Abstract
Introduction
This study assessed the safety and efficacy of ertugliflozin (an oral sodium-glucose cotransporter 2 inhibitor) vs. glimepiride in patients with type 2 diabetes mellitus (T2DM) inadequately controlled on metformin.
Methods
This phase III, double-blind, non-inferiority study (NCT01999218) randomized patients with HbA1c ≥ 7.0% and ≤ 9.0% on stable metformin ≥ 1500 mg/day 1:1:1 to ertugliflozin 15 or 5 mg once-daily (QD), or glimepiride (titrated from 1 mg QD). The primary hypothesis was that ertugliflozin 15 mg was non-inferior to glimepiride on HbA1c (non-inferiority criterion: upper bound of the 95% confidence interval [CI] about the treatment difference < 0.3%).
Results
Mean baseline HbA1c of randomized patients (N = 1326) was 7.8%. Mean and median doses of glimepiride were 3.0 mg/day throughout the study. At week 52, the least squares mean change (95% CI) from baseline in HbA1c was − 0.6% (− 0.7, − 0.5), − 0.6% (− 0.6, − 0.5), and − 0.7% (− 0.8, − 0.7) in the ertugliflozin 15 mg, ertugliflozin 5 mg, and glimepiride groups, respectively. The between-group difference for ertugliflozin 15 mg and glimepiride of 0.1% (− 0.0, 0.2) met the pre-specified non-inferiority criterion. Relative to glimepiride, greater body weight and systolic blood pressure (SBP) reductions were observed with ertugliflozin. The overall incidence of adverse events (AEs) was similar across groups. The incidence of symptomatic hypoglycemia and genital mycotic infection (GMI) were, respectively, lower and higher with ertugliflozin relative to glimepiride. The incidences of urinary tract infection and hypovolemia AEs were not meaningfully different among the groups.
Conclusions
Ertugliflozin 15 mg was non-inferior to glimepiride in reducing HbA1c when added to metformin in patients with T2DM. Ertugliflozin had an acceptable safety profile and resulted in less hypoglycemia and more GMIs than glimepiride.
Clinical Trial Registration
Clinicaltrials.gov NCT01999218.
Similar content being viewed by others
Introduction
Current guidelines recommend metformin as first-line pharmacological treatment for patients with type 2 diabetes mellitus (T2DM) [1]. However, T2DM is a progressive disease and many individuals require combination therapy to maintain glycemic control. Sulfonylureas (SUs) remain a common second-line treatment option [1]; however, they reduce blood glucose levels by glucose-independent stimulation of insulin release from the pancreas, with an associated increased risk of hypoglycemia and weight gain [2]. The risk of hypoglycemia varies within the drug class; newer-generation SUs gliclazide and glimepiride have been associated with a lower risk of hypoglycemia relative to other SUs [3, 4]. The efficacy of SUs can attenuate over time. There have also been reports of increased cardiovascular risk with SUs, although further evidence is needed to establish the cardiovascular safety of SUs [5].
In phase III clinical studies, the sodium-glucose cotransporter 2 (SGLT2) inhibitor ertugliflozin improved glycemic control and reduced body weight and blood pressure (BP) with a low incidence of hypoglycemia as monotherapy [6], as add-on to metformin [7], or as add-on to the combination of sitagliptin and metformin [8]. As an SGLT2 inhibitor, ertugliflozin has a mechanism of action complementary to all other classes of antihyperglycemic agents, and therefore may represent a useful therapy at all stages of T2DM [9].
The VERTIS (eValuation of ERTugliflozin effIcacy and Safety) SU study compared the safety and efficacy of ertugliflozin (15 and 5 mg) with that of glimepiride in adult patients with T2DM and inadequate glycemic control on metformin monotherapy. The primary hypothesis was that the glycemic efficacy of ertugliflozin 15 mg, as an add-on to metformin, was non-inferior to that of glimepiride after 52 weeks of treatment.
Methods
Study Design
Protocol MK-8835-002 was a multicenter, randomized, double-blind, active-controlled, parallel-group, phase III clinical study (VERTIS SU; ClinicalTrials.gov identifier: NCT01999218). The study was conducted over 104 weeks in two 52-week phases; the primary and secondary hypotheses were pre-specified for testing at week 52 (phase A); treatment was continued for another 52 weeks (phase B) to evaluate longer-term safety and efficacy of ertugliflozin. Phase A results are reported here.
