beyond glycemic control (reduction in urinary albumin/creatinine ratio) [43]. In the LixiLan trials, patients with an eGFR < 30 mL/min were excluded from participation (considered severe renal impairment to end-stage chronic kidney disease).
The incidence of common TEAEs in the iGlarLixi and insulin glargine treatment groups was similar in both patients with normal renal function (53.8% iGlarLixi vs 48.5% insulin glargine) and in patients with mild renal impairment at baseline for the phase 3 study pool (56.5% iGlarLixi vs 54.0% insulin glargine) [27].
Cardiovascular Safety
In 2008, the FDA recommended that all new antihyperglycemic medications being investigated for the treatment of T2D should be evaluated for cardiovascular AEs [44]. In the LixiLan trials, the Cardiovascular Events Adjudication Committee, which comprised cardiovascular and cerebrovascular disease experts independent of the sponsor and the investigators, was set up to adjudicate cardiovascular endpoints in a blinded manner. A cardiovascular outcome trial was not required for iGlarLixi since the lixisenatide and insulin glargine components had each been evaluated for cardiovascular outcomes in the ELIXA and ORIGIN trials, respectively. The LixiLan trials were, therefore, not powered to specifically assess cardiovascular outcomes. However, data from these trials showed that the incidence of cardiovascular events in patients treated with iGlarLixi was low and comparable to that observed in patients taking insulin glargine [13, 14].
The ELIXA study included 6068 patients who had experienced an acute coronary syndrome event (acute myocardial infarction [MI] or hospitalization for MI) within the previous 180 days, representing a relatively unstable population at particularly high cardiovascular risk [19]. Over a median follow-up of 25 months, the composite primary endpoint of cardiovascular death, non-fatal MI, non-fatal stroke, and hospitalization for unstable angina (4-point major adverse cardiovascular event) was comparable between patients receiving lixisenatide (13.4%) and those receiving placebo (13.2%). Hospitalization rates for heart failure were comparable between the two groups (hazard ratio, 0.96; 95% confidence interval [CI], 0.75–1.23), as were rates of death (hazard ratio 0.94; 95% CI 0.78–1.13) [19].
The ORIGIN trial [45] demonstrated that there was no increased risk of cardiovascular events associated with insulin glargine in patients with prediabetes or early T2D and high cardiovascular risk. Additionally, there was no association with increased risk of serious cardiovascular events in individuals with pre-existing cardiovascular risk factors compared with standard of care. Rates of cardiovascular events were similar with insulin glargine and standard care (2.94 and 2.85 per 100 person-years, respectively).
Adverse Events in Specific Populations
Older Patients
In older patients (≥ 65 years), a post hoc analysis of data from the LixiLan-L and LixiLan-O trials showed that iGlarLixi was associated with no increased risk of hypoglycemia when compared with insulin glargine. Modest weight loss was observed in iGlarLixi-treated older patients in both the LixiLan-L (P = 0.007) and LixiLan-O (P = 0.017) trials [46]. Of the 834 patients in the LixiLan studies who received iGlarLixi, 25.2% (n = 210) were at least 65 years of age and 4% (n = 33) were at least 75 years of age. Overall, there was no difference in safety and efficacy of iGlarLixi observed across the age groups [15].
Gender
A further post hoc analysis of the LixiLan trials found no differences in the effects of iGlarLixi based on gender [47].
Children and Pregnancy
To date, the use of iGlarLixi, or its components, has not been studied in children with T2D or during pregnancy [15, 25, 26]. It is currently recommended that iGlarLixi should not be used during pregnancy unless the potential benefits outweigh the potential risks to the developing fetus.
Summary
Treatment with insulin and a GLP-1 RA targets seven of the eight pathophysiologic defects which lead to hyperglycemia in T2D [20]. The complementary actions of insulin glargine and lixisenatide have been shown to exert beneficial effects on A1C, with no increased risk of hypoglycemia, while also reducing body weight compared with insulin glargine alone, and with fewer GI side effects than lixisenatide alone [13, 14, 23]. iGlarLixi, given as a once-daily subcutaneous injection, has been shown to reduce the incidence of common AEs associated with lixisenatide, such as nausea and vomiting. This is likely to be related to the more gradual titration of lixisenatide in iGlarLixi, which runs parallel to the up-titration of insulin. Moreover, safety data of the individual components of iGlarLixi have shown no increased risk of cardiovascular disease, thyroid cancer, pancreatitis, or pancreatic malignancy. In addition to offering comparable safety and reduced AEs, combination therapies are generally considered to be a more convenient alternative to taking the individual components separately, providing simpler treatment regimens with fewer daily injections.
