Abstract
The purpose of this study is to determine reduction of door-to-balloon (D2B) time using a single universal guiding catheter (Ikari-Left catheter) in transradial approach. In this procedure, we can skip a total of five steps compared with a conventional procedure (two catheter insertions, two catheter removals, and one catheter engagement). Reducing total ischemic time is important to achieving a better outcome in primary percutaneous coronary intervention (PCI) for ST segment elevation myocardial infarction (STEMI). We retrospectively compared 30 consecutive STEMI patients who underwent transradial primary PCI with a single guiding catheter (IL group) with 30 consecutive patients with conventional transradial primary PCI. Patients with cardiogenic shock, heart failure, or need for intra-aortic balloon pumping support before primary PCI were excluded. Baseline characteristics were not different between the two groups. The D2B time was significantly shorter in the IL group (55 ± 16 vs. 63 ± 17 min, respectively; p = 0.01). Puncture-to-balloon time was also significantly shorter in the IL group (15 ± 11 min vs. 25 ± 11 min, respectively; p = 0.001). The total number of diagnostic and guiding catheters was significantly less in IL group (1 (IQR 1-1) vs. 3 (IQR 3-3), respectively; p < 0.0001). Primary PCI with a single universal guiding catheter reduced D2B time by skipping several procedural steps, and reduced the total number of catheters needed. This technique could reduce patient mortality as well as total medical cost.
Similar content being viewed by others
Introduction
Primary percutaneous coronary intervention (PCI) reduces the mortality rate in patients with acute ST segment elevation myocardial infarction (STEMI) [1, 2]. Shorter door-to-balloon (D2B) time has strong association with a lower mortality rate [3–5]. Based on these data, a D2B time of <90 min has been established as a Class I recommendation in the current guidelines [6, 7]. To reduce the D2B time, many studies have suggested strategies to reduce door-to-catheterization laboratory time [8, 9]. On the other hand, there is still room for improvement to reduce catheterization laboratory-to-balloon time.
Recently, the radial approach in primary PCI has revealed significant clinical benefits in reducing bleeding events and morbidity compared with the femoral approach; however, D2B time with the radial approach was longer than with the femoral approach [10, 11]. Shortening D2B time using the radial approach would be one way to improve STEMI patient outcome. A previous study showed that a high success rate was achieved safely in transradial PCI using a 6-Fr single universal guiding catheter (IL, Ikari-Left catheter; Terumo Corporation, Tokyo, Japan) in elective cases [12]. IL catheter is one of the universal catheters that is feasible for both transradial and transfemoral intervention [13], for both right and left coronary artery [14, 15], and coronary anomalies like high takeoff.
Thus, we developed a hypothesis that a single universal guiding catheter can shorten D2B time compared with the conventional strategy in primary PCI for STEMI.
Methods
Subjects
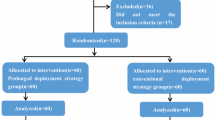
We retrospectively analyzed 30 consecutive patients with STEMI who underwent primary PCI with a single universal guiding catheter (Ikari-left catheter, IL group) at Tokai University Hospital from January 2013 to May 2015. Inclusion criteria were: medical consultation <24 h after symptom onset, chest pain lasting >20 min, ST segment elevation >1 mm in at least two continuous leads, or new left bundle branch block. In the same period, 30 consecutive patients who underwent primary PCI with the transradial approach using diagnostic catheters and a guiding catheter were enrolled as a control group (Conventional group). We excluded patients with persistent pulseless cardiogenic shock, heart failure (Killip > II), or patients needing intra-aortic balloon pumping (IABP) support before the primary PCI. We also excluded patients who could not perform the transradial approach (radial artery was not palpable, abnormal Allen’s test result, or hemodialysis patients with A-V shunt in upper limb). However, radial approach failure and crossover to a femoral approach were not reasons for exclusion.
This study complied with the Declaration of Helsinki in regard to investigation in humans and was approved by the institutional ethics committees at Tokai University Hospital. There was no industry involvement in the design, conduct, financial support, or analysis of this study.
