Abstract
Indicated to manage a variety of disorders affecting the female genital tract, hysterectomy represents the second most common gynaecological operation after caesarean section. Performed via an open, laparoscopic or vaginal approach, hysterectomy is associated with non-negligible morbidity and occasional mortality. Iatrogenic complications represent a growing concern for gynaecologists and may result in prolonged hospitalisation, need for interventional procedures or repeated surgery, renal impairment and malpractice claims. As a result, radiologists are increasingly requested to investigate patients with suspected complications after hysterectomy. In the vast majority of early postoperative situations, multidetector CT represents the ideal modality to comprehensively visualise the surgically altered pelvic anatomy and to consistently triage the varied spectrum of possible injuries. This pictorial review provides an overview of current indications and surgical techniques, illustrates the expected CT appearances after recent hysterectomy, the clinical and imaging features of specific complications such as lymphoceles, surgical site infections, haemorrhages, urinary tract lesions and fistulas, bowel injury and obstruction. Our aim is to increase radiologists’ familiarity with normal post-hysterectomy findings and with post-surgical complications, which is crucial for an appropriate choice between conservative, interventional and surgical management.
Teaching points
• Hysterectomy via open, laparoscopic or vaginal route is associated with non-negligible morbidity.
• Multiplanar CT imaging optimally visualises the surgically altered pelvic anatomy.
• Familiarity with early post-hysterectomy CT and expected findings is warranted.
• Complications encompass surgical site infections, haemorrhages, bowel injury and obstruction.
• Urological complications include ureteral leakage, bladder injury, urinomas and urinary fistulas.
Similar content being viewed by others
Introduction
Background
Performed to manage several different disorders of the female reproductive system, hysterectomy (surgical removal of the uterus) represents one of the most prevalent surgeries worldwide and the second most common gynaecological operation after caesarean section. The annual hysterectomy rates vary among different countries in the range 1.2 to 4.8/1000 women. In the USA, approximately 600,000 such operations are performed each year [1].
Although the majority of women experience an uneventful postoperative course, hysterectomy is associated with non-negligible risks. Potentially serious postoperative complications such as infections, haemorrhage, urinary and bowel injuries may be either recognised intraoperatively, manifest during postoperative hospitalisation, or sometimes become apparent weeks or months later [2,3,4,5].
Aim
Transvaginal ultrasound represents the first-line modality to investigate the female genital organs. However, in recently operated patients this modality is cumbersome and poorly tolerated, and provides a limited field of view. In our experience, partly due to fear of litigation, radiologists are increasingly requested to investigate suspected iatrogenic complications after hysterectomy. During the last decade, multidetector CT has become the mainstay technique to assess the vast majority of postoperative abdominal and pelvic conditions, as it rapidly and comprehensively visualises the surgically altered anatomy and can triage the varied spectrum of possible complications [6,7,8,9].
This pictorial essay provides an overview of current indications and surgical techniques, then reviews and illustrates the expected postoperative CT findings, and common and unusual specific complications after hysterectomy. Our aim is to provide radiologists with an increased familiarity in the interpretation of early post-hysterectomy CT studies, thus providing a consistent basis for correct therapeutic choice and ultimately helping to decrease morbidity [7, 9].
Overview of hysterectomy
Techniques and indications
The uterus may be removed using three different routes, namely vaginal, abdominal and laparoscopic. The indications of different surgical techniques are summarised in Table 1.
Although declining, abdominal hysterectomy (AH) continues to be the most widely used approach (60–64% of all operations) worldwide. AH begins with a transverse suprapubic laparotomic incision of the anterior abdominal wall, involves dissection and removal of the uterus, and ends with suture of the vaginal cuff (VC). Radical AH for tumours is completed with removal of the adnexa (salpingo-oophorectomy), lymphadenectomy, peritoneal exploration and lavage [10, 11].
Worldwide, the majority (90%) of hysterectomies are performed to treat non-neoplastic conditions which negatively impact women’s quality of life, such as bleeding leiomyomas and hypermenorrhoea. In recent years, hysterectomy rates are declining in Western countries after introduction of several alternative therapeutic options for benign diseases, such as hormonal medications, intrauterine levonorgestrel-releasing devices, endometrial ablation techniques, hysteroscopic and surgical myomectomy, ultrasound focused energy and transcatheter uterine artery embolisation. However, leiomyomas still account for approximately 40–62% of all hysterectomies [1, 12,13,14,15].
For benign disorders requiring hysterectomy, according to the American College of Obstetricians and Gynaecologists guidelines, criteria for choosing the surgical route include surgeon’s skill and training, parity, size and shape of the vagina and uterus, accessibility to the uterus (e.g. prolapse, pelvic adhesions), underlying pathological condition and presence of extrauterine disease [14].
In vaginal hysterectomy (VH) the uterus is approached, excised, anteverted and extracted via the vagina. Being the safest technique, unless contraindicated, VH should be the preferred approach in the majority of patients with non-malignant disorders, particularly genital prolapse [12,13,14, 16].
