Abstract
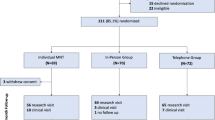
Engaging patients in a group-based weight loss program is a challenge for the acute-care hospital outpatient setting. To evaluate the feasibility, effectiveness and cost-effectiveness of a telephone-based weight loss service and an existing face-to-face, group-based service a non-randomised, two-arm feasibility trial was used. Patients who declined a two-month existing outpatient group-based program were offered a six-month research-based telephone program. Outcomes were assessed at baseline, two months (both groups) and six months (telephone program only) using paired t tests and linear regression models. Cost per healthy life year gained was calculated for both programs. The telephone program achieved significant weight loss (−4.1 ± 5.0 %; p = 0.001) for completers (n = 35; 57 % of enrolees) at six months. Compared to the group-based program (n = 33 completers; 66 %), the telephone program was associated with greater weight loss (mean difference [95%CI] −2.0 % [−3.4, −0.6]; p = 0.007) at two months. The cost per healthy life year gained was $33,000 and $85,000, for the telephone and group program, respectively. Telephone-delivered weight management services may be effective and cost-effective within an acute-care hospital setting, likely more so than usual (group-based) care.

Similar content being viewed by others
References
Ng M, Fleming T, Robinson M, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014; 384: 766-781.
National Preventative Health Taskforce. Australia: the healthiest country by 2020. In: Ministry for Health and Ageing, Canberra. 2009.
Colagiuri S, Lee CM, Colagiuri R, et al. The cost of overweight and obesity in Australia. Med J Aust. 2010; 192: 260-264.
Korda RJ, Liu B, Clements MS, et al. Prospective cohort study of body mass index and the risk of hospitalisation: findings from 246 361 participants in the 45 and Up Study. Int J Obes. 2012.
Hart CL, Hole DJ, Lawlor DA, Smith GD. Obesity and use of acute hospital services in participants of the Renfrew/Paisley study. J Publ Health. 2007; 29: 53-56.
Darnis S, Fareau N, Corallo CE, Poole S, Dooley MJ, Cheng AC. Estimation of body weight in hospitalized patients. QJM. 2012; 105: 769-774.
Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of Obesity in the United States, 2009–2010. NCHS Data Brief. 2012; 82
Ash S, Reeves M, Bauer J, et al. A randomised control trial comparing lifestyle groups, individual counselling and written information in the management of weight and health outcomes over 12 months. Int J Obes. 2006; 30: 1557-1564.
Paul-Ebhohimhen V, Avenell A. A systematic review of the effectiveness of group versus individual treatments for adult obesity. Obes Facts. 2009; 2: 17-24.
Glasgow RE, McKay HG, Piette JD, Reynolds KD. The RE-AIM framework for evaluating interventions: what can it tell us about approaches to chronic illness management? Patient Educ Couns. 2001; 44: 119-127.
Goode A, Reeves M, Eakin E. Telephone-delivered interventions for physical activity and dietary behaviour change: an updated systematic review. Am J Prev Med. 2012; 42: 81-88.
Eakin EG, Lawler SP, Vandelanotte C, Owen N. Telephone interventions for physical activity and dietary behavior change: a systematic review. Am J Prev Med. 2007; 32: 419-434.
van Wier MF, Ariens GA, Dekkers JC, Hendriksen IJ, Smid T, van Mechelen W. Phone and e-mail counselling are effective for weight management in an overweight working population: a randomized controlled trial. BMC Public Health. 2009; 9: 6.
VanWormer JJ, Martinez AM, Benson GA, et al. Telephone counseling and home telemonitoring: the Weigh by Day Trial. Am J Health Behav. 2009; 33: 445-454.
Sherwood NE, Jeffery RW, Pronk NP, et al. Mail and phone interventions for weight loss in a managed-care setting: weigh-to-be 2-year outcomes. Int J Obes. 2006; 30: 1565-1573.
Ely AC, Banitt A, Befort C, et al. Kansas primary care weighs in: a pilot randomized trial of a chronic care model program for obesity in 3 rural Kansas primary care practices. J Rural Health : Off J Am Rural Health Assoc National Rural Health Care Assoc. 2008; 24: 125-132.
Djuric Z, DiLaura NM, Jenkins I, et al. Combining weight-loss counseling with the weight watchers plan for obese breast cancer survivors. Obes Res. 2002; 10: 657-665.
Dekkers JC, van Wier MF, Ariens GA, et al. Comparative effectiveness of lifestyle interventions on cardiovascular risk factors among a Dutch overweight working population: a randomized controlled trial. BMC Public Health. 2011; 11: 49.
Whittemore R. A systematic review of the translational research on the Diabetes Prevention Program. Transl Behav Med. 2011; 1: 480-491.