PCI procedure
All patients were pretreated with a loading dose of 300 mg clopidogrel and 200 mg aspirin. Procedural anticoagulation was achieved with preliminary administration of an unfractionated heparin bolus at a dose of 70 IU/kg, supplemented during the procedure to maintain an activated clotting time of >250 s. All patients received 100 mg aspirin once daily for life and 75 mg clopidogrel for at least 6 month after the procedure. Thrombolytic agents and glycoprotein IIb/IIIa inhibitor were not given before the procedure.
In the Conventional group, primary PCI was performed with diagnostic catheters and a guiding catheter. First, a 6-Fr sheath was inserted through radial artery. Right coronary artery angiography was performed with a 4-Fr JR diagnostic catheter (Judkins Right catheter, Asahi Intecc, Nagoya, Japan). After that, the JR diagnostic catheter was removed, and left coronary artery angiography was performed with a JL diagnostic catheter (Judkins Left catheter, Asahi Intecc). After the JL diagnostic catheter was removed, the operator chose the type of guiding catheter and engaged it to the culprit vessel. Type of guiding catheter was at discretion of operators. In the IL group, after 6-Fr sheath insertion through radial artery, angiography of non-culprit coronary artery was performed with a 6-Fr Ikari-Left guiding catheter. After that, the Ikari-Left guiding catheter was disengaged from the non-culprit coronary artery and directly engaged to the culprit coronary artery without catheter exchange (Fig. 1). The timing of changing guiding catheter and approach site was at discretion of operators.
Study endpoints and definition
The primary endpoint of this study was D2B time, which was the time from arrival at the hospital until first device activation in the culprit artery. Secondary endpoints were 30-day incidence of major adverse cardiac event (MACE), hospital stay, and puncture-to-balloon time, which was the time from needle puncture for local anesthesia infusion until first device activation. Data on 30-day outcomes were obtained by direct patient visit or contact with referring physician in the absence of any adverse event. MACE was defined as all-cause death, MI due to acute or sub-acute stent thrombosis, or target lesion revascularization. Cardiac death was defined as any death due to cardiac cause, procedure-related deaths, or death due to unknown cause. New myocardial infarction was defined as new ischemic symptoms lasting >20 min and new or recurrent ST segment elevation or depression >1 mm in at least two contiguous leads, associated with a >20 % increase of the cardiac biomarker values not attributable to the evolution of the index myocardial infarction [16]. Stent thrombosis was classified by the Academic Research Consortium definition as definite, probable, or possible [17].
Statistical analysis
Baseline patient characteristics are summarized with mean ± SD for continuous variables with normal distribution, or median (first to third quartiles) for those continuous but with skewed distribution. The Wilcoxon rank-sum test was used to determine statistically significant differences in clinical parameters between the two groups. Fisher’s exact test was applied to determine the difference between categorical variables. To identify factors that might be related to D2B time, logistic regression models were used. Data were analyzed using JMP version 9.0.0 (SAS Institute Inc., Cary, NC, USA). A p value of <0.05 was considered statistically significant.
Results
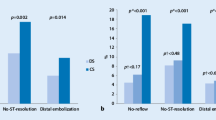
Baseline characteristics and clinical status on arrival are shown in Table 1. There were no statistically significant differences between the groups’ baseline characteristics. Procedural characteristics are shown in Table 2. The D2B time was significantly shorter in the IL group compared with the Conventional group (55 ± 16 vs. 63 ± 17 min, respectively; p = 0.01). Although door-to-puncture time was not significantly different between the two groups (42 ± 17 vs. 40 ± 12 min, respectively; p = 0.7), puncture-to-balloon time was also significantly shorter in the IL group compared with the Conventional group (15 ± 11 vs. 25 ± 11 min, respectively; p = 0.001) (Fig. 2). Logistic regression analysis was performed to identify the clinical factors associated with D2B. In the IL group, temporary pacemaker insertion before PCI and crossover to the femoral artery approach were included as independent variables. Use of the IL was identified as a factor contributing to D2B (β −5.28, 95 % CI −9.68 to −0.88; p = 0.01) (Table 3). In this study, there was no mortality at 30-day or MACE in either group. Length of hospital stay, intensive care unit stay, contrast volume, X-ray exposure time, and peak CK were not significantly different between the groups (Fig. 2).
