Abstract
Objectives
To determine the diagnostic yield of computed tomography scanning of the pulmonary arteries (CTPA) in our centre and factors associated with it. Differences between specialties as well as adherence to protocol were investigated.
Methods
All patients receiving a first CTPA for pulmonary embolism (PE) in 2010 were included. Data about relevant clinical information and the requesting specialty were retrospectively obtained. Differences in diagnostic yield were tested using a chi-squared test. Independent predictors were identified with multivariate logistic regression.
Results
PE on CTPA was found in 224 of the 974 patients (23 %). Between specialties, diagnostic yield varied from 19.5 to 23.9 % (p = 0.20). Independent predictors of diagnostic yield were: age, sex, D-dimer, cough, dyspnea, cardiac history, chronic obstructive pulmonary disease (COPD), atelectasis/consolidation, intrapulmonary mass and/or interstitial pulmonary disease on CT. Wells scores were poorly documented (n = 127, 13.0 %). Poor adherence to protocol was also shown by a high amount of unnecessary D-dimer values with a high Wells-score (35 of 58; 58.6 %).
Conclusions
The diagnostic yield of CTPA in this study was relatively high in comparison with other studies (6.7–31 %). Better adherence to protocol might improve the diagnostic yield further. A prospective study could confirm the independent predictors found in this study.
Teaching Points
• Pulmonary embolism is potentially life-threatening and requires quick and reliable diagnosis.
• Computed tomography of the pulmonary arteries (CTPA) provides this reliable diagnosis.
• Several independent predictors of diagnostic yield of CTPA for pulmonary embolism were identified.
• Diagnostic yield of CTPA did not differ between requesting specialties in our Hospital.
• Better protocol adherence could improve the diagnostic yield of CTPA for pulmonary embolism.
Similar content being viewed by others
Introduction
Pulmonary embolism (PE) is a serious, potentially life-threatening disease that requires timely and effective treatment. Its diagnosis can be difficult, since symptoms are non-specific [1]. Current Dutch guidelines recommend a diagnostic work-up in three steps. Firstly, the clinical probability should be determined by calculating a Wells score [2]. Wells’ criteria are shown in Table 1. Secondly either the Wells-score is high (a score of more than four points) and a computed tomography scan of the pulmonary arteries (CTPA) should be made or, if the Wells score is low (four points or less), the D-dimer level should be assessed. Thirdly, a high D-dimer level (≥0.5 mg/ml) also dictates performing CTPA [2–4]. CTPA is currently regarded as the reference standard for confirming the diagnosis of pulmonary embolism. Its sensitivity is estimated between 60 % and 100 % and its specificity between 81 % and 98 % [5–8]. Studies show that the diagnostic yield of CTPA for pulmonary embolism varies between 6.7 % and 31 % [9–14]. In our teaching hospital (Isala, Zwolle, The Netherlands) approximately 1000 CTPA’s are made annually. Most of these CTPAs are requested by pulmonologists, internal medicine specialists or cardiologists. In this pilot study we tried to investigate the quality of the diagnostic work-up for pulmonary embolism in our hospital. We tried to determine whether there were differences in diagnostic yield between the requesting specialties, to find out the extent of protocol adherence (to perform the aforementioned diagnostic steps in the right order) and to assess independent predictors of diagnostic yield of CTPA. We expected a uniformly good standard of diagnostics, with a diagnostic yield conforming to figures from the recent literature, with room for improvement of protocol adherence.
Materials and methods
All patients receiving a CTPA for pulmonary embolism from 1 January 2010 to 31 December 2010 were included in this study. For all the exams a 40- or 64-slice MDCT with helical scan (Royal Philips) was used with a peak voltage of 120 kV and an exposure of 300 milliampere-second per slice. Electronic and paper medical files were searched for the CTPA outcome, clinical characteristics and relevant medical history. The Wells score was dichotomised to low (≤4) or high (>4), and D-dimer levels also to low (≤0.5 mg/ml) or high >0.5 mg/ml). The specialties were classified into five groups: pulmonologists, cardiologists, internal medicine specialists (including neurologists and anaesthesiologists/intensive care specialists), surgical specialists and mixed specialists (urology and gynaecology).