Laparoscopy is increasingly used as a minimally invasive alternative to AH for those patients in whom VH is contraindicated or technically challenging, and currently accounts for 14% of all hysterectomies in the USA. The technically challenging total laparoscopic hysterectomy (TLH) is differentiated from laparoscopically-assisted VH (LAVH), which is completed with removal of the uterus via the vagina. Compared to AH, both VH and laparoscopy result in shorter hospitalisation, less postoperative pain and fever, and faster return to normal activities. On the other hand, laparoscopy requires specific surgeons’ training and the longest operating time of all techniques [1, 2, 12, 15].
Complications
The overall morbidity and mortality rates associated with different hysterectomy techniques are summarised in Table 2. Both prevalence of major complications at 30 postoperative days and mortality are highest after radical hysterectomy for cancer. Conversely, the composite morbidity is much lower in VH compared to AH, and in patients operated with every technique for benign disease, the 40-day mortality is approximately 1/1000. General risk factors for post-hysterectomy morbidity included advanced age, medical comorbidities and malignancy [3].
Regarding the type of complications, systemic and cardiorespiratory events such as venous thromboembolism, myocardial infarction, pneumonia, sepsis and fluid/metabolic imbalance may develop after hysterectomy similarly to other surgeries. Clinically manifest thromboembolic disease and pneumonia are reported in 1–4% and 2% of patients, respectively [2,3,4,5, 12].
Patterns and incidence of specific complications partly differ between the three surgical approaches (Table 3). The commonest category is postoperative infections, which affect 9–13% of patients after hysterectomy with every technique and encompass surgical site, urinary tract, systemic and wound infections. The latter occur in 1–6% of patients, particularly after AH. Vaginal vault haematoma and lymphocele are typically associated with VH and radical AH, respectively. The incidence of significant bleeding requiring transfusions is in the range 2–5% with every technique. The next most frequent category is urologic injuries, which occur most usually after TLH (3–6.2%), LAVH (3.06%) and radical AH (2.78%). The uncommon VC dehiscence mostly develops after TLH (1.35%) rather than LAVH, AH and VH in descending order of frequency. With every technique, potentially severe injuries to the gastrointestinal tract occur in less than 1% (roughly 0.2–0.3%) of patients [2,3,4,5, 12].
Early post-hysterectomy CT
Indications and techniques
In our experience, the usual indications for obtaining urgent post-hysterectomy CT imaging are listed in Table 4, and are often multiple in each patient.
Since pleuropulmonary changes (such as atelectasis, pneumonia and pleural effusions) are commonly encountered, after recent hysterectomy the CT acquisition should encompass the entire abdomen from the lung bases to the inferior contour of the gluteus muscles. A comprehensive CT study including intravenous contrast medium (CM) injection is warranted unless strongly contraindicated. In patients with impaired renal function or allergy, appropriate measures are recommended such as intravenous hydration or pharmacological premedication, following guidelines from the European Society of Urogenital Radiology [17].
Following recent hysterectomy, we generally recommend a multiphase protocol, including a preliminary unenhanced acquisition, aiming to identify high attenuation values consistent with recent blood at the vaginal vault, in the pelvis and peritoneal cavity. After automated power injection of 110–130 ml of iodinated CM (dose may be calculated on the basis of lean body weight and CM iodine concentration) such as iopromide (370 mgI/ml), iomeprol (350 mgI/ml) or iodixanol (300 mgI/ml) at a 2.5 to 4-ml/s flow rate, we usually acquire arterial phase scanning using a bolus tracking technique with a region of interest in the infrarenal aorta, a 10-s delay and a 120-Hounsfield units (HU) threshold. Aimed at detecting active haemorrhage, the arterial phase (CT angiography) may be obviated to limit the radiation dose if haemoglobin levels tend to improved during the first postoperative days. The mandatory portal-venous phase acquisition is obtained after 75–80 s after start of CM injection. At the attending radiologist’s discretion, excretory phase may be acquired after injection of 200 ml of saline and 8–10 min of delay, to visualise the opacified urinary cavities. Additional very delayed acquisition (20 min to 1 h) may be warranted if urinary tract injury or urinoma are suspected [7, 9].
Additionally, in patients with clinical suspicion of iatrogenic bladder injury or fistulisation multidetector CT cystography acquired after drop infusion of 1:10 diluted CM through the Foley catheter represents the most accurate technique. The resulting acquisition should be reviewed along multiple planes at CT angiography window settings (width 600–900 HU, level 150–300 HU) [18]. Borrowing from experience with multidetector CT imaging of acute gynaecological diseases, also in the postoperative setting, routine reconstruction of 3–4-mm-thick contiguous images along sagittal and coronal planes is beneficial to elucidate the female pelvic anatomy [19,20,21].
Study interpretation and expected post-surgical appearances
After AH the vagina is best identified on mid-sagittal CT images, with the VC slightly retracted cranially compared to preoperative studies, a band- or H-shaped axial configuration, uniform walls and thin enhancing mucosa (Fig. 1). After recent hysterectomy, minimal pelvic effusion and gas are common postoperative findings. Following AH, air may either distribute freely in the peritoneal cavity or collect in the operated subperitoneal spaces, and typically resolves within a week but decreases on serial imaging. Conversely, air which persists or increases should raise concern for visceral perforation. Following laparoscopic surgery, the amount of expected intraperitoneal free gas is lower compared to AH because insufflated carbon dioxide is rapidly reabsorbed, and subcutaneous emphysema from insufflation in the abdominal wall is sometimes encountered [22,23,24].
