Abstract
Purpose
To analyze obstetric admissions to intensive care unit and to identify the risk factors responsible for intensive care admission.
Methods
This is a retrospective study of all obstetric cases admitted to the intensive care unit over a period of 3 years. Data were collected from case records. The risk factors responsible for ICU admission were analyzed.
Results
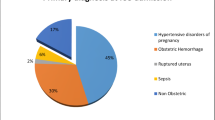
There were 765 obstetric admissions to ICU accounting for 1.24 % of all deliveries. 56.20 % were in the age group of 20–25 years. 38.43 % were in their first pregnancy. 36.48 % of cases were at 37–40 weeks of gestation. Postpartum admissions were 80.91 %. Major conditions responsible were obstetric hemorrhage in 44.05 %, hypertensive disorders of pregnancy in 28.88 %, severe anemia in 14.37 %, heart disease in 12.15 %, and sepsis in 7.97 % of ICU cases. 40.39 % cases required high dependency care. Maternal mortality was seen in 15.55 % of ICU cases. Commonest cause of mortality was hemorrhagic shock (26.89 %) and multiorgan dysfunction syndrome (26.05 %).
Conclusion
Commonest risk factors for ICU admissions are obstetric hemorrhage and hypertensive disorders of pregnancy. Other major risk factors are severe anemia, heart disease, sepsis, more than one diagnosis on admission, and the need for cesarean delivery.
Similar content being viewed by others
Introduction
Obstetric emergencies are a challenge to the obstetrician because of the unique nature of obstetric medicine. The altered physiology of pregnancy, the presence of the fetus, the rapid deterioration of maternal and fetal condition in case of a complication, and the simultaneous management of two lives with different physiologies are a challenge [1]. These emergency conditions should be managed in a well-equipped, dedicated obstetric intensive care unit (ICU) for better maternal and fetal outcomes [2]. The percentage of obstetric population requiring admission to the ICU is different in different countries based on the socioeconomic status, criteria for ICU admission, availability of ICU beds, and availability of a high dependency unit. It ranges from 0.08 to 0.76 % of deliveries in developed countries [3–7] and 0.13 to 4.6 % in developing countries [1, 8–15]. The mortality in these patients is high and ranges from 0 to 4.9 % of ICU admissions in developed [4–7] and 2–43.63 % in developing countries [8–11, 13, 15, 16]. Hypertensive disorders and obstetric hemorrhage are the two the commonest risk factors for ICU admission [7]. The other risk factors are sepsis, cardiac disease, and severe anemia [7, 13, 14, 17, 18]. The present study was done to analyze all the obstetric admissions to the intensive care unit of a tertiary care referral hospital for a period of 3 years and to identify the risk factors responsible for admission.
Materials and Methods
It is a retrospective study of obstetric cases admitted to the intensive care unit over a period of 3 years from July 2010 to June 2013. All the pregnant and postpartum (<42 days) patients admitted to the intensive care unit of Vanivilas hospital attached to Bangalore Medical College and Research Institute, Bangalore were included the study. The admissions were identified from the ICU register, and the case records of the patients were studied in detail. The parameters noted were the age, parity, diagnosis on admission, associated medical and surgical condition, the ward from which the patient was shifted to ICU, reason for ICU admission, any surgical procedure performed, antenatal or postnatal admission, details of treatment given like ventilator support, blood and blood component transfusion, ionotropic support, and dialysis. The neonatal outcome was noted in terms of death and neonatal intensive care admissions. The total duration of stay was noted. The maternal mortality and its cause were noted. Vanivilas hospital is a medical college-attached hospital. Cases from all over the state and also some places of nearby states are referred to this institute. The ICU of the hospital is a six-bedded obstetric ICU managed by the anesthetist and obstetrician. 24-h laboratory and blood-bank facilities are available. The ICU does not have dialysis facility for which we have to shift the patient to adjacent nephrourology block. Cardiologists, nephrologists, neurologists, hematologists, pulmonologists, and gastroenterologists are available as and when required for consultation. In this hospital, all the services for pregnant women and women in puerperium including ICU admission and investigations are free of cost.