A chi-squared test was used to determine the differences in diagnostic yield between the specialties. A Student’s t-test for two independent groups was used to test for differences in D-dimer level between men and women. An association between D-dimer level, Wells score and the diagnostic yield was univariately tested with a chi-squared test. When appropriate, a Fisher’s exact test was used. To identify independent predictors of the diagnostic yield of CTPA, multivariate logistic regression was used. Because there was little evidence from the literature as to which factors could affect diagnostic yield of CTPA, all factors collected in this study were interpreted in this analysis. Furthermore, selecting factors based on p values seemed less likely to give a good model, since clues for the direction of a possible relationship were lacking [15]. Factors were differentiated in pre-diagnostic factors (patient characteristics) and complementary factors (findings on imaging techniques).
A p value of 0.05 or less was regarded as significant. The “Statistical Package for the Social Sciences” (SPSS), version 18.0.1 was used for statistical analysis.
Results
Between 1 January 2010 and 31 December 2010, a total of 999 patients underwent CTPA for the suspicion of pulmonary embolism in our hospital. Of this group, 22 patients were excluded because of repeated CTPA and three were excluded because CTPA was requested for other reasons. The setting for the 974 remaining patients was as follows: 691 patients presented at the emergency department (70.9 %), 214 were inpatients (22 %) and 47 were outpatients (4.8 %). For 22 patients, the setting was unknown. Figure 1 shows the flow chart for inclusion with distribution per specialty. Table 2 shows patient characteristics. There appeared to be slightly more women than men, without a significant age difference between these groups. Men had a higher mean D-dimer level than women (3.97 vs 2.89; p = 0.04), and proportionally more often had a high Wells score (56 % vs 39 %; p = 0.06).
Pulmonary embolism was found in 224 of the 974 included patients (23 %). This group consisted of 111 women and 113 men. A scan was named undiagnostic in 38 cases (4 %), meaning the reviewing radiologist could neither confirm nor rule-out a (small, subsegmental) pulmonary embolism. The differences in diagnostic yield between the specialties were analysed without the group “mixed specialties” due to the small number of patients in this group (n = 17). The diagnostic yield of the other specialties varied between 19.5 % and 23.9 %. There was no significant relationship between the diagnostic yield of CTPA and the various specialties (p = 0.20).
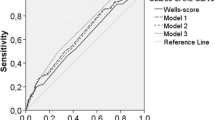
Univariate analysis showed no relationship between the Wells score and the diagnostic yield of CTPA (p = 0.84). For the D-dimer level, however, the relationship with the diagnostic yield was significant. Analysis showed that a higher D-dimer level was associated with a higher diagnostic yield of CTPA (odds ratio 13.1; 95 % confidence interval 1.8–96.5; p < 0.0001).
The Wells score was documented for 127 patients (13.0 %), the D-dimer level for 601 patients (61.7 %), and both values were present for 97 patients (10 %). The Wells score was documented most frequently by pulmonologists (n = 100; 22 %), followed by the internal medicine specialists (n = 22, 8.2 %), the cardiologists (n = 4, 8.2 %) and mixed specialties (n = 1, 5.9 %). Surgeons did not document the Wells score on any occasion. D-dimer levels were documented most frequently by cardiologists (n = 125; 79.6 %) and pulmonologists (n = 352; 77 %), followed by mixed specialties (n = 8; 47 %), internal medicine specialist (n = 69; 35 %) and surgeons (n = 20; 26 %). In 35 out of 58 patients (58.6 %) with a high Wells score, D-dimer level was also documented. Of which 26 were requested by the pulmonologist. In case of a low Wells score, D-dimer level was missing in 5 out of 69 cases (5.2 %). An association between diagnostic yield of CTPA and various combinations of high and low Wells score and D-dimer levels could not be interpreted due to low numbers.
The low numbers of documented Wells scores made the multivariate analysis of independent predictors of diagnostic yield of CTPA that included this parameter difficult to interpret. Therefore, we chose to control the complete analyses which assessed the predictive properties of the pre-diagnostic and complementary factors for: age, sex, speciality and setting.