A, B) Usual contrast-enhanced CT appearance after recent abdominal hysterectomy (AH), including a non-distended vagina (arrows) with slight upwards retraction of the vaginal dome in sagittal view (A), preserved band-like transverse configuration and thin mucosal enhancement (B), minimal presacral fluid. (Partially reproduced from open access ref. no [58])
After uncomplicated VH, we have consistently observed a characteristic CT appearance which reflects diffuse vaginal oedema, including a roundish configuration in transverse planes, circumferential oedematous mural thickening and marked mucosal enhancement (Fig. 2). When interpreting early post-hysterectomy CT studies, radiologists should thoroughly search for abnormal (bloody, fluid or abscess) collections at the surgical site above the closed VC.
Expected CT appearance 4 days after uncomplicated vaginal hysterectomy (VH) performed to treat genital prolapse (GP), in an 80-year-old female suffering from abdominal distension, vague pelvic pain and low-grade fever. Multiplanar contrast-enhanced images (A–C) show a moderately distended vagina (arrows) with loss of the usual transverse configuration, circumferential mural thickening and marked, uniform mucosal enhancement reflecting diffuse vaginal oedema. The patient was discharged without any additional treatment (Partially reproduced from open access ref. no [58])
CT imaging of post-hysterectomy complications
Vaginal vault haematoma
A typical sequel of VH, vaginal vault haematoma develops in up to 20–25% of patients, more frequently in premenopausal women with larger, more vascular uteri rather than in elderly woman with atrophic uteri. Diagnosed up to 7–14 days after VH, haematomas often manifest with fever, and are generally self-limiting but may require blood transfusions, prolongation of hospitalisation or readmission after discharge. Conversely, after AH and TLH, vaginal vault haematoma is rare and not associated with febrile morbidity [25,26,27].
At CT, median or paramedian haematomas generally measure 3 to 6 cm in size and are identified by their characteristic hyperattenuation. In CM-enhanced acquisition, the peripheral rim enhancement can be misleading as it may suggest an incorrect diagnosis of abscess (Fig. 3). However, in most cases, the gynaecologist is aware of this complication since it is easily detected clinically and sonographically [25,26,27].
Two cases of vaginal vault haematoma. A) Typical example of midline haematoma after VH for GP in a 40-year-old female: precontrast sagittal CT image showing 5-cm hyperattenuating (45–50 Hounsfield units, HU) mass-like structure (*) above the vaginal dome, causing compression of the bladder. B–D) in a 35-year-old female, following VH for menorrhagia, a smaller (3 × 2 cm) paramedian vaginal vault haematoma (*) shows mild precontrast (B) hyperattenuation (40 HU), peripheral enhancement after iv contrast (C, D), abutting the upper right aspect of the vaginal dome (arrows). Both occurrences were successfully managed conservatively. Note: lymphocele (+). (Partially reproduced from open access ref. no [58])
Lymphoceles
Lymphoceles are collections of lymphatic fluid which result from surgical injury to the lymphatic system. Strongly associated with lymph node dissection, uni- or bilateral lymphoceles are detected in up to 40% of patients after resection of gynaecologic tumours [4, 28] .
At CT, the characteristic appearance of a lymphocele is a laterally positioned pelvic collection with homogeneous fluid attenuation and signal intensity, generally adjacent to surgical clips and iliac blood vessels (Figs. 3 and 4). On early postoperative CT studies, lymphoceles lack a perceptible wall (Fig. 4a). Later on, lymphoceles progressively become round- or ovoid-shaped and better demarcated, and develop a thin regular contour which corresponds to the fibrotic wall without epithelial lining. Variably sized lymphoceles are generally asymptomatic and therefore incidentally found on cross-sectional imaging. The majority of cases tend to resolve spontaneously, may occasionally (20% of cases) persist 1 year after surgery and do not require treatment [28].
Usual CT appearance and short-time evolution of pelvic lymphoceles. A, B) Three days after AH for uterine body carcinoma, early CT (A) showed a fluid attenuation collection (*) without perceptible wall abutting the left external iliac vessels. Four weeks later, repeated CT (B) showed large left-sided lymphoceles (*) with unchanged homogeneous attenuation and development of a thin, regular wall. C, D) in another patient, early postoperative CT after radical AH showed a well-demarcated ovoid collection (*) with thin regular wall measuring 4 × 2.5 cm, adjacent to surgical clips (thin arrow in C) and left external iliac vessels
Some lymphoceles may cause ipsilateral lower limb oedema and pain, and may be treated by imaging-guided interventions. Percutaneous catheter drainage with and without sclerotherapy achieves technical success in 74.3% and 100% of cases, respectively. Recurrence occurs in up to 13% of patients and may require repeated drainage. Alternatively, open surgical or laparoscopic drainage and internal marsupialisation may be performed [29, 30].
Occasionally, complications such as deep venous thrombosis, bladder compression and superinfection may occur. The latter is heralded by fever, pelvic pain, leukocytosis and elevated acute phase reactants, and is suggested at imaging by enlargement of a known lymphocele, appearance of septations, internal inhomogeneity or by an abscess-like appearance with thickened enhancing walls (Fig. 5) [31].