Patients with adequate compliance during the placebo run-in period (≥ 80% based on pill count) and who met all other entry criteria were randomized 1:1:1 to ertugliflozin 15 mg once-daily (QD), ertugliflozin 5 mg QD, or glimepiride titrated from 1 mg up to 6 or 8 mg QD (to either maximum dose according to the local country label or maximum tolerated dose). Randomization was performed using a central electronic randomization system. Ertugliflozin and glimepiride tablets were packaged identically relative to their matching placebos. Study personnel, including patients, investigators, study site, central laboratory, and the sponsor remained blinded throughout the 52-week phase A treatment period.
To manage both hyperglycemia and hypoglycemia, the dose of glimepiride/matching placebo was to be up- and/or down-titrated throughout the study duration on the basis of finger-stick glucose determinations performed in the clinic or at home, and by the investigator’s clinical assessment of the patient’s glycemic status (see Supplementary Methods).
Glycemic rescue therapy with open-label sitagliptin was prescribed for patients meeting progressively more stringent glycemic rescue criteria (see Supplementary Methods). Rescued patients continued on their study medication and background metformin.
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964, as revised in 2013. It was conducted in accordance with the principles of good clinical practice and approved by the appropriate institutional review boards and regulatory agencies. Informed consent was obtained from all individual participants included in the study. The protocol and statistical analysis plan were developed by the sponsors in consultation with an external Scientific Advisory Committee.
The methods used in this study are similar to those previously reported for other VERTIS studies [6,7,8, 10].
Patient Population
Patients aged at least 18 years with T2DM and inadequate glycemic control (HbA1c ≥ 53 and ≤ 75 mmol/mol [≥ 7.0% and ≤ 9.0%]) on ≥ 1500 mg/day of metformin monotherapy for at least 8 weeks at screening were eligible for the study and, if other criteria were met, could proceed directly into a 2-week, single-blind placebo run-in period prior to randomization. Patients on this regimen for less than 8 weeks, on lower doses of metformin, or on any dose of metformin with another antihyperglycemic agent (AHA) at screening were eligible if they met the above criteria after the appropriate dose/medication adjustment, stabilization, or washout period (see Supplementary Methods).
Key patient exclusion criteria included history of type 1 diabetes mellitus or of ketoacidosis; weight not stable (≥ 5% change in body weight in previous 6 months); treatment in previous 12 weeks with insulin or any other type of injectable AHA, pioglitazone or rosiglitazone, other SGLT2 inhibitors, bromocriptine, or colesevelam, or any other AHAs, with the exceptions of SUs administered at less than 50% of the maximum approved dose, dipeptidyl peptidase-4 (DPP-4) inhibitors, meglitinides, and alpha-glucosidase inhibitors; history of myocardial infarction (MI), unstable angina, arterial revascularization, stroke, transient ischemic attack, or New York Heart Association functional class III–IV heart failure within 3 months of screening; any active, obstructive uropathy or indwelling urinary catheter; mean value for triplicate sitting systolic BP (SBP) > 160 mmHg and/or diastolic BP (DBP) > 90 mmHg (patients on BP medication must have been on a stable regimen for at least 4 weeks prior to randomization); estimated glomerular filtration rate (eGFR) < 55 mL/min/1.73 m2; serum creatinine ≥ 115 μmol/L (1.3 mg/dL) in men or ≥ 106 μmol/L (1.2 mg/dL) in women.
Efficacy Assessments
The primary efficacy endpoint was change from baseline in HbA1c at week 52. Key secondary efficacy endpoints were the changes from baseline in body weight and SBP at week 52. Other efficacy endpoints evaluated at week 52 included the percentage of patients with HbA1c < 53 mmol/mol (7.0%); changes from baseline in DBP, fasting plasma glucose (FPG), homeostasis model assessment of β-cell function (HOMA-β), and proinsulin/C-peptide ratio; the percentage of patients requiring rescue medication; and the percentage of patients meeting the composite endpoints of (1) HbA1c reduction > 5.5 mmol/mol (0.5%) with no symptomatic hypoglycemia or body weight gain, and (2) HbA1c < 53 mmol/mol (7.0%) with no symptomatic hypoglycemia.
Body weight was measured in duplicate with a standardized digital scale. Sitting BP was measured in triplicate using an automated oscillometric BP measuring device. HOMA-β was calculated by the University of Oxford method [11], using FPG and fasting C-peptide levels measured at baseline and week 52.
Safety Assessments
Safety assessments included the incidence of adverse events (AEs), including AEs of special interest (symptomatic hypoglycemia [episodes with clinical symptoms reported by the investigator as hypoglycemia; biochemical documentation not required], AEs associated with urinary tract infection [UTI], genital mycotic infection [GMI] [by gender], and hypovolemia). Documented hypoglycemia (episodes with a glucose level ≤ 3.9 mmol/L [70 mg/dL] with or without symptoms) and severe hypoglycemia (episodes that required medical or non-medical assistance) were recorded. Changes over time in laboratory parameters (including eGFR, low-density lipoprotein cholesterol [LDL-C], and high-density lipoprotein cholesterol [HDL-C]) were also assessed.