O’Hara BJ, Phongsavan P, Venugopal K, et al. Effectiveness of Australia’s Get Healthy Information and Coaching Service(R): translational research with population wide impact. Prev Med. 2012; 55: 292-298.
Goode A, Reeves M, Owen N, Eakin E. Results from the dissemination of an evidence-based telephone-delivered intervention for healthy lifestyle and weight loss: the Optimal Health Program. Transl Behav Med. 2013; 3: 340-350.
Sangster J, Furber S, Allman-Farinelli M, et al. Effectiveness of a pedometer-based telephone coaching program on weight and physical activity for people referred to a cardiac rehabilitation program: a randomized controlled trial. J Cardiopulmonary Rehab and Prev. 2014.
Vale MJ, Jelinek MV, Best JD, et al. Coaching patients On Achieving Cardiovascular Health (COACH): a multicenter randomized trial in patients with coronary heart disease. Arch Intern Med. 2003; 163: 2775-2783.
Goode AD, Reeves M, Owen N, Eakin E, G. Results from the dissemination of an evidence-based telephone-delivered intervention for healthy lifestyle and weight loss: the optimal health program. Trans Behav Med. 2013; 3: 340-350.
Yngve A, Nilsson A, Sjostrom M, Ekelund U. Effect of monitor placement and of activity setting on the MTI accelerometer output. Med Sci Sports Exerc. 2003; 35: 320-326.
Cobiac L, Vos T, Veerman L. Cost-effectiveness of Weight Watchers and the Lighten Up to a Healthy Lifestyle program. Aust N Z J Public Health. 2010; 34: 240-247.
Reeves MM, Brakenridge CL, Whelan ME, Eakin EG. Weight loss via the telephone - does it work? A systematic review and meta-analysis. Australia and New Zealand Obesity Society Annual Scientific Meeting; 2014; Sydney.
Jensen MD, Ryan DH, Apovian CM, et al. 2013 AHA/ACC/TOS Guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. Circulation. 2014; 129: S102-S138.
National Health and Medical Research Council. Management of overweight and obesity in adults, adolescents and children: clinical practice guidelines for primary care health professionals. 2013.
Emmons K, Rollnick S. Motivational interviewing in health care settings: opportunities and limitations. Am J Prevent Med. 2001; 20: 68-74.
Rollnick S, Miller W, Butler C. Motivational Interviewing in Health Care. New York: The Guilford Press; 2008.
Bandura A. Social foundations of thought and action: a social cognitive theory. Englewood Cliffs, NJ: Prentice-Hall; 1986.
Borushek A. The CalorieKing Calorie, Fat, and Carbohydrate Counter 2011. USA: Family Health Publications; 2011.
Donnelly JE, Blair SN, Jakicic JM, Manore MM, Rankin JW, Smith BK. American College of Sports Medicine Position Stand. Appropriate physical activity interventoin strategies for weight loss and prevention of weight regain for adults. Med Sci Sports Exerc. 2009; 41: 459-471.
Institute of Medicine of the National Academics. Dietary reference intakes for energy, carbohydrate, fiber, fat, fatty acids, cholesterol, protein, and amino acids. Washington DC. 2005.
Wing R, Hill J. Successful weight loss maintenance. Annu Rev Nutr. 2001; 21: 323-341.
Thorp A, Owen N, Neuhaus M, Dunstan DW. Sedentary behaviours and subsequent health outcomes in adults: a systematic review of longitudinal studies, 1996–2011. Am J Prevent Med. 2011; 41: 207-215.
Slavin JL. Dietary fiber and body weight. Nutrition. 2005; 21: 411-418.
National Heart Lung and Blood Institute. The practical guide: identification, evaluation and treatment of overweight and obesity in adults. In: The North American Association for the Study of Obesity, Bethesda. 2000.
Johnson M, Sallis J, Hovell M. Self-report assessment of walking: effects of aided recall instructions and item order. Meas Phys Educ Exerc Sci. 2000; 4: 141-155.
ActiLife 6.0 [computer program]. Version 6. Pensacola, Florida 2011.
SAS/GRAPH 9.2, Second Edition [computer program]. Cary, NC: SAS Institute Inc.; 2010.
Freedson PS, Melanson E, Sirard J. Calibration of the Computer Science and Applications, Inc. accelerometer. Med Sci Sports Exerc. 1998; 30: 777-781.
Winkler EA, Gardiner PA, Clark BK, Matthews CE, Owen N, Healy GN. Identifying sedentary time using automated estimates of accelerometer wear time. Br J Sports Med. 2012; 46: 436-442.
Swartz A, Strath S, Bassett D, O'Brian W, King A, Ainsworth B. Estimation of energy expenditure using CSA accelerometers at hip and waist sites. Med Sci Sports Exerc. 2000; 32: 450-456.