Delayed superinfection of a lymphocele 9 months after radical AH in a 41-year-old female, suffering from recurrent fever after chemotherapy. Contrast-enhanced CT (A, B) showed a fluid-like collection with thick, enhancing wall (arrowheads) in the right lateral pelvis, in the site of a small lymphocele described in a previous ultrasound (not shown). Signs of iliac-femoral thrombosis were absent. Fever, laboratory and imaging abnormalities ultimately regressed after intensive antibiotics (Partially reproduced with permission from ref. no [59])
Surgical site infections
Infections result from ascending polymicrobial contamination of the surgical site from the vagina and endocervix. Specific risk factors include patient features (such as obesity, diabetes, malnutrition, advanced ages, steroid use, history of radiation and bacterial vaginosis) and operation-related factors including prolonged duration, blood loss and staple closure. Among them, VC cellulitis represents superficial infection at the vaginal suture margin, and typically present with 5–10 postoperative days with fever, abdominal pain and palpation without masses. Conversely, deep infections encompass pelvic cellulitis and abscesses, often manifest after discharge from the hospital with pelvic pain, purulent vaginal secretions, marked oedema, tenderness and a mass at physical examination. CT helpfully complements physical examination by demonstrating the extent and topography of pelvic abscesses (Fig. 6), which may sometimes result from superinfection of a conservatively treated haematoma, lymphocele or urinoma. If clinically unresponsive to intensive antibiotics, abscesses require percutaneous or laparoscopic drainage [32].
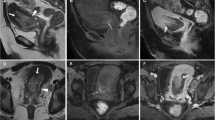
Multidetector CT appearances in two cases of surgical site infections. A–C) after recent laparoscopic hysterectomy (LH), clinical diagnosis of pelvic cellulitis corresponded to a bilobated fluid-like collection (*) with thin peripheral enhancement. D–F) after radical AH, a larger abscess (*) with peripheral enhancement (arrowheads) developed upwards from the normal-appearing vaginal dome (arrows) (Partially reproduced from open access ref. no [58])
Alternatively to infection, the presence of a fluid collection abutting the VC may occasionally correspond to VC dehiscence. Particularly in patients suffering from vaginal pain and bleeding, careful scrutiny of the VC for mural discontinuity and fat herniation is warranted to suggest to the gynaecologist the possibility of VC and request a focused physical examination [2, 9, 33].
The key CT differential diagnosis of a postoperative pelvic abscess is presence of oxidised regenerated cellulose (Surgicel®, Ethicon), a gauze-like bioabsorbable haemostatic material which mimics as a mixed gas-fluid collection and requires awareness of surgical details to avoid misinterpretation [34].
Finally, a peculiar condition underlying persistent postoperative fever is septic pelvic thrombophlebitis, which may result in systemic embolisation (to the lungs, brain and musculoskeletal system) if untreated [35, 36]. The CT findings include enlargement of hypogastric, iliac or femoral veins, with partial or complete luminal non-opacification, thickening and hyperenhancement of the vessel wall, and inflammatory stranding of the surrounding fat planes [9, 35, 37].
Haemorrhage
After hysterectomy, bleeding is one of the most feared complications. Haemorrhage from surgical manipulation or inadequate vessel ligation may extend from the surgical site to the pelvis and abdominal cavity. Alternatively, during laparoscopic surgery, the abdominal wall, mesenteric or inferior epigastric vessels may be injured by insertion of Veress needles or trocars [23, 24].
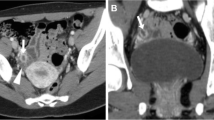
The use of CT is crucial to detect the presence, site, entity, age and features of iatrogenic haemorrhage. Haematomas are recognised by the characteristic 30–45-HU attenuation of fresh blood, which becomes even more hyperdense (HU > 60) after a few hours from clotting, and progressively develops inhomogeneity and fluid-fluid levels from mixing of clotted regions and serum from haemoglobin lysis. CT may reveal CM extravasation corresponding to active bleeding in either arterial or venous phase (Figs. 7 and 8) [7, 9].
Large pelvic haematoma developing within 48 h after LH for uterine myoma, manifesting with hypotension and severe haemoglobin drop. Axial precontrast CT image (A) showed abundant, strongly hyperattenuating (60–70 HU) blood. CT angiography (maximum-intensity reformation B) and venous-phase CT acquisition (C) did not show active contrast medium extravasation suggesting active bleeding. Repeated laparoscopy was required for drainage of the peritoneal cavity and haemostasis
Haemoperitoneum after LH for uterine myomas, manifesting the next day with worsening pelvic pain and blood loss. Precontrast CT (A, B) images showed haemoperitoneum (+) in the upper abdomen, and a vast hyperattenuating haematoma (*) occupying most of the pelvis, causing compression on the urinary bladder. CT angiography (C) and venous-phase CT acquisition (D) showed active arterial bleeding as serpiginous contrast medium extravasation (arrowheads). Open surgery confirmed presence of nearly 1 l of blood in the abdominal cavity and arterial haemorrhage from the left-sided angle of the vaginal vault and small vessels of the ipsilateral ovarian pedicle, which was treated by coagulation and suture (Partially reproduced from open access ref. no. [60])
If available, transarterial embolisation of the uterine or internal iliac artery is increasingly performed to control iatrogenic pelvic bleeding without repeated surgery [38].
