Abstract
Background
Primary percutaneous coronary intervention (PPCI) is the standard procedure for reperfusion for ST-segment elevation myocardial infarction (STEMI), but the occurrence of the no-reflow phenomenon remains common and is associated with adverse outcomes.
Aims
This study aimed to evaluate whether prolonged balloon inflation in stent deployment would lessen the occurrence of the no-reflow phenomenon in PPCI compared with conventional rapid inflation/deflation strategy.
Methods
Patients were randomly assigned to either the prolonged balloon inflation in stent deployment group (PBSG) or conventional deployment strategy group (CDSG) in a 1:1 ratio. A subset of patients was included in the cardiac magnetic resonance (CMR) assessment.
Results
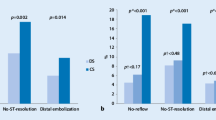
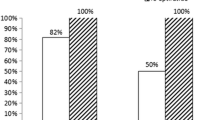
Thrombolysis in MI (TIMI) flow grade 3 was found in 96.7% and 63.3% of the patients of the PBSG and CDSG, respectively (P = 0.005). The results of the PBSG and CDSG are respectively shown as follows: 0% versus 30% no-reflow or slow flow (P = 0.002); 90% versus 66.7% ST-segment resolution ≥ 50% (P = 0.028); 35.6 ± 14.5 frames versus 49.18 ± 25.2 frames on corrected TIMI frame count (P = 0.014); and 60% versus 20% myocardial blush grade 3 (P = 0.001). At 1 month, the major cardiovascular adverse event (cardiovascular mortality) rate was 3.3% in both groups; at 1 year, the rate was 3.3% and 6.7% for the PBSG and CDSG, respectively (P = 1.00). In the CMR subset of cases, the presence of microvascular obstruction (MVO) was detected in 6.7% and 50% of the patients in the PBSG and CDSG, respectively (P = 0.023).
Conclusion
In our pilot trial, prolonged balloon inflation during stent deployment strategy in PPCI reduces the occurrence of the no-reflow phenomenon in patients with STEMI and improved the myocardial microcirculation perfusion (ClinicalTrials.gov number: NCT03199014; registered: 26/June/2017).
Similar content being viewed by others
Background
Although the use of primary percutaneous coronary intervention (PPCI) for ST-segment elevation myocardial infarction (STEMI) in China has increased in recent decades, the in-hospital mortality and long-term prognosis of patients has not significantly changed [1]. Coronary no-reflow is defined as a phenomenon in which, despite revascularization therapy with PPCI, the cardiac tissue fails to normally perfuse and has a negative effect on outcomes, negating the potential benefits of PPCI [2,3,4,5].
The pathophysiology of the no-reflow phenomenon is multifactorial, and it is now referred to as microvascular obstruction (MVO), which includes injuries related to ischemia, reperfusion, endothelial cell edema, thrombus embolization, and embolization of atherosclerotic plaque fragments [6]. Therefore, these injuries are of concern during PPCI [7]. In theory, the manipulation of factors during PPCI may contribute to no-reflow; however, the balloon pressure, inflation time, repeated balloon dilations, and stent number did not affect the incidence of no-reflow in a retrospective analysis [8]. In small vessels, it is possible that the stent itself affixes the thrombus to the vessel wall, especially if the thrombus is more fibrous [9].
The duration of stent inflation has a significant impact on stent expansion, and rapid inflation/deflation may not be sufficient to fully expand the stent [10, 11]. Therefore, a fully expanded stent may entrap the atherothrombus under the struts that are more fixed and reduce distal embolization in PPCI. However, this hypothesis has not been thoroughly investigated in randomized controlled trial (RCT) studies. The present study was undertaken to evaluate whether prolonged balloon inflation during stent deployment strategy would lessen the occurrence of the no-reflow phenomenon in PPCI compared with the conventional rapid inflation/deflation strategy.