References
Riddle MC, Aronson R, Home P, et al. Adding once-daily lixisenatide for type 2 diabetes inadequately controlled by established basal insulin: a 24-week, randomized, placebo-controlled comparison (GetGoal-L). Diabetes Care. 2013;36:2489–96.
Riddle MC, Forst T, Aronson R, et al. Adding once-daily lixisenatide for type 2 diabetes inadequately controlled with newly initiated and continuously titrated basal insulin glargine: a 24-week, randomized, placebo-controlled study (GetGoal-Duo 1). Diabetes Care. 2013;36:2497–503.
Diamant M, Nauck MA, Shaginian R, et al. Glucagon-like peptide 1 receptor agonist or bolus insulin with optimized basal insulin in type 2 diabetes. Diabetes Care. 2014;37:2763–73.
Rosenstock J, Fonseca VA, Gross JL, et al. Advancing basal insulin replacement in type 2 diabetes inadequately controlled with insulin glargine plus oral agents: a comparison of adding albiglutide, a weekly GLP-1 receptor agonist, versus thrice-daily prandial insulin lispro. Diabetes Care. 2014;37:2317–25.
Inzucchi SE, Bergenstal RM, Buse JB, et al. Management of hyperglycemia in type 2 diabetes, 2015: a patient-centered approach. Update to a position statement of the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care. 2015;38:140–9.
Leiter LA, Gross JL, Chow F, et al. Once weekly glucagon-like peptide-1 receptor agonist albiglutide vs prandial insulin added to basal insulin in patients with type 2 diabetes mellitus: results over 52 weeks. J Diabetes Complicat. 2017;31:1283–5.
Maiorino MI, Chiodini P, Bellastella G, Capuano A, Esposito K, Giugliano D. Insulin and glucagon-like peptide 1 receptor agonist combination therapy in type 2 diabetes: a systematic review and meta-analysis of randomized controlled trials. Diabetes Care. 2017;40:614–24.
Khunti K, Nikolajsen A, Thorsted BL, Andersen M, Davies MJ, Paul SK. Clinical inertia with regard to intensifying therapy in people with type 2 diabetes treated with basal insulin. Diabetes Obes Metab. 2016;18:401–9.
Blonde L, Meneghini L, Peng XV, et al. Probability of achieving glycemic control with basal insulin in patients with type 2 diabetes in real-world practice in the USA. Diabetes Ther. 2018;9:1347–58.
Davies M. The reality of glycaemic control in insulin treated diabetes: defining the clinical challenges. Int J Obes Relat Metab Disord. 2004;28(Suppl 2):S14–22.
Ross SA. Breaking down patient and physician barriers to optimize glycemic control in type 2 diabetes. Am J Med. 2013;126(9 Suppl 1):S38–48.
Cersosimo E, Johnson EL, Chovanes C, Skolnik N. Initiating therapy in patients newly diagnosed with type 2 diabetes: combination therapy versus a stepwise approach. Diabetes Obes Metab. 2018;20:497–507.
Rosenstock J, Aronson R, Grunberger G, et al. Benefits of LixiLan, a titratable fixed-ratio combination of insulin glargine plus lixisenatide, versus insulin glargine and lixisenatide monocomponents in type 2 diabetes inadequately controlled on oral agents: the LixiLan-O randomized trial. Diabetes Care. 2016;39:2026–35.
Aroda VR, Rosenstock J, Wysham C, et al. Efficacy and safety of LixiLan, a titratable fixed-ratio combination of insulin glargine plus lixisenatide in type 2 diabetes inadequately controlled on basal insulin and metformin: the LixiLan-L randomized trial. Diabetes Care. 2016;39:1972–80.
Sanofi Inc. Soliqua®. Prescribing information 2017. http://products.sanofi.us/soliqua100-33/soliqua100-33.pdf. Accessed June 2017.
Sanofi. Press Release. Sanofi receives FDA approval of Soliqua™ 100/33 for the treatment of adults with type 2 diabetes, 2016. http://www.news.sanofi.us/2016-11-21-Sanofi-Receives-FDA-Approval-of-Soliqua-100-33-for-the-Treatment-of-Adults-with-Type-2-Diabetes/. Accessed Feb 2018.