Bowel injury and obstruction
Compared to postoperative ileus, bowel obstruction is relatively rare. Within and immediately after the postoperative hospitalisation, the most frequent cause is represented by incision and port site (Fig. 9) hernias developing respectively after open and laparoscopic surgery. Risk factors include advanced age, obesity, duration of surgery, use of large-bore trocars and ports for specimen removal. Due to the small size of the defect, both sites have a high likelihood of causing obstruction. Borrowing from experience with spontaneous acute abdomens, CT effectively triages presence and degree of obstruction, transition point (Fig. 9) and possible signs of strangulation [22,23,24].
Small-bowel obstruction developing after recent LH. The patient was readmitted with plain radiographic (A) evidence of distended bowel loops with multiple fluid-fluid levels. CT (B, C) confirmed distended jejunal and ileal loops with abundant intraluminal fluid, caused by herniation (arrowhead) into a laparoscopic trocar access site
Although very uncommon, iatrogenic intestinal injuries represent potentially serious complications, especially if unrecognised at the time of surgery. Delayed diagnosis corresponds to high risk of perforation, faecal peritonitis, sepsis and death. After both AH and VH, most injuries involve the rectum and sigmoid colon. Conversely, albeit incidence is similar, laparoscopic surgery may damage the small bowel during Veress needle or trocar insertion. Radiologists should suggest possible bowel injury when faced with abundant, persistent or increasing pneumoperitoneum, with peritonitis with effusion and enhancing serosa (Fig. 10), or with unexplained abscess collections. The rare but more specific signs include identification of focal bowel wall thickening, discontinuity (Fig. 11) or non-enhancement. Unfortunately, CT sensitivity is approximately 70%, and negative CT findings despite serious bowel complications have been reported [9, 39].
Post-hysterectomy urologic complications
Despite technical advancements and surgeons’ experience, due to the close anatomic relationship between the urinary and female genital tracts, urologic injuries represent typical complications of gynaecologic surgery and a potential cause of litigation. According to the European Association of Urology (EAU) guidelines, early recognition facilitates immediate repair, improves patients’ outcome and decreases the likelihood of long-term sequelae such as renal function impairment [8, 40].
General risk factors for urologic complications include obesity, diabetes, radical hysterectomy including lymph node dissection for malignancy, adhesions from previous surgeries and history of irradiation. In descending order of frequency, urologic injuries affect the urinary bladder (60–70% of cases), the ureter (24–30%) and the vagina (2.1%). Acute urologic injuries manifest during the first postoperative days with a combination of pelvic or flank pain, abdominal distension, ileus, peritonitis, fever, decreased urinary output, worsening renal function, haematuria and abnormal urinalysis [41,42,43,44,45,46,47,48].
Ureteral injuries
Mechanisms of iatrogenic damage to the ureters include direct manipulation, inadvertent ligation or kinking with a suture, thermal injury and ischaemia from devascularisation. In patients with distorted pelvic anatomy, prophylactic stenting is beneficial to decrease risks. Unfortunately, ureteral damage is unrecognised during hysterectomy in almost two thirds of patients and delayed diagnosis (weeks to months after surgery) with hydronephrosis and permanent loss of renal function is not unusual [8, 43, 44, 49, 50].
According to the EAU guidelines, appropriate therapeutic planning requires thorough assessment of the site, features and degree of ureteral injuries using excretory-phase CT [8]. The right and left ureters are injured with similar frequency. The typical (80–90% of cases) site of injury is the lower ureteral third, either at the pelvic brim or along the pelvic sidewall at uterine artery crossing. The main CT pattern of ureteral injury is partial or complete disruption, which is heralded by extravasation of urine (Figs. 12 and 13). Following recent hysterectomy, fluid-attenuation (0–20 HU) collections abutting the ureters should be viewed with suspect. The diagnosis of urinoma is confirmed by enhancement on excretory-phase scanning, with inhomogeneous opacification (denser close to the leaking source) which progresses on repeated delayed scanning. Preserved opacification of the ureteral segment distal to the leaking site allows differentiating partial lacerations from complete disruption [7, 9, 51,52,53].
Ureteral injury manifesting with fever and pelvic tenderness 3 days after TLH. Vaginal examination and sonography (not shown) detected a sizeable hypo-anechoic pelvic collection, initially interpreted as a vaginal vault haematoma, which rapidly increased in volume. CT confirmed a large fluid-attenuation collection (*) cranial to the urinary bladder and vagina, which in the excretory phase (B, C) was partially opacified by enhanced urine (arrowhead in B) leaking from the right ureter. The latter was opacified (arrow in C) distally to the injury, consistent with an incomplete laceration. Note surgical clips (thin arrows). Conservative treatment included ureteral stenting and prolonged catheterisation. A month later, follow-up CT (not shown) showed near-complete resolution of the urinoma (Partially reproduced with permission from ref. no [61])
Another case of ureteral injury shortly after LH. Despite preoperative bilateral ureteral stenting (thin arrows), unenhanced CT images (A) showed a mixed-fluid and hyperattenuating pelvic collection (*), with corresponding peripheral enhancement in the venous phase (B) and filling by opacified urine in the excretory phase (C). On additional delayed acquisition, leakage from the most distal tract of the left ureter (arrowheads in D, E) and progressive opacification of the urinoma (*) were seen. Endourological treatment was performed (Partially reproduced from open access ref. no [58])
The second pattern of ureteral injury is ligation without urine extravasation, which often occurs at the site of surgical clips, causes upstream hydronephrosis and may be either acute (Fig. 14) or asymptomatic (Fig. 15). Nowadays, percutaneous nephrostomy, antegrade recanalisation by endourology techniques and long-term stent placement are the preferred management for both ureteral obstruction and laceration. Alternatively, open or laparoscopic surgical repair with suturing, end-to-end uretero-ureterostomies or uretero-neocystostomy may be necessary [49, 50, 54].