In Table 3, the results of the analysis of pre-diagnostic factors are shown. Chest pain, dyspnea, cough, haemoptysis, malignancy, cardiac history, Chronic obstructive pulmonary disease (COPD) and surgery in the previous 4 weeks were included in the analysis (n = 866) as pre-diagnostic factors. Sex was found to be an independent predictor; female sex was associated with a lower yield. A lower yield was also found for a presentation with cough, cardiac history and/or history of COPD. Higher age and a presentation with dyspnoea increased the odds of finding pulmonary embolism. There was a borderline-significant trend for chest-pain increasing diagnostic yield (p = 0.052).
Table 4 shows the significant findings of the analysis of complementary factors. This analysis, with data of 851 patients, included the controlling factors described above and the complementary factors: alternative diagnosis on chest X-ray, findings of an infiltrate, atelectasis/consolidate, ground-glass aspect, interstitial abnormalities and an intrapulmonary mass on CT. In this analysis, sex and age were found to be similarly associated with diagnostic yield, as found in the pre-diagnostic analysis. Complementary factors that made a pulmonary embolism on CTPA less likely to find were: atelectasis/consolidate and interstitial abnormalities.
Discussion
This study aimed to determine the diagnostic yield of CTPA and investigated differences in this yield between specialties. Furthermore, protocol adherence was examined. To our knowledge, it is the first study that also aimed to identify factors that could influence the diagnostic yield of CTPA. We think that it is very likely that the working method regarding the diagnostics of pulmonary embolism in our centre resembles the situation in many other hospitals closely. So, in our opinion, results might be generalised. The diagnostic yield of 23 % that we found is relatively high in comparison with values reported in the literature (6.7–31 %) [9–14]. Another study in The Netherlands found a diagnostic yield of 19.1 % [16]. The relatively high diagnostic yield could be the result of technological advances in scanning technique, leading to the discovery of more small, subsegmental pulmonary emboli, the clinical relevance of which is still controversial [17]. An example of this development is the introduction of dual-energy multidetector CT, which, in preliminary studies, shows promising results [18]. The differences in diagnostic yield between the specialties (19.5–23.9 %) in this study were not significant, which could be an indication of a uniformly high quality of diagnostic work-up for pulmonary embolism in our hospital, although this is not properly documented, as is shown in the following paragraph. According to protocol, for every patient with a suspicion of pulmonary embolism, a Wells score should be calculated. This study found however, that for only was 13.0 % the Wells score documented. Proportionally most Wells scores were documented by pulmonologists (22 %), followed by internal medicine specialists (8.2 %). It is likely that in daily practice this score is being calculated more often than it is documented. The D-dimer level, on the other hand, is being documented in many more cases, namely in 61.7 % of the patients in this study.
As earlier stated, only when the Wells score is low should the D-dimer level be assessed. High D-dimer levels dictate making a CTPA. However, in daily practice, the D-dimer level is often being requested together with standard laboratory investigations immediately when a patient presents with a suspicion of pulmonary embolism. This intends to save time, but may result in too many D-dimer level requests, and thus in unnecessary costs and unnecessary requests for CT scans. In case of a high Wells score, the D-dimer level is being requested in 58.6 % of patients, which is not according to protocol recommendations; and D-dimer level was missing for 5 out of 69 patients with a low Wells score. These results suggest that D-dimer level and Wells-score were requested and interpreted independently, which is in contradiction of the protocol, which recommends to consistently follow the three steps in pulmonary embolism diagnostics.
From the literature, little is known about factors associated with diagnostic yield of CTPA. To gain more knowledge about this, we conducted a multivariate analysis to identify potential pre-diagnostic and complementary factors. Unfortunately, the most important multivariate analysis in this study could not be controlled for Wells score and D-dimer level, since there were too many missing values for both of these factors together. The performed analysis showed that higher age, male sex, dyspnea, atelectasis/consolidate on CT and/or intrapulmonary mass on CT were independently associated with higher diagnostic yield of CTPA. There was a borderline significant trend for chest pain. It was less likely to find a pulmonary embolism on CT in presence of the following factors: female sex, cough, cardiac history, COPD and/or interstitial abnormalities. Univariate analysis raised the suspicion that a higher D-dimer level was also associated with a higher diagnostic yield.