Sanofi. Press Release. Suliqua™ Approved in the European Union for the treatment of adults with type 2 diabetes, 2017. http://mediaroom.sanofi.com/suliquatm-approved-in-the-european-union-for-the-treatment-of-adults-with-type-2-diabetes/. Accessed Feb 2018.
Hanefeld M, Monnier L, Schnell O, Owens D. Early treatment with basal insulin glargine in people with type 2 diabetes: lessons from ORIGIN and other cardiovascular trials. Diabetes Ther. 2016;7:187–201.
Pfeffer MA, Claggett B, Diaz R, et al. Lixisenatide in patients with type 2 diabetes and acute coronary syndrome. N Engl J Med. 2015;373:2247–57.
DeFronzo RA, Eldor R, Abdul-Ghani M. Pathophysiologic approach to therapy in patients with newly diagnosed type 2 diabetes. Diabetes Care. 2013;36(Suppl 2):S127–38.
Fineman MS, Cirincione BB, Maggs D, Diamant M. GLP-1 based therapies: differential effects on fasting and postprandial glucose. Diabetes Obes Metab. 2012;14:675–88.
Lorenz M, Pfeiffer C, Steinsträsser A, et al. Effects of lixisenatide once daily on gastric emptying in type 2 diabetes—relationship to postprandial glycemia. Regul Pept. 2013;185:1–8.
Rosenstock J, Diamant M, Aroda VR, et al. Efficacy and safety of LixiLan, a titratable fixed-ratio combination of lixisenatide and insulin glargine, versus insulin glargine in type 2 diabetes inadequately controlled on metformin monotherapy: the LixiLan proof-of-concept randomized trial. Diabetes Care. 2016;39:1579–86.
Riddle MC, Rosenstock J, Gerich J, Insulin Glargine 4002 Study Investigators. The treat-to-target trial: randomized addition of glargine or human NPH insulin to oral therapy of type 2 diabetic patients. Diabetes Care. 2003;26:3080–6.
Sanofi. Lantus®. Prescribing information 2009. https://www.accessdata.fda.gov/drugsatfda_docs/label/2009/021081s034lbl.pdf. Accessed Feb 2018.
Sanofi. Adlyxin®. Prescribing information 2016. http://products.sanofi.us/adlyxin/adlyxin.pdf. Accessed Feb 2018.
Sanofi. Lixisenatide and iGlarLixi (insulin glargine/lixisenatide fixed-ratio combination) for the treatment of type 2 diabetes: briefing document for the Endocrinologic and Metabolic Drugs Advisory Committee meeting: May 25 2016. http://www.fda.gov/downloads/AdvisoryCommittees/CommitteesMeetingMaterials/Drugs/EndocrinologicandMetabolicDrugsAdvisoryCommittee/UCM502559.pdf. Accessed Aug 2018.
Morales J, Schneider D. Hypoglycemia. Am J Med. 2014;127:S17–24.
UK Hypoglycaemia Study Group. Risk of hypoglycaemia in types 1 and 2 diabetes: effects of treatment modalities and their duration. Diabetologia. 2007;50:1140–7.
Trujillo J, Roberts M, Dex T, Chao J, White J, LaSalle J. Low incidence of gastrointestinal adverse events over time with a fixed-ratio combination of insulin glargine and lixisenatide vs lixisenatide alone. Diabetes Obes Metab. 2018;20:2690.
Fineberg SE, Kawabata TT, Finco-Kent D, Fountaine RJ, Finch GL, Krasner AS. Immunological responses to exogenous insulin. Endocr Rev. 2007;28:625–52.
Gunn GR 3rd, Sealey DC, Jamali F, Meibohm B, Ghosh S, Shankar G. From the bench to clinical practice: understanding the challenges and uncertainties in immunogenicity testing for biopharmaceuticals. Clin Exp Immunol. 2016;184:137–46.
Filippatos TD, Panagiotopoulou TV, Elisaf MS. Adverse effects of GLP-1 receptor agonists. Rev Diabet Stud. 2014;11:202–30.
Elashoff M, Matveyenko AV, Gier B, Elashoff R, Butler PC. Pancreatitis, pancreatic, and thyroid cancer with glucagon-like peptide-1-based therapies. Gastroenterology. 2011;141:150–6.
Nauck MA, Friedrich N. Do GLP-1-based therapies increase cancer risk? Diabetes Care. 2013;36(Suppl 2):S245–52.