Ligation of the left ureter manifesting 24 h after AH. Unenhanced CT (A) showed a sizeable vaginal vault haematoma (*) and residual pneumoperitoneum (+) as expected findings. After intravenous contrast, the left kidney showed hydronephrosis (+) and impaired nephrogram compared to contralateral side, caused by abrupt stricture of the distal ureter (+ in C) in the site of surgical clips (thin arrow in C). Surgical reoperation including clip removal was required to manage the obstruction
Bladder injury and fistulas
The urinary bladder may be damaged during surgical dissection or from laparoscopic trocar insertion. Most bladder injuries are recognised intraoperatively using dyes and cystoscopy, and immediately repaired [44, 55].
After surgery, the CT hallmark of bladder injury is represented by either extraperitoneal or intraperitoneal urine extravasation at excretory-phase CT. Since a Foley catheter is generally in place shortly after hysterectomy, minor bladder injuries and suspected urinomas should be investigated using CT cystography which confirms bladder wall integrity, ruling out possible leakages, when retrograde filling with at least 250 ml of diluted contrast is obtained (Fig. 16) [7, 9, 18]. Whereas extraperitoneal leakage is treated conservatively with bladder drainage, intraperitoneal injuries require surgical exploration and repair [8].
Multidetector CT-cystography performed 4 h after radical surgery for ovarian cystoadenocarcinoma, with intraoperative suspicion of bladder rupture. Multiplanar images show optimal distension of the normal-shaped urinary bladder by diluted contrast medium instilled via the Foley catheter. Note perivesical gas bubbles. The lack of extravasated contrast in the perivesical spaces allowed confident exclusion of either intra- or extraperitoneal bladder injury and vesico-vaginal fistula (Reproduced from open access ref. no. [18])
Alternatively, hysterectomy may result in formation of a vesico-vaginal fistula (VVF), which accounts for over two thirds of iatrogenic pelvic fistulas. The risk is highest (0.74%) during radical AH secondary to extensive parametrial and nodal dissection. The typical manifestations include continuous urinary leakage, foul odours or discharge from the vagina. Clinical diagnosis of VVF is often challenging, and requires a combination of vaginal examination, cystoscopy, bladder filling with dye and biochemical assay of discharge fluid for high creatinine levels [42, 44, 47, 56].
At imaging, a VVF is suggested by identification of air and/or fluid in the vaginal lumen. Excretory-phase CT or CT cystography are useful for treatment planning as they can confirm and directly visualise the opacified abnormal track (Fig. 17) [7, 9, 18, 57]. Albeit some VVF seal during with prolonged catheterisation, most cases ultimately require surgical repair [42, 44, 47, 56].
Vesico-vaginal fistula (VVF) developing after radical AH and radiotherapy for endometrial carcinoma in a 66-year-old female, manifesting with vaginal discharge without abnormal findings at gynaecological examination. Excretory-phase CT (A, B) showed a well- opacified urinary bladder with a Foley catheter and left-sided ureteral stent (thin arrow) in place, lateral retraction and opacification of the vagina (arrows) through a short communication (arrowheads) consistent with VVF. After vaginal electrocoagulation, long-term antibiotics and ureteral stenting, repeated CT urography 6 months later (C) showed persistent vaginal opacification (arrow) through the high-output supratrigonal VVF. A year later, CT follow-up (D) showed non-opacified vagina (arrow) indicating fistula closure (Partially reproduced with permission from ref. no. [62])
Conclusion
Imaging plays an increasingly pivotal role in the diagnosis of postoperative complications following hysterectomy, such as infections, haemorrhage, bowel perforation or obstruction, urologic injuries and fistulas. In our experience, multidetector CT allows a comprehensive assessment of the operated pelvis, and is therefore recommended to elucidate suspected post-hysterectomy complications and to provide a consistent basis for choosing between conservative, percutaneous or open surgical management.