Door-to-balloon time and puncture-to-balloon time in the IL and Conventional groups. D2B time (55 ± 16 vs. 63 ± 17 min, respectively; p = 0.01) and puncture-to-balloon time (15 ± 11 vs. 25 ± 11 min, respectively; p = 0.001), were significantly shorter in the IL group compared with the Conventional group. D2B door-to-balloon
In the IL group, 2 patients (6.7 %) needed diagnostic catheterization (JR-4) because angiography of non-culprit right coronary artery was difficult to engage with IL catheter; however, all culprit coronary arteries in this group were successfully engaged with an IL catheter. In the Conventional group, 2 patients (6.7 %) needed another type of guiding catheter. The percentage of crossover to the femoral artery due to difficulties with the radial approach was the same (6.7 %) in both groups (Table 2). The total number of catheters used was significantly less in the IL group.
Discussion
In this study, primary PCI with a single universal guiding catheter (Ikari-Left catheter) significantly reduced D2B time compared with the conventional strategy. Also, the total number of catheters used was significantly less.
Using a single universal guiding catheter, we can perform both angiography and primary PCI, meaning we can skip five procedures: two diagnostic catheter insertions, two removals from non-culprit vessel, and one catheter engagement, as shown in Fig. 1. This technique was first reported by Youssef et al. for elective transradial PCI cases, with an extremely high success rate of more than 98 % [12]. Feasibility of this technique compared with transfemoral intervention for STEMI was reported by Chow et al. [18]. In this study, we compared D2B time with conventional transradial intervention, the standard guideline-suggested strategy for STEMI.
Another way to shorten D2B time is by direct primary PCI without diagnostic angiography of non-culprit vessels [19]. However, this strategy may have a serious limitation, as it provides no information of contralateral coronary artery status. We feel that angiography of the non-culprit vessel is informative for ensuring a safe procedure in cases of multiple culprit lesions or multiple coronary artery disease.
In this study, 2 patients (6.7 %) in the IL group had the catheter changed to a diagnostic catheter (JR-4) for angiography of the non-culprit vessel because of the engagement difficulties. In the Conventional group, 2 patients (6.7 %) had the guiding catheter changed for primary PCI; the number of guiding catheters used in the procedure was not significantly different between the two groups (Table 2). A previous study of elective cases showed that both coronary arteries were successfully engaged in 98.1 % of cases with the IL catheter [12]. This difference in results may be due to pressure on the operators in the emergency setting.
The radial approach by an experienced operator in primary PCI has been shown to reduce the incidence of acute bleeding events and is now a Class IIa recommendation in the latest guidelines [7]. However, a weak point of the radial approach has been shown to be longer D2B time than that of femoral approach [10, 11]. Difficulty in puncture, spasm of radial artery, different engagement method for guiding catheters, and arterial anomalies of upper limb artery [20] are reasons for the longer D2B time. According to our findings, the single universal guiding catheter is one of the potential methods for overcoming the limitation of longer D2B time in the radial approach, which could result in a better mortality rate for patients with STEMI.
There are several limitations in this study. This study was a single-center, non-randomized, retrospective analysis, and the sample size was relatively small. Additional prospective randomized controlled trials with larger sample sizes would be necessary to support our findings.
Conclusions
Primary PCI with a single universal guiding catheter significantly reduced not only door-to-balloon time by skipping several procedural steps but also reduced the total number of catheters needed. These findings suggest that this technique could reduce patient mortality rate as well as the total medical costs in treating STEMI.
References
Dalby M, Bouzamondo A, Lechat P, Montalescot G. Transfer for primary angioplasty versus immediate thrombolysis in acute myocardial infarction: a meta-analysis. Circulation. 2003;108:1809–14.
Keeley EC, Boura JA, Grines CL. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomised trials. Lancet. 2003;361:13–20.
Berger PB, Ellis SG, Holmes DR Jr, et al. Relationship between delay in performing direct coronary angioplasty and early clinical outcome in patients with acute myocardial infarction: results from the global use of strategies to open occluded arteries in Acute Coronary Syndromes (GUSTO-IIb) trial. Circulation. 1999;100:14–20.