FDA. Victoza® (liraglutide injection): Human relevance of rodent thyroid C-cell tumors. 2009. https://wayback.archive-it.org/7993/20170404152315/https://www.fda.gov/downloads/AdvisoryCommittees/CommitteesMeetingMaterials/Drugs/EndocrinologicandMetabolicDrugsAdvisoryCommittee/UCM151176.pdf. Accessed Sept 2018.
AstraZeneca. Bydureon®. Prescribing information 2012. https://www.accessdata.fda.gov/drugsatfda_docs/label/2012/022200s000lbl.pdf. Accessed Jan 2018.
Novo Nordisk. Ozempic®. Prescribing information. https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/209637lbl.pdf. Accessed Feb 2018.
Eli Lilly. Trulicity®. Prescribing information 2018. https://pi.lilly.com/us/trulicity-uspi.pdf. Accessed Feb 2018.
Novo Nordisk. Victoza®. Prescribing information 2017. http://www.novo-pi.com/victoza.pdf. Accessed Jan 2018.
World Health Organization. Global report on diabetes. 2016. http://apps.who.int/iris/bitstream/handle/10665/204871/9789241565257_eng.pdf;jsessionid=00331698D9C67252ADDAAB586965A2F4?sequence=1. Accessed Sept 2018.
Filippatos TD, Elisaf MS. Effects of glucagon-like peptide-1 receptor agonists on renal function. World J Diabetes. 2013;4:190–201.
Muskiet MA, Tonneijck L, Huang Y, et al. Lixisenatide and renal outcomes in patients with type 2 diabetes—a post hoc analysis of the ELIXA trial. Diabetes Care. 2018;67(Suppl):1.
FDA. Guidance for industry. Diabetes mellitus—evaluating cardiovascular risk in new antidiabetic therapies to treat type 2 diabetes. 2008. https://www.fda.gov/downloads/Drugs/Guidances/ucm071627.pdf. Accessed Feb 2018.
Gerstein HC, Bosch J, Dagenais GR, et al. Basal insulin and cardiovascular and other outcomes in dysglycemia. N Engl J Med. 2012;367:319–28.
Handelsman Y, Chovanes C, Dex T, et al. Efficacy and safety of insulin glargine/lixisenatide fixed-ratio combination in elderly patients with T2D. Diabetes. 2016;65:A246 (ADA 2016, abstract 954).
Frias J, Stager W, Davidson J. Effect of gender on clinical outcomes of patients with type 2 diabetes treated with insulin glargine/lixisenatide fixed-ratio combination. AANP 2017.
Acknowledgements
The authors would like to thank Christine Roy, Dan Gil, Kristen Sharma, Leila Larbi, and Tammie Adomako for their expert advice on the content and development of this manuscript.
Funding
This study was funded by Sanofi US Inc. The journal’s article processing charges were also funded by Sanofi US, Inc.
Medical Writing and Editorial Assistance
The authors received writing/editorial support in the preparation of this manuscript provided by Georgina Bowden, PhD and Keisha Peters, MSc of Excerpta Medica, funded by Sanofi US, Inc.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Authorship Contributions
All authors contributed to the data analysis and critical review of this manuscript.
Disclosures
Juan P. Frias has received research support from AbbVie, Allergan, AstraZeneca, Boehringer Ingelheim, BMS, Elcelyx, Eli Lilly, Genentech, IONIS, Janssen, Johnson and Johnson, Lexicon, Ligand, Madrigal, Merck, Mylan, Novartis, Novo Nordisk, Pfizer, Sanofi, and Theracos. He has also received consultancy fees and/or honoria for serving on advisory boards from AstraZeneca, BMS, Elcelyx, Johnson and Johnson, Novo Nordisk, and Sanofi. Terry Dex is an employee of Sanofi US, Inc. Michelle Roberts is an employee of Sanofi US, Inc. Allen Kaplan serves on the adjudication committee regarding angioedema events for Genentech.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors.
Data Availability
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Author information
Authors and Affiliations
Corresponding author
Additional information
Enhanced Digital Features
To view enhanced digital features for this article go to https://doi.org/10.6084/m9.figshare.7392701.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Frias, J.P., Dex, T., Roberts, M. et al. A Review of the Safety and Adverse Event Profile of the Fixed-Ratio Combination of Insulin Glargine and Lixisenatide. Diabetes Ther 10, 21–33 (2019). https://doi.org/10.1007/s13300-018-0547-5
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-018-0547-5