References
Domingo S, Pellicer A (2009) Overview of current trends in hysterectomy. Expert Rev of Obstet Gynecol 4:673–685
Clarke-Pearson DL, Geller EJ (2013) Complications of hysterectomy. Obstet Gynecol 121:654–673
Erekson EA, Yip SA, Ciarleglio M et al (2011) Postoperative complications after gynecological surgery. Obstet Gynecol 118:784–793
Franchi M, Ghezzi F, Riva C et al (2001) Postoperative complications after pelvic lymphadenectomy for the surgical staging of endometrial cancer. J Surg Oncol 78:232–237 discussion 237-240
Hodges KR, Davis BR, Swaim LS (2014) Prevention and management of hysterectomy complications. Clin Obstet Gynecol 57:43–57
Sartelli M, Viale P, Catena F et al (2013) 2013 WSES guidelines for management of intra-abdominal infections. World J Emerg Surg 8:3
Paspulati RM, Dalal TA (2010) Imaging of complications following gynecologic surgery. Radiographics 30:625–642
Summerton DJ, Kitrey ND, Lumen N et al (2012) EAU guidelines on iatrogenic trauma. Eur Urol 62:628–639
Tsai R, Raptis D, Raptis C et al (2017) Complications after gynecologic and obstetric procedures: a pictorial review. Curr Probl Diagn Radiol. https://doi.org/10.1067/j.cpradiol.2017.06.006
Chan YGS, Ho HK, Chen CYH (1993) Abdominal hysterectomy: indications and complications. Singap Med J 34:337–340
Moen M (2016) Hysterectomy for benign conditions of the uterus: Total abdominal hysterectomy. Obstet Gynecol Clin N Am 43:431–440
Aarts JW, Nieboer TE, Johnson N et al (2015) Surgical approach to hysterectomy for benign gynaecological disease. Cochrane Database Syst Rev: Cd003677
Byrnes JN, Occhino JA (2016) Hysterectomy for benign conditions of the uterus: Total vaginal hysterectomy. Obstet Gynecol Clin N Am 43:441–462
American College of Gynecologists (2017) Choosing the route of hysterectomy for benign disease. URL: https://www.acog.org/Clinical-Guidance-and-Publications/Committee-Opinions/Committee-on-Gynecologic-Practice/Choosing-the-Route-of-Hysterectomy-for-Benign-Disease. Accesed 2 Oct 2017
Reich H (2007) Total laparoscopic hysterectomy: indications, techniques and outcomes. Curr Opin Obstet Gynecol 19:337–344
Jeppson PC, Sung VW (2014) Hysterectomy for pelvic organ prolapse: indications and techniques. Clin Obstet Gynecol 57:72–82
European Society of Urogenital Radiology (2016) ESUR guidelines on contrast media 9.0. Available at: “www.esur.org/guidelines”. Accesed 2 Oct 2017
Tonolini M, Bianco R (2012) Multidetector CT cystography for imaging colovesical fistulas and iatrogenic bladder leaks. Insights Imaging 3:181–187
Bennett GL, Slywotzky CM, Giovanniello G (2002) Gynecologic causes of acute pelvic pain: spectrum of CT findings. Radiographics 22:785–801
Cano Alonso R, Borruel Nacenta S, Diez Martinez P et al (2009) Role of multidetector CT in the management of acute female pelvic disease. Emerg Radiol 16:453–472
Swart JE, Fishman EK (2008) Gynecologic pathology on multidetector CT: a pictorial review. Emerg Radiol 15:383–389
Saddala P, Ramanathan S, Tirumani SH et al (2015) Complications of minimally invasive procedures of the abdomen and pelvis: a comprehensive update on the clinical and imaging features. Emerg Radiol 22:283–294
Hindman NM, Kang S, Parikh MS (2014) Common postoperative findings unique to laparoscopic surgery. Radiographics 34:119–138
Han NY, Sung DJ, Park JB et al (2014) Imaging of complications associated with port access of abdominal laparoscopic surgery. Abdom Imaging 39:398–410
Thomson AJ, Farquharson RG (2000) Vault haematoma and febrile morbidity after vaginal hysterectomy. Hosp Med 61:535–538
Thomson AJ, Sproston AR, Farquharson RG (1998) Ultrasound detection of vault haematoma following vaginal hysterectomy. Br J Obstet Gynaecol 105:211–215
Kuhn RJ, de Crespigny LC (1985) Vault haematoma after vaginal hysterectomy: an invariable sequel? Aust N Z J Obstet Gynaecol 25:59–62
Tam KF, Lam KW, Chan KK et al (2008) Natural history of pelvic lymphocysts as observed by ultrasonography after bilateral pelvic lymphadenectomy. Ultrasound Obstet Gynecol 32:87–90
Kim JK, Jeong YY, Kim YH et al (1999) Postoperative pelvic lymphocele: treatment with simple percutaneous catheter drainage. Radiology 212:390–394
Alago W Jr, Deodhar A, Michell H et al (2013) Management of postoperative lymphoceles after lymphadenectomy: percutaneous catheter drainage with and without povidone-iodine sclerotherapy. Cardiovasc Intervent Radiol 36:466–471
Kew F, Noble A, Sandhu M (2012) Infection of a lymphocyst after pelvic lymph node dissection for endocervical adenocarcinoma. J Obstet Gynaecol 32:606
Lachiewicz MP, Moulton LJ, Jaiyeoba O (2015) Pelvic surgical site infections in gynecologic surgery. Infect Dis Obstet Gynecol 2015:614950