The presence of an alternative diagnosis for the symptoms of the patients with cardiac history, COPD, atelectasis/consolidate on CT and/or interstitial abnormalities on CT could be the explanation for the lower yield of CTPA in these patients. The influence of age could be attributed to the fact that with increasing age the incidence of pulmonary embolism is also increased [19]. The association with higher diagnostic yield in patients with chest pain and dyspnea is an indication that these findings correctly raise a suspicion of pulmonary embolism [20, 21]. Female sex seemed to protect against finding pulmonary embolism. To explain this, two possible reasons can be given. Firstly, in our study significantly lower D-dimer levels and almost significantly lower Wells scores were found in females. Secondly, in our study, more females than men were undergoing CTPA, while the literature showed that there are reasons to believe that the incidence of pulmonary embolism is equal among the sexes [2, 22–24]. It may be the case that doctors are sooner inclined to perform CTPA in (young) female patients because of risk-factors not being scored in the Wells table, e.g. contraceptives or pregnancy, even though this is speculative.
In every retrospective study the reliability of data can be a problem, because data from letters or notes made at the time of presentation can be misinterpreted. Probably, some of the CTPAs were requested for reasons other than suspicion of pulmonary embolism and some CTPAs could have been falsely classified as positive. The largest problem was, however, posed by the fact that the Wells score was known for such a limited number of patients, which made some of the analysis, as described in the results section, difficult to interpret. This caused a problem in determining the true independent influence of Wells score and D-dimer on diagnostic yield of CTPA.
This study shows a relatively high diagnostic yield of CTPA in our hospital, without differences in requesting specialties, which could indicate uniform good quality of pulmonary embolism diagnostics in our centre, although this is not properly documented. Adherence to protocol proves to be subject for improvement, especially since the Wells score and D-dimer levels appeared to be requested and interpreted independently. Better adherence to the protocol could improve diagnostic yield and lower costs. Furthermore, reduction of unnecessarily requested CTPA leads to a reduction in radiation exposure. In order to make sure the three steps in diagnostics are followed, it might be considered to develop a requesting system in which respectively a D-dimer and a CTPA can only be requested after a Wells score is determined and documented.
A prospective study will be conducted to confirm the independent predicting factors of the diagnostic yield of CTPA found in this study. This could aid the development of new clinical assessment tools. Moreover, in this manner the influence of the Wells score and D-dimer can also be better determined.
References
Gandara E, Wells PS (2010) Diagnosis: use of clinical probability algorithms. Clin Chest Med 31:629–639
Wells PS, Anderson DR, Rodger M et al (2001) Excluding pulmonary embolism at the bedside without diagnostic imaging: management of patients with suspected pulmonary embolism presenting to the emergency department by using a simple clinical model and d-dimer. Ann Intern Med 135:98–107
Wells PS, Anderson DR, Rodger M et al (2000) Derivation of a simple clinical model to categorize patients probability of pulmonary embolism: increasing the models utility with the SimpliRED D-dimer. Thromb Haemost 83:416–420
Kwaliteitsinstituut voor de Gezondheidszorg CBO algemeen voorzitterschap van Buller, H.R (2008) CBO richtlijn diagnostiek, preventie en behandeling van veneuze trombo-embolie en secundaire preventie van arteriele trombose; found on http://www.nvkc.nl/kwaliteitsborging/documents/Richtlijnveneuzetrombodefinitief--130109.pdf. Accessed 13 January 2014