Results
During the study period, there were 63,800 obstetric admissions and 61,615 deliveries. 765 obstetric patients were admitted to the intensive care unit. This is the largest number reported so far from a single center. ICU cases accounted for 1.19 % of all obstetric admissions and 1.24 % of all deliveries. 90 % of the cases in ICU were referred from outside hospitals. 56.20 % of the cases were in the age group of 20–25 years, followed by 22.61 % of the patients in age group 26–30 years (Table 1). 38.43 % of women were in their first pregnancy followed by 35 % of women who were in their second pregnancy (Table 2). Gestational age on admission to the hospital was calculated predominantly based on the date of last menstrual period. Majority of the women were of 37–40 weeks of gestation accounting for 36.48 % of cases. 13.59 % of women were in gestational age group of 29–34 weeks, and 12.49 % were of 35–36 weeks. 16.99 % of women were admitted to our hospital in puerperium (Table 3). Majority of patients admitted in ICU were postpartum admissions accounting for 80.91 % of cases. 8.8 % of the patients were antenatal admissions with more than 20 weeks of gestation. The rest of the cases were with ectopic pregnancy, abortion,, and molar pregnancy contributing to 5.35, 4.70, and 0.13 % of admissions, respectively (Table 4). 50.72 % of admissions were from the emergency operation theater followed by 43 % of admissions from labor ward (Table 5). The different conditions diagnosed on admission to the hospital ranged from common conditions like preeclampsia to rare disorders like myasthenia gravis. There were 52 cases (6.79 %) which did not have any obstetric or medical risk factors on admission but still developed unexpected complications. Among the 52 cases, 42 were taken for emergency section, and 10 were vaginal deliveries. 122 (15.94 %) cases had more than one diagnosis on admission. Among them, 79 (10.32 %) had two diagnosis, 30 (3.92 %) had three diagnosis, and 13 (1.69 %) had more than three diagnosis on admission. As shown in Table 6, obstetric hemorrhage (44.05 %) was the commonest condition requiring ICU admission followed by hypertensive disorder of pregnancy (28.88 %). The other major conditions were anemia (14.37 %), heart disease (12.15 %), and sepsis (7.97 %). 46.27 % of patients stayed for 2 days, 30.98 % of patients stayed for a duration of 2–4 days, and the maximum duration of stay in ICU was 25 days (Table 7). 40.39 % of women did not require ICU admission and could be managed in an HDU. Our hospital does not have an HDU so the cases were admitted in ICU. The commonest therapy given (Table 8) was the blood (51.37 %) and blood component (26.93 %) transfusion, followed by ionotropic support (45.75 %), and followed by ventilator support (40.50 %). 60.78 % of women underwent surgical procedures (Table 9). The commonest surgical procedure performed was the cesarean section (37.12 %) followed by peripartum hysterectomy (9.67 %). The number of maternal deaths was 119 which accounts for 15.55 % of obstetric patients admitted in ICU and 18.42 % of deliveries among ICU patients. The commonest causes of maternal mortality (Table 10) were hemorrhagic shock (26.89 %) and multiorgan dysfunction syndrome (26.05 %). There were 646 deliveries among ICU patients. 74.61 % were live births, and 20.43 % were neonatal intensive care admissions.
Discussion
Obstetric medicine is unique and complicated. Obstetric medicine is different from the general medicine because of the various physiological changes occurring in pregnancy, and only an experienced obstetrician who has good knowledge of obstetric medicine can interpret and understand complex conditions in pregnancy. The threshold of an insult required for ICU admission is low in obstetric patients compared to nonpregnant population. We have seen women developing disseminated intravascular coagulation very rapidly with obstetric complications like hemorrhage and hypertensive disorders. The threshold for ventilator support also is low in pregnancy. These are just observations and experiences, and further study is needed to validate the same.
The rate of ICU admissions in this study was 1.19 % of all obstetric admissions and 1.24 % of all deliveries. Studies done in the past 10 years report an incidence which varies between developed and developing countries. It ranges from 0.08 to 4.6 % of deliveries. The rate in this study is higher than other studies [1, 3–7, 9, 15, 18] because 90 % of the ICU cases included in this study were booked elsewhere and referred to our institute for tertiary care. However, the rate is lower compared to some studies [8, 10, 19].