Cronin B, Sung VW, Matteson KA (2012) Vaginal cuff dehiscence: risk factors and management. Am J Obstet Gynecol 206:284–288
Mausner EV, Yitta S, Slywotzky CM et al (2011) Commonly encountered foreign bodies and devices in the female pelvis: MDCT appearances. AJR Am J Roentgenol 196:W461–W470
Garcia J, Aboujaoude R, Apuzzio J et al (2006) Septic pelvic thrombophlebitis: diagnosis and management. Infect Dis Obstet Gynecol 2006:15614
Chirinos JA, Garcia J, Alcaide ML et al (2006) Septic thrombophlebitis: diagnosis and management. Am J Cardiovasc Drugs 6:9–14
Huang JS, Ho AS, Ahmed A et al (2011) Borne identity: CT imaging of vascular infections. Emerg Radiol 18:335–343
Katz MD, Sugay SB, Walker DK et al (2012) Beyond hemostasis: spectrum of gynecologic and obstetric indications for transcatheter embolisation. Radiographics 32:1713–1731
AlHilli MM, El-Nashar SA, Garrett AT et al (2013) Use of computed tomography in the diagnosis of bowel complications after gynecologic surgery. Obstet Gynecol 122:1255–1262
Hove LD, Bock J, Christoffersen JK et al (2010) Analysis of 136 ureteral injuries in gynecological and obstetrical surgery from completed insurance claims. Acta Obstet Gynecol Scand 89:82–86
Adelman MR, Bardsley TR, Sharp HT (2014) Urinary tract injuries in laparoscopic hysterectomy: a systematic review. J Minim Invasive Gynecol 21:558–566
Hwang JH, Lim MC, Joung JY et al (2012) Urologic complications of laparoscopic radical hysterectomy and lymphadenectomy. Int Urogynecol J 23:1605–1611
Parpala-Sparman T, Paananen I, Santala M et al (2008) Increasing numbers of ureteric injuries after the introduction of laparoscopic surgery. Scand J Urol Nephrol 42:422–427
Siow A, Nikam YA, Ng C et al (2007) Urological complications of laparoscopic hysterectomy: a four-year review at KK Women's and Children's hospital, Singapore. Singap Med J 48:217–221
Bai SW, Huh EH, Jung Da J et al (2006) Urinary tract injuries during pelvic surgery: incidence rates and predisposing factors. Int Urogynecol J 17:360–364
Dorairajan G, Rani PR, Habeebullah S et al (2004) Urological injuries during hysterectomies: a 6-year review. J Obstet Gynaecol Res 30:430–435
Lee JS, Choe JH, Lee HS et al (2012) Urologic complications following obstetric and gynecologic surgery. Korean J Urol 53:795–799
Ozdemir E, Ozturk U, Celen S et al (2011) Urinary complications of gynecologic surgery: iatrogenic urinary tract system injuries in obstetrics and gynecology operations. Clin Exp Obstet Gynecol 38:217–220
Al-Awadi K, Kehinde EO, Al-Hunayan A et al (2005) Iatrogenic ureteric injuries: incidence, aetiological factors and the effect of early management on subsequent outcome. Int Urol Nephrol 37:235–241
Mahendran HA, Praveen S, Ho C et al (2012) Iatrogenic ureter injuries: eleven years experience in a tertiary hospital. Med J Malaysia 67:169–172
Gayer G, Zissin R, Apter S et al (2002) Urinomas caused by ureteral injuries: CT appearance. Abdom Imaging 27:88–92
Titton RL, Gervais DA, Hahn PF et al (2003) Urine leaks and urinomas: diagnosis and imaging-guided intervention. Radiographics 23:1133–1147
Gayer G, Apter S, Garniek A et al (2000) Complications after laparoscopic gynecologic procedures: CT findings. Abdom Imaging 25:435–439
Koukouras D, Petsas T, Liatsikos E et al (2010) Percutaneous minimally invasive management of iatrogenic ureteral injuries. J Endourol 24:1921–1927
Ibeanu OA, Chesson RR, Echols KT et al (2009) Urinary tract injury during hysterectomy based on universal cystoscopy. Obstet Gynecol 113:6–10
Romics I, Kelemen Z, Fazakas Z (2002) The diagnosis and management of vesicovaginal fistulae. BJU Int 89:764–766
Moon SG, Kim SH, Lee HJL et al (2001) Pelvic fistulas complicating pelvic surgery or diseases: spectrum of imaging findings. Korean J Radiol 2(2):97–104
Tonolini F (2018) Early CT after vaginal hysterectomy: normal or abnormal? {Online}. EuroRAD Case 15268
Tonolini M, Pagani A (2014) Late superinfection of postsurgical lymphocele {Online} EuroRAD Case 11670
Tonolini M (2017) Life-threatening haemorrhage after laparoscopic hysterectomy {Online}. EuroRAD Case 15152
Tonolini M (2015) Iatrogenic ureteral injury with urinoma following laparoscopic hysterectomy: CT diagnosis and follow-up {Online}. EuroRAD Case 12226
Tonolini M, Damiani G (2014) Post-surgical vesico-vaginal fistula: CT diagnosis and follow-up {Online}. EuroRAD Case 12239
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Tonolini, M. Multidetector CT of expected findings and complications after hysterectomy. Insights Imaging 9, 369–383 (2018). https://doi.org/10.1007/s13244-018-0610-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13244-018-0610-9