Statistical Analyses
With a non-inferiority margin of 3.3 mmol/mol (0.3%), and assuming a true mean difference in HbA1c of 0 mmol/mol, randomization of approximately 1230 patients (410 patients per group, to yield a sample size of 337 per group at week 52) was estimated to provide 97% power to demonstrate non-inferiority of a given ertugliflozin dose to glimepiride in HbA1c reduction at week 52.
Non-inferiority in terms of HbA1c reduction was declared if the upper limit of the two-sided 95% confidence interval (CI) for the mean difference between ertugliflozin and glimepiride at week 52 was less than the non-inferiority margin of 3.3 mmol/mol (0.3%). The efficacy hypotheses were tested using an ordered testing procedure (Supplementary Table S1). Hypothesis testing stopped when the first test in the ordered procedure failed to meet its success criterion. Comparisons involving other efficacy endpoints, not included in the ordered testing procedure, were supportive; no multiplicity adjustment was performed on these other comparisons.
Efficacy analyses excluded results following initiation of glycemic rescue therapy to avoid the confounding influence of rescue therapy. The full analysis set (FAS; all randomized patients who took at least one dose of study drug and had at least one measurement of the respective endpoint) was the primary population for efficacy analyses. A longitudinal data analysis (LDA) model was used to evaluate continuous endpoints in the FAS, with terms for treatment, AHA status (monotherapy or dual therapy) at screening, baseline eGFR, time (categorical), and the interaction of time by treatment with a constraint that the true mean at baseline is common to all treatment groups (which is valid owing to randomization) [12]. Logistic regression was used to evaluate the proportion of patients with HbA1c < 53 mmol/mol (7.0%), with the model including terms for treatment and baseline HbA1c, and missing data imputed via multiple imputation using the LDA model described above. The pre-specified composite endpoints were analyzed using the Miettinen and Nurminen method in the FAS population [13], with missing data imputed using the last observation carried forward method. HbA1c reduction from baseline at week 52 was assessed in categorical subgroups using a repeated measures analysis of covariance (ANCOVA) model.
Sensitivity analyses were conducted for the primary and key secondary efficacy endpoints in the per protocol (PP) population (all randomized patients who took at least one dose of study medication, with a measurement of the analysis endpoint at both baseline and week 52, and without significant protocol deviations) with an ANCOVA model, which included treatment, prior AHA medication, baseline eGFR, and baseline value.
Safety analyses included all randomized, treated patients. Data following initiation of glycemic rescue were included for the analysis of serious AEs (SAEs), discontinuations due to AEs, and excluded for the other endpoints. p values and 95% CIs for between-group differences in pre-specified AEs of special interest were calculated using the Miettinen and Nurminen method [13]. Percentage change from baseline for LDL-C and HDL-C was assessed using the LDA model described above. Changes from baseline in laboratory, vital signs, and other safety endpoints were summarized descriptively.
Results
The study was conducted at 232 centers across 16 countries (Argentina, Canada, Czech Republic, Hungary, South Korea, Lithuania, Mexico, the Philippines, Poland, Romania, Russia, Slovakia, South Africa, Taiwan, Ukraine, and the USA). The study started on December 17, 2013, and the last patient completed phase A on April 28, 2016.
Patient Disposition and Baseline Characteristics
In total, 1326 patients were randomized and 1325 analyzed (one patient randomized to ertugliflozin 15 mg did not receive treatment; Fig. 1). A total of 1161 patients (87.6%) completed phase A of the study; 357 (81.0%), 340 (75.9%), and 348 (79.6%) in the ertugliflozin 15 mg, ertugliflozin 5 mg, and glimepiride groups, respectively, completed phase A on study medication. More patients discontinued study medication in the ertugliflozin 5 mg group; compared with the other two groups, excess discontinuations were primarily related to hyperglycemia and non-compliance with study drug.
Baseline demographics were generally similar between groups, except for a lower percentage of male patients in the ertugliflozin 15 mg group (Table 1). The mean duration of T2DM was 7.5 years, mean baseline HbA1c 61.7 mmol/mol (7.8%), mean FPG 8.9 mmol/L (161.0 mg/dL), and mean eGFR 87.2 mL/min/1.73 m2.