Gestational age The commonest gestational age was term gestation indicating that complications are common at term and around the time of delivery followed by women in gestational age group of 29–34 weeks and 35–36 weeks, explaining the high-risk cases requiring early termination. The mean gestational age reported in other studies ranges from 31 to 36 weeks [9–11, 15]. 16.99 % of women were admitted to our hospital in puerperium. These were the cases which delivered in outside hospitals. This can be used as an indicator of care in peripheral hospitals especially the management of third stage of labor. Hence, there is a need for education in peripheral hospitals for the nurses and junior doctors in active management of third stage of labor and also to identify at-risk cases and for timely referral.
Postpartum admissions accounted for 80.91 %. The reasons can be the following: postpartum complications were more especially postpartum hemorrhage, patients requiring cesarean section were shifted to the ICU after cesarean, some patients with risk factors were already in active labor and were shifted to the ICU after delivery, cases were referred from outside after delivery, and some patients developed complications during cesarean section. Postoperative admissions were not out of complications related to surgical skills but because of the antenatal morbidity for which cesarean was done. For example, conditions like placental abruption, obstructed labor, HELLP syndrome, severe preeclampsia, and eclampsia that require operative delivery, as such, are more prone for postpartum hemorrhage and disseminated intravascular coagulation. The severe preeclampsia patients are more prone for pulmonary edema after cesarean section. Operative delivery in the presence of medical or obstetric complication can be a potential risk factor for ICU admission.
Antenatal admissions were 8.8 %. These patients were either severely ill or remote from term gestation. Patients who were ill and required delivery were shifted to the labor room and admitted to ICU after delivery unless they required ventilator support. There should be facilities for conducting labor in ICU because these patients can need ventilator support any time, and time will be unnecessarily wasted in shifting them later. Studies done so far report postpartum admissions as the majority. Some studies have reported a majority of antepartum admissions [13, 20], and delivery admissions (on the day of delivery) [6, 21], some studies have reported a high rate, though not the majority [10, 15]. Epidemiology of antepartum admissions needs further research.
Previous cesarean delivery There were a total of 101 delivery cases with one previous cesarean and 14 cases with two previous cesarean both accounting for 15 % of all the cases. Among them, 94 cases had associated obstetric and medical risk factors. Scar on the uterus adds to the risk for ICU admission. Cases like severe preeclampsia and heart diseases which could be delivered vaginally were taken for emergency cesarean because of the scar, an additional factor contributing to the morbidity. Minimizing primary cesarean sections will reduce the ICU admissions and the morbidity. Zwart JJ has reported previous cesarean in 14.7 % cases, which is the same figure as found in our study. One study reports a high percentage of 35.36 % [10].
Low-risk patients 52 cases (6.79 %) belonged to the low-risk group. They had no medical or obstetric disorders. Among them, 42 were taken for emergency cesarean, and ten were normal deliveries. Should the need for an emergency cesarean delivery in a low-risk pregnancy be considered a risk factor for ICU admission is a question here, which needs further study. If we exclude them, then it can be said that 1.30 % (10 cases) of cases without risk factors can develop complications requiring ICU admission.
The number of comorbid conditions 15.94 % cases had more than one diagnosis on admission. Any obstetric or medical risk factor is a potential predictor of ICU admission. The risk increases with the number of conditions diagnosed on admission.
Major risk factors Obstetric hemorrhage (44.05 %) was the commonest condition requiring ICU admission followed by hypertensive disorder of pregnancy (28.88 %). The other major conditions were severe anemia (14.37 %), heart disease (12.15 %), and sepsis (7.97 %). Some studies report hypertensive disorders as the commonest condition [2, 4, 9, 10, 16]. Some studies report obstetric hemorrhage as the commonest condition [5, 7, 14, 22]. For hypertensive disorders, the range is 7–73.6 % from 24 studies [1–24], and the mean is 34.85 %. For obstetric hemorrhage, the range is 11–62.5 %, and the mean is 27.90 % from 23 studies [1–12, 14–24].
Small MJ has reported cardiac dysfunction in 36 % cases and as the commonest condition [18]. Mirghani also reports a high percentage (21.6 %) of cardiac disease compared to this study [22]. The percentage of cardiac disease ranges from 3.5 to 18.3 in other studies [5–8].
Sepsis was seen in the range of 2.4–18.3 in other studies [10, 13, 16, 24, 25]. Three studies reported sepsis rates similar to our study [6, 7, 14]. Yuel reports a high rate of 30.9 % [13].