Eng J, Krishnan JA, Segal JB et al (2004) Accuracy of CT in the diagnosis of pulmonary embolism: a systematic literature review. AJR Am J Roentgenol 183:1819–1827
Stein PD, Fowler SE, Goodman LR et al (2006) Multidetector computed tomography for acute pulmonary embolism. N Engl J Med 354:2317–2327
Stein PD, Kayali F, Hull RD (2007) Spiral computed tomography for the diagnosis of acute pulmonary embolism. Thromb Haemost 98:713–720
Remy-Jardin M, Pistolesi M, Goodman LR et al (2007) Management of suspected acute pulmonary embolism in the era of CT angiography: a statement from the Fleischner Society. Radiology 245:315–329
Hoo GW, Wu CC, Vazirani S, Li Z, Barack BM (2011) Does a clinical decision rule using D-dimer level improve the yield of pulmonary CT angiography? AJR Am J Roentgenol 196:1059–1064
Chin P, Hurrell M, McGregor D, Beckert L (2006) The role of CT pulmonary angiography in patients with suspected pulmonary embolism admitted to general medicine. N Z Med J 119:U2052
David S, Beddy P, Babar J, Devaraj A (2011) Evolution of CT pulmonary angiography: referral patterns and diagnostic yield in 2009 compared with 2006. Acta Radiol 53:39–43
Costantino MM, Randall G, Gosselin M, Brandt M, Spinning K, Vegas CD (2008) CT angiography in the evaluation of acute pulmonary embolus. AJR Am J Roentgenol 191:471–474
Donohoo JH, Mayo-Smith WW, Pezzullo JA, Egglin TK (2008) Utilization patterns and diagnostic yield of 3421 consecutive multidetector row computed tomography pulmonary angiograms in a busy emergency department. J Comput Assist Tomogr 32:421–425
Kiley CA, Lowry KJ, Mysliwiec V (2007) Examination of hospital referral practices for CT pulmonary angiography. J Hosp Med 2:253–257
Steyerberg EW, Eijkemans MJ, Harrell FE Jr, Habbema JD (2001) Prognostic modeling with logistic regression analysis: in search of a sensible strategy in small data sets. Med Dec Making 21:45–56
De Bruin S, Van Langevelde K, Huisman MV, Cannegieter SC (2012) Verdenking longembolie: CT-rendement hangt af van patiëntenkenmerken en verwijzer. Ned Tijdschr Geneeskd 156:A4201
Wiener RS, Schwartz LM, Woloshin S (2013) When a test is too good: how CT pulmonary angiograms find pulmonary emboli that do not need to be found. BMJ 347:f3368
Tang CX, Zhang LJ, Han ZH et al (2013) Dual-energy CT based vascular iodine analysis improves sensitivity for peripheral pulmonary artery thrombus detection: an experimental study in canines. Eur J Radiol 82(12):2270–2278
Goldhaber SZ (2004) Pulmonary embolism. Lancet 363:1295–1305
Stein PD, Terrin ML, Hales CA et al (1991) Clinical, laboratory, roentgenographic, and electrocardiographic findings in patients with acute pulmonary embolism and no pre-existing cardiac or pulmonary disease. Chest 100:598–603
Squizzato A, Luciani D, Rubboli A et al (2011) Differential diagnosis of pulmonary embolism in outpatients with non-specific cardiopulmonary symptoms. Intern Emerg Med 8:695-702
Musset D, Parent F, Meyer G et al (2002) Diagnostic strategy for patients with suspected pulmonary embolism: a prospective multicentre outcome study. Lancet 360:1914–1920
Moores L, Bilello KL, Murin S (2004) Sex and gender issues and venous thromboembolism. Clin Chest Med 25:281–297
Roggenland D, Peters SA, Lemburg SP, Holland-Letz T, Nicolas V, Heyer CM (2008) CT angiography in suspected pulmonary embolism: Impact of patient characteristics and different venous lines on vessel enhancement and image quality. AJR Am J Roentgenol 190:W351–W359
Acknowledgements
The authors declare that they have no actual or potential conflict of interest in relation to this article. No sponsorship or grants were received.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Walen, S., Leijstra, MA., Uil, S.M. et al. Diagnostic yield of CT thorax angiography in patients suspected of pulmonary embolism: independent predictors and protocol adherence. Insights Imaging 5, 231–236 (2014). https://doi.org/10.1007/s13244-014-0325-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13244-014-0325-5