Efficacy
Primary and Key Secondary Endpoints
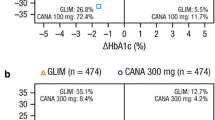
At week 52, clinically meaningful reductions from baseline in HbA1c were observed in all treatment groups (Fig. 2a). Reductions were observed in all groups at week 6 (first post-randomization visit). Further reductions were observed in all three treatment groups at week 12. In the glimepiride group, at week 12 reductions in HbA1c were greater than in the ertugliflozin groups, and reached a nadir at weeks 18 and 26, after which a progressive rise occurred through week 52. The mean and median doses of glimepiride were 3.0 mg.
The least squares (LS) mean HbA1c changes (95% CI) from baseline at week 52 were − 7.0 (− 7.9, − 6.0), − 6.1 (− 7.1, − 5.1), and − 8.1 (− 9.0, − 7.1) mmol/mol (− 0.6% [− 0.7, − 0.5], − 0.6% [− 0.6, − 0.5], and − 0.7% [− 0.8, − 0.7]) in the ertugliflozin 15 mg, ertugliflozin 5 mg, and glimepiride groups, respectively (FAS population). The LS mean difference (95% CI) between ertugliflozin 15 mg and glimepiride at week 52 was 1.1 mmol/mol (− 0.2, 2.5) (0.1% [− 0.0, 0.2]). Ertugliflozin 15 mg met the pre-specified criterion for non-inferiority to glimepiride in reducing HbA1c, as the upper bound of the 95% CI around the treatment difference was less than 3.3 mmol/mol (0.3%). The LS mean (95% CI) between-group difference for ertugliflozin 5 mg and glimepiride at week 52 was 2.0 mmol/mol (0.6, 3.3) (0.2% [0.1, 0.3]). As the upper confidence bound was not less than 3.3 mmol/mol (0.3%) for the 5 mg dose, ertugliflozin 5 mg did not satisfy the criterion for non-inferiority to glimepiride. The ordered testing procedure stopped with the comparison of ertugliflozin 5 mg to glimepiride on HbA1c (Supplementary Table S1). As such, p values only denote significance for comparisons for ertugliflozin 15 mg to glimepiride for HbA1c, body weight, and symptomatic hypoglycemia. All other p values are provided for descriptive purposes only (i.e., not used to declare statistical significance).
In pre-specified sensitivity analyses conducted in the PP population, the upper bounds of the 95% CIs around the differences in LS mean HbA1c reduction between ertugliflozin and glimepiride were less than the non-inferiority margin of 3.3 mmol/mol (0.3%) for both ertugliflozin 15 mg and 5 mg (LS mean difference from glimepiride: 1.28 mmol/mol [− 0.09, 2.65], [0.12% (− 0.01, 0.24)], and 1.84 mmol/mol [0.45, 3.22] [0.17% (0.04, 0.29)], respectively).
Both ertugliflozin doses and glimepiride provided generally similar and consistent mean reductions from baseline HbA1c in a variety of patient subgroups; greater reductions were observed in the subgroups with higher vs. lower baseline HbA1c values (Supplementary Table S2).
At week 52, 38.0%, 34.4%, and 43.5% of patients in the ertugliflozin 15 mg, ertugliflozin 5 mg, and glimepiride groups, respectively, had an HbA1c < 53 mmol/mol (7.0%) (Table 2).
Greater reductions from baseline in body weight were observed at week 52 in the ertugliflozin groups compared with glimepiride (Fig. 2b). The LS mean changes (95% CI) in body weight from baseline at week 52 were − 3.4 kg (− 3.7, − 3.0), − 3.0 kg (− 3.3, − 2.6), and 0.9 kg (0.6, 1.3) in the ertugliflozin 15 mg, ertugliflozin 5 mg, and glimepiride groups, respectively (Fig. 2b). The LS mean differences (95% CI) versus glimepiride at week 52 were − 4.3 kg (− 4.8, − 3.8) and − 3.9 kg (− 4.4, − 3.4) for ertugliflozin 15 mg and 5 mg, respectively (p < 0.001 vs. glimepiride).
Relative to glimepiride, greater reductions from baseline in SBP were observed in the ertugliflozin groups at week 52 (Fig. 2c). LS mean changes from baseline at week 52 were − 3.8 mmHg (− 4.9, − 2.7), − 2.2 mmHg (− 3.4, − 1.1) and 1.0 mmHg (− 0.1, 2.1) in the ertugliflozin 15 mg, ertugliflozin 5 mg, and glimepiride groups, respectively. The LS mean differences (95% CI) versus glimepiride at week 52 were − 4.8 mmHg (− 6.3, − 3.2) and − 3.2 mmHg (− 4.7, − 1.7) for ertugliflozin 15 mg and 5 mg, respectively (p < 0.001 vs. glimepiride). Reductions from baseline in DBP were also observed in the ertugliflozin groups compared with the glimepiride group (p < 0.05; Table 2; Fig. 2e).