Reeves M, Winkler E, Eakin E, G. The Fat and Fibre Behaviour Questionnaire: reliability, relative validity and responsiveness to change. Nutrition and Dietetics. 2014 [Epub ahead of print].
Rutishauser IH, Webb K, Abraham B. Evaluation of short dietary questions from the 1995 National Nutrition Survey. In: Australian Government Department of Health and Ageing, Canberra. 2001.
Eakin EG, Reeves MM, Winkler E, et al. Six-month outcomes from living well with diabetes: a randomized trial of a telephone-delivered weight loss and physical activity intervention to improve glycemic control. Ann Behav Med : Publ Soc Behav Med. 2013; 46: 193-203.
Tabachnick BG, Fidell LS. Using Multivariate Statistics. 4th Ed. USA. 2001.
Bendel R, Afifi A. Comparison of stopping rules in forward regression. J Am Stat Assoc. 1977; 72: 46-53.
Vos T, Carter R, Barendregt J, et al. Assessing cost-effectiveness in prevention (ACE-prevention): final report. University of Queensland, Brisbane and Deakin University, Melbourne; 2010.
Forster M, Veerman JL, Barendregt JJ, Vos T. Cost-effectiveness of diet and exercise interventions to reduce overweight and obesity. Int J Obes. 2011; 35: 1071-1078.
Barendregt JJ, Van Oortmarssen GJ, Van Hout BA, Van Den Bosch JM, Bonneux L. Coping with multiple morbidity in a life table. Math Popul Stud. 1998; 7: 29-49.
Australian Institute of Health and Welfare. Health Expenditure Australia 2010–11. Canberra: AIHW;2012.
Dansinger M, Tatsioni A, Wong J, Mei C, Balk E. Meta-analysis: the effect of dietary counseling for weight loss. Ann Intern Med. 2007; 147: 41-47.
Jolly K, Lewis A, Beach J, et al. Comparison of range of commercial or primary care led weight reduction programmes with minimal intervention control for weight loss in obesity: lighten up randomised trial. Br Med J. 2011; 343.
Ski CF, Vale MJ, Bennett GR, et al. Improving access and equity in reducing cardiovascular risk: the Queensland Health model. Med J Aust. 2015; 202: 148-152.
Graves N, Barnett AG, Halton KA, et al. Cost-effectiveness of a telephone-delivered intervention for physical activity and diet. PLoS One. 2009; 4: 7135.
Campbell MK, Carr C, Devellis B, et al. A randomized trial of tailoring and motivational interviewing to promote fruit and vegetable consumption for cancer prevention and control. Ann Behav Med : Publ Soc Behav Med. 2009; 38: 71-85.
Moroshko I, Brennan L, O'Brien P. Predictors of dropout in weight loss interventions: a systematic review of the literature. Obes Rev : Off J Int Assoc Study Obes. 2011; 12: 912-934.
Miller BM, Brennan L. Measuring and reporting attrition from obesity treatment programs: a call to action! Obes Res Clin Pract. 2015; 9: 187-202.
Acknowledgments
This study was supported by a Queensland Health, Health Practitioner Grant (2011). MEW is supported by Australian Postgraduate Award Scholarship. IJH is supported by a Queensland Health, Health Practitioner Research Grant and a Lions Medical Research Fellowship. EGE is supported by a National Health and Medical Research Council Senior Research Fellowship. MMR is supported by a National Breast Cancer Foundation Early Career Fellowship. The authors would like to acknowledge the contribution of clinical staff including Melissa Gwizd, Amy Davis, Louise Cooney, Emily Power, Scott Honeyball and Steven McPhail, as well as the Princess Alexandra Hospital Department of Nutrition and Dietetics and the Department of Diabetes.
Conflict of interest
The authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Implications
Practice: A telephone-based weight loss service may be a feasible, effective and cost-effective alternative service delivery option to an existing group-based program in an acute-care hospital outpatient setting.
Policy: Evaluating alternative and broader-reaching service delivery models for reach, effectiveness and cost-effectiveness is important for decision-making in relation to the allocation of scarce health care resources.
Research: Further research needs to address the significant proportion of patients who remain unengaged with existing weight management services.
An erratum to this article is available at http://dx.doi.org/10.1007/s13142-016-0416-6.
About this article
Cite this article
Whelan, M.E., Goode, A.D., Eakin, E.G. et al. Feasibility, effectiveness and cost-effectiveness of a telephone-based weight loss program delivered via a hospital outpatient setting. Behav. Med. Pract. Policy Res. 6, 386–395 (2016). https://doi.org/10.1007/s13142-015-0337-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13142-015-0337-9