Cannon CP, Gibson CM, Lambrew CT, et al. Relationship of symptom-onset-to-balloon time and door-to-balloon time with mortality in patients undergoing angioplasty for acute myocardial infarction. JAMA. 2000;283:2941–7.
McNamara RL, Wang Y, Herrin J, et al. Effect of door-to-balloon time on mortality in patients with ST-segment elevation myocardial infarction. J Am Coll Cardiol. 2006;47:2180–6.
O’Gara PT, Kushner FG, Ascheim DD, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;61:e78–140.
Steg PG, James SK, Atar D, et al. ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J. 2012;33:2569–619.
Bradley EH, Herrin J, Wang Y, et al. Strategies for reducing the door-to-balloon time in acute myocardial infarction. N Engl J Med. 2006;355:2308–20.
Diercks DB, Kontos MC, Chen AY, et al. Utilization and impact of pre-hospital electrocardiograms for patients with acute ST-segment elevation myocardial infarction: data from the NCDR (National Cardiovascular Data Registry) ACTION (Acute Coronary Treatment and Intervention Outcomes Network) Registry. J Am Coll Cardiol. 2009;53:161–6.
Jolly SS, Yusuf S, Cairns J, et al. Radial versus femoral access for coronary angiography and intervention in patients with acute coronary syndromes (RIVAL): a randomised, parallel group, multicentre trial. Lancet. 2011;377:1409–20.
Romagnoli E, Biondi-Zoccai G, Sciahbasi A, et al. Radial versus femoral randomized investigation in ST-segment elevation acute coronary syndrome: the RIFLE-STEACS (Radial Versus Femoral Randomized Investigation in ST-Elevation Acute Coronary Syndrome) study. J Am Coll Cardiol. 2012;60:2481–9.
Youssef AA, Hsieh YK, Cheng CI, Wu CJ. A single transradial guiding catheter for right and left coronary angiography and intervention. EuroIntervention. 2008;3:475–81.
Murakami T, Masuda N, Torii S, et al. The efficacy and feasibility of chronic total occlusion by transradial intervention: a Japanese single-center retrospective study. J Invasive Cardiol. 2015;27:E177–81.
Ikari Y, Nagaoka M, Kim JY, Morino Y, Tanabe T. The physics of guiding catheters for the left coronary artery in transfemoral and transradial interventions. J Invasive Cardiol. 2005;17:636–41.
Ikari Y, Masuda N, Matsukage T, et al. Backup force of guiding catheters for the right coronary artery in transfemoral and transradial interventions. J Invasive Cardiol. 2009;21:570–4.
Thygesen K, Alpert JS, Jaffe AS, et al. Third universal definition of myocardial infarction. Circulation. 2012;126:2020–35.
Cutlip DE, Windecker S, Mehran R, et al. Clinical end points in coronary stent trials: a case for standardized definitions. Circulation. 2007;115:2344–51.
Chow J, Tan CH, Tin AS, et al. Feasibility of transradial coronary angiography and intervention using a single Ikari left guiding catheter for ST elevation myocardial infarction. J Interv Cardiol. 2012;25:235–44.
Plourde G, Abdelaal E, Bataille Y, et al. Effect on door-to-balloon time of immediate transradial percutaneous coronary intervention on culprit lesion in ST-elevation myocardial infarction compared to diagnostic angiography followed by primary percutaneous coronary intervention. Am J Cardiol. 2013;111:836–40.
Fujii T, Masuda N, Tamiya S, et al. Angiographic evaluation of right upper-limb arterial anomalies: implications for transradial coronary interventions. J Invasive Cardiol. 2010;22:536–40.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study complied with the Declaration of Helsinki in regard to investigation in humans and was approved by the institutional ethics committees at Tokai University Hospital. There was no industry involvement in the design, conduct, financial support, or analysis of this study.
Conflict of interest
Yuji Ikari, MD receives a royalty fee from Terumo Corporation. All other authors have no conflict of interests.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Torii, S., Fujii, T., Murakami, T. et al. Impact of a single universal guiding catheter on door-to-balloon time in primary transradial coronary intervention for ST segment elevation myocardial infarction. Cardiovasc Interv and Ther 32, 114–119 (2017). https://doi.org/10.1007/s12928-016-0395-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12928-016-0395-z