Other Secondary Endpoints
FPG reductions were seen across all treatment groups. Relative to glimepiride, greater reductions from baseline in FPG were observed at week 52 with ertugliflozin 15 mg but not with ertugliflozin 5 mg, where reductions were similar to glimepiride (Table 2; Fig. 2d).
In the ertugliflozin groups, a higher percentage of patients met the composite endpoint of a HbA1c decrease > 5.5 mmol/mol (0.5%) at week 52 with no symptomatic hypoglycemia and no body weight gain compared with the glimepiride group (p < 0.001; Table 2). The percentage of patients meeting the composite endpoint of HbA1c < 53 mmol/mol (7.0%) at week 52 with no symptomatic hypoglycemia was similar between groups (Table 2).
LS mean increases from baseline in HOMA-β (%) at week 52 were smaller in the ertugliflozin groups compared with the glimepiride group (p < 0.05; Table 2). Reductions in the proinsulin/C-peptide ratio were observed across all groups, with a larger decrease in the ertugliflozin groups versus glimepiride (p < 0.001; Table 2).
A small percentage of patients required glycemic rescue in each group (ertugliflozin 15 mg, 3.6%; ertugliflozin 5 mg, 5.6%; glimepiride, 3.2%).
Safety
The percentage of patients with at least one AE was similar across groups (Table 3). Drug-related AEs were driven largely by GMI AEs. The incidence of SAEs was greater in the ertugliflozin 5 mg group, compared with the ertugliflozin 15 mg and glimepiride groups; this slight imbalance was not due to any specific SAE. In the three treatment groups, SAEs were distributed across multiple system organ classes, and only two SAEs occurred in more than one patient in a treatment group, including pneumonia (ertugliflozin 5 mg, n = 2; glimepiride, n = 1) and cerebrovascular accident (ertugliflozin 5 mg, n = 2; glimepiride, n = 1). The incidence of AEs leading to discontinuation was similar across groups. Seven deaths (1 [0.2%], 5 [1.1%], and 1 [0.2%] in the ertugliflozin 15 mg, ertugliflozin 5 mg, and glimepiride groups, respectively) were reported during the study (including the treatment and post-treatment periods). None of the deaths was considered by the investigators to be drug-related, and there was no pattern in causes of deaths as determined by the reported AE terms.
The incidence of symptomatic hypoglycemia was lower in the ertugliflozin groups compared with the glimepiride group (Table 3). Severe hypoglycemia was reported in 1 (0.2%), 1 (0.2%), and 10 (2.3%) patients in the ertugliflozin 15 mg, ertugliflozin 5 mg, and glimepiride groups, respectively. Both events of severe hypoglycemia in the ertugliflozin groups had precipitating factors of skipped meals or snacks and resolved. One event resulted in a reduced level of consciousness, required medical assistance, and resolved in 10 min. The other required non-medical assistance and resolved within 30 min. Glucose values were not obtained for either event. The incidence of documented hypoglycemia (symptomatic or asymptomatic) was lower in the ertugliflozin 15 mg (8.2% [n = 36]) and 5 mg (5.6% [n = 25]) groups relative to glimepiride (27.2% [n = 119]).
The incidences of AEs related to GMIs were significantly greater in patients of both genders receiving ertugliflozin 15 mg or 5 mg (2.1–10.0%) than those receiving glimepiride (0–1.4%; Table 3). The incidences of AEs related to UTIs and hypovolemia were similar across groups (Table 3).
At the first post-randomization assessment (week 6), modest reductions from baseline in eGFR were observed in the ertugliflozin groups; eGFR values returned to slightly above baseline by week 52 (Fig. 3). Overall, 4.7%, 3.7%, and 4.9% of patients in the ertugliflozin 15 mg, ertugliflozin 5 mg, and glimepiride groups, respectively had a decrease from baseline of greater than 30% in eGFR on at least one occasion. A low percentage (0.2–0.5%) of patients had a decrease of greater than 50% in eGFR from baseline across treatment groups. A total of 7 (1.6%), 3 (0.7%), and 2 (0.5%) patients in the ertugliflozin 15 mg, ertugliflozin 5 mg, and glimepiride groups, respectively, had at least one AE of decreased renal function (i.e., eGFR decreased and/or serum creatinine increased); the majority of these events were non-serious and mild-to-moderate in intensity, except for an SAE of acute kidney injury in the ertugliflozin 15 mg group which led to discontinuation of study medication and subsequently resolved. In total, three patients in the ertugliflozin 15 mg group and none in the other groups discontinued study drug as a result of AEs of decreased eGFR.