One study done in India reports a high rate of anemia (38.18 %) and also as the commonest risk factor [13].
40.39 % of women could be managed in an HDU. There should be a HDU in all tertiary obstetric care hospitals. It will minimize the burden on ICU staff.
Cesarean delivery 60.78 % of women underwent surgical procedures. The commonest surgical procedure performed was the emergency cesarean section (37.12 %). Other studies report a high percentage of cesarean sections among ICU patients, 78.5 % [10], 50.7 % [4], 52.9 % [5], and 67.27 % [20], compared to this study. This indicates that most of the women needed operative delivery. Cesarean delivery, especially in the presence of obstetric and medical comorbidities, can be a potential risk factor for ICU admission and needs further research. According to Zwart, cesarean delivery is an adjusted risk factor for ICU admission [5].
The number of maternal deaths was 119 which accounts for 15.55 % of obstetric patients admitted in ICU and 18.42 % of deliveries among ICU patients. The commonest causes of maternal mortality were hemorrhagic shock (26.89 %) and multiorgan dysfunction syndrome (26.05 %). Mortality in this study is high compared to other studies [1, 4–7, 9, 10, 14, 16, 18, 21, 22, 24] but low compared to studies done in India [11–13, 15, 19, 23]. Multiorgan dysfunction has been reported as the commonest cause of mortality in some studies [1, 10, 24]. Irrespective of the primary disease, multiorgan failure commonly occurs in pregnancy as an end result [15]. The commonest cause is the hypertensive disorder of pregnancy. The causes for multiorgan failure in this study were HELLP syndrome, sepsis, and acute fatty liver of pregnancy.
Conclusion
In conclusion, 1.24 % of deliveries required intensive care in our hospital. There is a need for HDU in tertiary care hospitals. Obstetric hemorrhage and hypertensive disorders of pregnancy are the major risk factors for ICU admission. Majority of complications occurred in women with gestational age of 37–42 weeks. 1.30 % patients with low-risk factors required ICU admissions. There is a need to train obstetricians in obstetric medicine and critical care to do justice to these critically ill pregnant women. Commonest cause for maternal mortality was hemorrhagic shock and multiorgan dysfunction. There is a need for training in emergency obstetrics so that the complication can be managed right at the time of occurrence. Training is also required for the junior doctors working in peripheral health centers in identifying at-risk cases and for timely referral. Severe anemia, cardiac disease, sepsis, need for a cesarean delivery, and more than one diagnosis on admission are the other risk factors for ICU admission.
References
Vasquez DN, Estenssoro E, Canales HS, et al. Clinical characteristics and outcomes of obstetric patients requiring ICU admission. Chest. 2007;131(3):718–24.
Zeeman GG, Wendel GD, Cunningham FG. A blueprint for obstetric critical care. Am J Obstet Gynecol. 2003;188:532–6.
Sadler LC, Austin DM, Masson VL, et al. Review of contributory factors in maternity admissions to intensive care at a New Zealand tertiary hospital. Am J Obstet Gynecol. 2013;209:549.e1-7.
Keizer JL, Zwart JJ, Meerman RH, et al. Obstetric intensive care admissions: a 12-year review in a tertiary care centre. Eur J Obstet Gynecol Reprod Biol. 2006;128(1–2):152–6.
Zwart JJ, Dupuis JR, Richters A, et al. Obstetric intensive care unit admission: a 2-year nationwide population-based cohort study. Intensive Care Med. 2010;36(2):256–63.
Wanderer JP, Leffert LR, Mhyre JM, et al. Epidemiology of obstetric-related ICU admissions in Maryland: 1999–2008. Crit Care Med. 2013;41(8):1844–52.
Baskett TF, O’Connell CM. Maternal critical care in obstetrics. J Obstet Gynaecol Can. 2009;31(3):218–21.
Ibrahim IA, Rayis DA, Alsammani MA, et al. Obstetric and gynecologic admissions to the intensive care unit at Khartoum Hospital, Sudan. Int J Gynecol Obstet. 2015;129(1):84.
Rios FG, Risso-Vazquez A, Alvarez J, et al. Clinical characteristics and outcomes of obstetric patients admitted to the intensive care unit. Int J Gynecol Obstet. 2012;119:136–40.