Greater increases from baseline in HDL-C at week 52 were observed in the ertugliflozin groups compared with the glimepiride group (Supplementary Table S3). A trend toward a greater increase from baseline in LDL-C at week 52 was observed in the ertugliflozin groups compared with the glimepiride group. Mean increases in hemoglobin of 0.5 g/dL were observed in both ertugliflozin groups compared with a reduction of 0.1 g/dL in the glimepiride group at week 52.
Four fractures were reported and confirmed by the adjudication committee, two in patients receiving ertugliflozin 15 mg (lower extremity fractures sustained from falls), one in a patient receiving ertugliflozin 5 mg (hand fracture resulting from a trap injury), and one in a patient receiving glimepiride (resulting from a twisted ankle).
One case of diabetic ketoacidosis in the ertugliflozin 15 mg group was identified in a 56-year-old woman with concurrent Klebsiella sepsis. The study medication was discontinued. The acidosis resolved with treatment of the Klebsiella. No event of pancreatitis was reported in this study. Toe amputations occurred in two patients, one in the ertugliflozin 15 mg group (history of neuropathy and peripheral vascular disease) and one in the glimepiride group (history of neuropathy and atherosclerosis).
Discussion
In this multicenter, randomized, double-blind, phase III clinical study (VERTIS SU), ertugliflozin 15 mg was non-inferior to glimepiride in lowering HbA1c from baseline at week 52. Clinically meaningful reduction in HbA1c was also observed with ertugliflozin 5 mg at week 52, although this reduction did not meet the pre-specified criterion for non-inferiority to glimepiride. In most regions of the world, it is anticipated that ertugliflozin will be a titrated medication, where up-titration to 15 mg will be allowed for patients tolerating the 5 mg starting dose who need additional glycemic control. Reductions in HbA1c were sustained through week 52. Subgroup analyses showed greater reductions in HbA1c from baseline with higher baseline HbA1c values for ertugliflozin and glimepiride.
Limited dose-ranging data available for glimepiride indicate that a 1 mg/day dose may provide nearly two-thirds of maximal efficacy of the agent and that near maximal efficacy is reached with a 4 mg/day dose [14]. In this study, investigators were to up-titrate glimepiride in patients if a defined glycemic goal was not met, risk of hypoglycemia was low, and there were no other contraindications. The dose should also have been down-titrated in the event of hypoglycemia. It may be for these reasons that the mean and median doses of glimepiride observed in this study (3 mg/day) approximated the dose of near maximal efficacy.
Weight gain was seen with glimepiride, while ertugliflozin led to reductions in body weight, which were sustained through week 52 (glimepiride-adjusted reductions of 4.3 kg and 3.9 kg in the ertugliflozin 15 mg and 5 mg groups, respectively). Similarly, BP reductions were observed with ertugliflozin compared with glimepiride. The incidence of hypoglycemia was lower with ertugliflozin relative to glimepiride, including a lower risk for severe hypoglycemia. Furthermore, a higher proportion of patients receiving ertugliflozin met the composite endpoint of HbA1c reduction of greater than 5.5 mmol/mol (0.5%), no body weight gain, and no symptomatic hypoglycemia compared with glimepiride, suggesting that ertugliflozin provides additional benefits beyond glycemic control.
The findings reported here are consistent with those comparing other SGLT2 inhibitors with SUs in patients inadequately controlled on background metformin therapy, in which non-inferiority after 52 weeks of treatment was observed [15,16,17].
The safety profile of ertugliflozin was generally consistent with that reported in other studies from the phase III VERTIS program [6,7,8]. There were greater incidences of SAEs in the ertugliflozin groups, and more deaths in the ertugliflozin 5 mg group than in the glimepiride group in this study, which was not observed in other studies with ertugliflozin [6,7,8]. No discernible pattern of SAEs or deaths was observed. None of the deaths was considered related to study medication. Both ertugliflozin doses were associated with a higher incidence of GMIs relative to glimepiride, as previously reported in a similar study evaluating another SGLT2 inhibitor [15]. The incidences of UTIs and hypovolemia AEs were not meaningfully different between groups. Overall, the safety profiles of the two doses were not meaningfully different.
SGLT2 inhibitors result in transient decreases in eGFR, which are likely to be hemodynamically mediated [18]. In this study, in both ertugliflozin groups, mean eGFR values decreased from baseline by week 6, but were above baseline and trending greater than in the glimepiride group by week 39.
This non-inferiority study did not include a placebo control group; however, in a separate study (VERTIS MET) comparing ertugliflozin with placebo as add-on to metformin therapy in patients with T2DM, addition of ertugliflozin led to significant improvements in glycemic control (placebo-adjusted reductions in HbA1c of 9.6 mmol/mol [0.9%] and 7.7 mmol/mol [0.7%] for the 15 mg and 5 mg doses, respectively), body weight, and BP [7]. Another study limitation is the possibility that the maximum tolerable dose of glimepiride was not used in every patient. While investigators were encouraged to follow a protocol-defined algorithm recommending dose titration, up-titration was not forced by the protocol.
Conclusion
Addition of ertugliflozin 15 mg to metformin therapy was non-inferior to addition of glimepiride in lowering HbA1c after 52 weeks of treatment. Both doses of ertugliflozin provided clinically meaningful glycemic control and led to weight loss and reductions in BP. Relative to glimepiride, ertugliflozin had a lower incidence of symptomatic hypoglycemia, documented, and severe hypoglycemia, but a higher incidence of GMIs. Taken together, the results reported here suggest that ertugliflozin is an alternative to SUs for patients with T2DM with inadequate glycemic control on metformin therapy.
References
American Diabetes Association. Standards of medical care in diabetes. Diabetes Care. 2017;40:S1–135.
Belsey J, Krishnarajah G. Glycaemic control and adverse events in patients with type 2 diabetes treated with metformin + sulphonylurea: a meta-analysis. Diabetes Obes Metab. 2008;10(Suppl 1):1–7.
Andersen SE, Christensen M. Hypoglycaemia when adding sulphonylurea to metformin: a systematic review and network meta-analysis. Br J Clin Pharmacol. 2016;82:1291–302.
González-Ortiz M, Guerrero-Romero J, Violante-Ortiz R, et al. Efficacy of glimepiride/metformin combination versus glibenclamide/metformin in patients with uncontrolled type 2 diabetes mellitus. J Diabetes Complicat. 2009;23:376–9.
Paneni F, Luscher TF. Cardiovascular protection in the treatment of type 2 diabetes: a review of clinical trial results across drug classes. Am J Cardiol. 2017;120:S17–27.
Terra SG, Focht K, Davies M, et al. Phase III, efficacy and safety study of ertugliflozin monotherapy in people with type 2 diabetes mellitus inadequately controlled with diet and exercise alone. Diabetes Obes Metab. 2017;19:721–8.
Rosenstock J, Frias J, Pall D, et al. Effect of ertugliflozin on glucose control, body weight, blood pressure and bone density in type 2 diabetes mellitus inadequately controlled on metformin monotherapy (VERTIS MET). Diabetes Obes Metab. 2017. https://doi.org/10.1111/dom.13103.
Dagogo-Jack S, Liu J, Eldor R, et al. Efficacy and safety of the addition of ertugliflozin in patients with type 2 diabetes mellitus inadequately controlled with metformin and sitagliptin: the VERTIS SITA2 placebo-controlled randomized study. Diabetes Obes Metab. 2017. https://doi.org/10.1111/dom.13116.
Nauck MA. Update on developments with SGLT2 inhibitors in the management of type 2 diabetes. Drug Des Devel Ther. 2014;8:1335–80.
Grunberger G, Camp S, Johnson J, et al. Ertugliflozin in patients with stage 3 chronic kidney disease and type 2 diabetes mellitus: the VERTIS RENAL randomized study. Diabetes Ther. 2017. https://doi.org/10.1007/s13300-017-0337-5.
University of Oxford. HOMA calculator, 2004. http://www.dtu.ox.ac.uk/homacalculator/. Accessed Oct 16, 2017.
Liang K-Y, Zeger S. Longitudinal data analysis of continuous and discrete responses for pre-post designs. Sankhya Ser B. 2000;62:134–48.
Miettinen O, Nurminen M. Comparative analysis of two rates. Stat Med. 1985;4:213–26.
Goldberg RB, Holvey SM, Schneider J. A dose-response study of glimepiride in patients with NIDDM who have previously received sulfonylurea agents. The Glimepiride Protocol #201 Study Group. Diabetes Care. 1996;19:849–56.
Cefalu WT, Leiter LA, Yoon KH, et al. Efficacy and safety of canagliflozin versus glimepiride in patients with type 2 diabetes inadequately controlled with metformin (CANTATA-SU): 52 week results from a randomised, double-blind, phase 3 non-inferiority trial. Lancet. 2013;382:941–50.
Ridderstrale M, Andersen KR, Zeller C, Kim G, Woerle HJ, Broedl UC. Comparison of empagliflozin and glimepiride as add-on to metformin in patients with type 2 diabetes: a 104-week randomised, active-controlled, double-blind, phase 3 trial. Lancet Diabetes Endocrinol. 2014;2:691–700.
Nauck M, del Prato S, Meier JJ, et al. Dapagliflozin versus glipizide as add-on therapy in patients with type 2 diabetes who have inadequate glycemic control with metformin. Dtsch Med Wochenschr. 2013;138(Suppl 1):S6–15.