Neto AFO, Parpinelli MA, Cecatti JG. Factors associated with maternal death in women admitted to an intensive care unit with severe maternal morbidity. Int J Gynaecol Obstet. 2009;105(3):252–6.
Gupta S, Naithani U, Doshi V, et al. Obstetric critical care: a prospective analysis of clinical characteristics, predictability, and fetomaternal outcome in a new dedicated obstetric intensive care unit. Indian J Anesth. 2011;55(2):146–53.
Tempe A, Wadhwa L, Gupta S, Bansal S, Satyanarayana L. Prediction of mortality and morbidity by simplified acute physiology score II in obstetric intensive care unit admissions. Indian J Med Sci. 2007;61:179–85.
Yuel VI, Kaur V, Kaur G, et al. Critical care in obstetrics-scenario in a developing country. J Obstet Gynaecol India. 2008;58(3):217–20.
Leung NY, Lau AC, Chan KK, et al. Clinical characteristics and outcomes of obstetric patients admitted to the intensive care unit: a 10-year retrospective review. Hong Kong Med J. 2010;16:18–25.
Karnad DR, Lapsia V, Krishnan A, et al. Prognostic factors in obstetric patients admitted to an Indian intensive care unit. Crit Care Med. 2004;32:1294–9.
Bandeira AR, Rezende CA, Reis ZS, et al. Epidemiologic profile, survival, and maternal prognosis factors among women at an obstetric intensive care unit. Int J Gynaecol Obstet. 2014;124(1):63–6.
Jain M, Modi JN. An audit of obstetric admissions to intensive care unit in a medical college hospital of central India: lessons in preventing maternal morbidity and mortality. Int J Reprod Contracept Obstet Gynecol. 2015;4(1):140–5.
Small MJ, James AH, Kershaw T, et al. Near-miss maternal mortality: cardiac dysfunction as the principal cause of obstetric intensive care unit admissions. Obstet Gynecol. 2012;119:250–5.
Sheela CN, Mhaskar A, Mhaskar R. Critical care in obstetrics—a 3 year review in a tertiary referral hospital. J Obstet Gynecol India. 2004;54:155–7.
Ashraf N, Mishra SK, Kundra P et al. Obstetric patients requiring intensive care: A one year retrospective study in a Tertiary Care Institute in India. Anesthesiol Res Pract. 2014, Article ID 789450:4 pages.
Stevens TA, Carroll MA, Promecene MA, et al. Utility of acute physiology, age, and chronic health evaluation (APACHE III) score in maternal admissions to the intensive care unit. Am J Obstet Gynecol. 2006;194:e13–5.
Mirghani HM, Hamed M, Ezimokhai M, et al. Pregnancy-related admissions to the intensive care unit. Int J Obstet Anesth. 2004;13:82–5.
Bhat PBR, Navada MH, Rao SV, et al. Evaluation of obstetric admissions to intensive care unit of a tertiary referral center in coastal India. Indian. J Crit Care Med. 2013;17(1):34–7.
Demirkiran O, Dikmen Y, Utku T, et al. Critically ill obstetric patients in the intensive care unit. Int J Obstet Anesth. 2003;12(4):266–70.
Togal T, Yucel N, Gedik E, et al. Obstetric admissions to the intensive care unit in a tertiary referral hospital. J Crit Care. 2010;25:628–33.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr Ashakiran T R and Dr Malini K V declare that they do not have any conflict of interest.
Ethical approval
The present study was approved by the ethical committee of our institute. Informed consent from patients was not taken because data collection was retrospective.
Additional information
Ashakiran T. Rathod is an Assistant professor in the Department of Obstetrics and Gynecology at Bangalore Medical College and Research Institute, Bangalore; Malini K. V. is a Professor and the Head of the Department of Obstetrics and Gynecology at Bangalore Medical College and Research Institute, Bangalore.
Rights and permissions
About this article
Cite this article
Rathod, A.T., Malini, K.V. Study of Obstetric Admissions to the Intensive Care Unit of a Tertiary Care Hospital. J Obstet Gynecol India 66 (Suppl 1), 12–17 (2016). https://doi.org/10.1007/s13224-015-0750-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13224-015-0750-5