Kalra S, Singh V, Nagrale D. Sodium-glucose cotransporter-2 inhibition and the glomerulus: a review. Adv Therapy. 2016;33:1502–18.
Acknowledgements
The authors wish to thank the investigators, staff, and participants in the VERTIS SU study (protocol MK-8835-002). Statistical support was provided by Deng Wang, MSc of MSD China, Beijing and funded by Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc., Kenilworth, NJ, USA. Data from this study were previously presented at the 53rd Annual Meeting of the European Association for the Study of Diabetes (Lisbon, Portugal, Abstract No 38).
Funding
Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc., Kenilworth, NJ, USA, in collaboration with Pfizer Inc., provided financial support for this study. Merck Sharp & Dohme Corp., a subsidiary of Merck & Co, Inc., Kenilworth, NJ, USA, provided funding for article processing charges for this publication. All authors had full access to all of the data in this study and take complete responsibility for the integrity of the data and accuracy of the data analysis.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval for the version to be published.
Medical Writing Assistance
Medical writing support, including assisting authors with the development of the initial draft, incorporation of comments, fact checking, and referencing, was provided by Jason Hoffman, PharmD and Camille Bonomelli, PhD and editorial support, including figure preparation, formatting, proof reading, and submission, was provided by Nicola Jenkins, MA (all of Scion, London, UK). This assistance was funded by Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc., Kenilworth, NJ USA. Ed O’Neill, PhD (Merck & Co., Inc., Kenilworth, NJ, USA) provided additional editing. The sponsor was involved in the study design, collection, analysis, and interpretation of data, as well as data checking of information provided in the manuscript. However, ultimate responsibility for opinions, conclusions, and data interpretation lies with the authors.
Disclosures
Priscilla Hollander received funding and honoraria from Merck & Co., Inc., Kenilworth, NJ, USA. Jie Liu is an employee of Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc., Kenilworth, NJ, USA, and may own stock and/or hold stock options in the company. Julie Hill is an employee of Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc., Kenilworth, NJ, USA, and may own stock and/or hold stock options in the company. Jeremy Johnson is an employee of Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc., Kenilworth, NJ, USA, and may own stock and/or hold stock options in the company. Gregory Golm is an employee of Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc., Kenilworth, NJ, USA, and may own stock and/or hold stock options in the company. Susan Huyck is an employee of Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc., Kenilworth, NJ, USA, and may own stock and/or hold stock options in the company. Samuel S. Engel is an employee of Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc., Kenilworth, NJ, USA, and may own stock and/or hold stock options in the company. Brett Lauring is an employee of Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc., Kenilworth, NJ, USA, and may own stock and/or hold stock options in the company. Zhi Wei Jiang was an employee of MSD R&D (China) Co., Ltd., a subsidiary of Merck & Co., Inc., Kenilworth, NJ, USA at the time the study was conducted and may own stock and/or hold stock options in the company. Steven G. Terra and James P. Mancuso are employees and shareholders, Pfizer Inc.
Author Contributions
JH, JJ, GG, JPM, SSE, and BL contributed to the conception and design of the study. JH, JJ, and BL collected data. PH, JL, ZWJ, GG, SH, SGT, JPM, SSE, and BL contributed to the analysis and interpretation of data. All authors drafted the article or revised it critically for important intellectual content and provided final approval of the published version. Authors are responsible for the work described in this paper. All authors reviewed the manuscript for important intellectual content and provided final approval of the version to be published. All authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Compliance with Ethics Guidelines
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964, as revised in 2013. It was conducted in accordance with the principles of good clinical practice and approved by the appropriate institutional review boards and regulatory agencies. Informed consent was obtained from all individual participants included in the study. The protocol and statistical analysis plan were developed by the sponsors in consultation with an external Scientific Advisory Committee.
Data Availability
Merck & Co., Inc.’s data sharing policy, including restrictions, is available at http://engagezone.merck.com/ds_documentation.php. Requests for access to the study data can be submitted through the EngageZone site or via email to dataaccess@merck.com.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Author information
Authors and Affiliations
Corresponding author
Additional information
Enhanced content
To view enhanced content for this article go to http://www.medengine.com/Redeem/BEFCF06006781336.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0), which permits use, duplication, adaptation, distribution, and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Hollander, P., Liu, J., Hill, J. et al. Ertugliflozin Compared with Glimepiride in Patients with Type 2 Diabetes Mellitus Inadequately Controlled on Metformin: The VERTIS SU Randomized Study. Diabetes Ther 9, 193–207 (2018). https://doi.org/10.1007/s13300-017-0354-4
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-017-0354-4