Materials and methods
Trial design and study participants
We conducted this single-center, randomized, single-blinded, parallel pilot trial to compare prolonged balloon inflation during stent deployment group (PBSG) (the stent was deployed with a single balloon inflation, and low-pressure inflation was sustained for > 30 s after the target balloon inflation pressure had been achieved. If the patient could not tolerate the procedure, showed signs of ischemia, or had chest pain, arrhythmia, or a decrease in blood pressure, the stent balloon was immediately deflated) with the conventional deployment strategy group (CDSG) (as a control group, in which the stent balloon inflation time was less than 10 s. Additional dilation, expansion pressure, and post dilation were left to the discretion of operators). Randomization was performed using a simple random sampling method generated by a computer program. The random allocation list was enclosed in sequentially numbered, opaque, and sealed envelopes. The eligible patients were assigned to the PBSG or CDSG in a 1:1 ratio. The trial design was approved by the Regional Ethics Review Board of West China Hospital. The research paper is written in accordance with the international CONSORT 2010 statement [12].
The patients were eligible for enrollment if they met the following criteria: (1) age ≥ 18 years; (2) patients with STEMI who were referred to PPCI within 12 h after the onset of symptoms and with ST-segment elevation ≥ 1 mm in ≥ 2 contiguous leads or a presumed new left bundle branch block or a true posterior MI; and (3) admission within 12 h of symptom onset or admission between 12 and 24 h if there was evidence of continuing ischemia. The exclusion criteria were as follows: cardiogenic shock, an intra-aortic balloon pump implant, or extracorporeal membrane oxygenation; thrombolysis; previous myocardial infarction; severe valvular disease; coronary artery bypass grafting; renal dysfunction (glomerular filtration rate of < 30 mL/min/1.73 m2); cardiomyopathy; congenital heart disease; malignant arrhythmia; chronic obstructive pulmonary disease; pregnancy; a contraindication to cardiac magnetic resonance (CMR) imaging (e.g., pacemaker and claustrophobia); and inability to give informed consent.
Procedures
Following coronary angiography (CAG), the patients who fulfilled the inclusion criteria were randomly assigned to PBSG or CDSG during PPCI. All patients received 300 mg oral aspirin and 600 mg clopidogrel (or 180 mg ticagrelor) as soon as STEMI was confirmed. The prescription of anticoagulants, glycoprotein IIb/IIIa inhibitors, and thrombus aspiration was left to the physician’s discretion. The patients were immediately taken to the cardiac catheterization lab. If the operator predicted that direct stenting was possible, predilation was not performed. If direct stenting was impossible, predilation with a single low-pressure inflation was performed. In all patients, only the infarct-related artery was treated. All procedures undergone by the patients in the study were performed by experienced cardiologists who were trained by the National Coronary Intervention Training Bases. All operations were performed according to the standardized procedures. Less than 10% residual stenosis was considered as the ideal stent implantation.
All placed stents were drug-eluting stents, and the patients were given the option to choose between two commercially available drug-eluting stents: the PROMUS Element stent (Boston Scientific, Boston, Massachusetts, USA) or a GuReater stent (Lepu, China). The diameters of the stents and balloons were selected by visual estimation to achieve a balloon/vessel ratio of 1:1 for both study groups. After stent implantation, if the no-reflow phenomenon occurred, pharmacological intervention, including common vasodilators (nitroprusside and/or diltiazem), was administered.
End points, assessment of outcomes, and definitions
The primary outcome of this study was the incidence of the no-reflow phenomenon according to thrombolysis in MI (TIMI) flow grade, a grading system used to evaluate blood flow. TIMI 0 is defined as no antegrade flow beyond the point of occlusion. TIMI 1 is defined as faint antegrade flow beyond the occlusion with incomplete filling of the distal vascular bed. TIMI 2 is defined as delayed antegrade flow with complete filling of the distal vascular bed. TIMI 3 is defined as normal flow with complete filling of the distal vascular bed. The no-reflow phenomenon was defined as TIMI flow grade < 3 and as myocardial blushing grade (MBG) < 2. The MBG is used to assess the filling and clearance of contracts in the myocardium. MBG 0 is defined as no apparent tissue-level perfusion in the distribution of the culprit artery. MBG 1 is defined as no clearance from the microvasculature. MBG 2 is defined as blush beginning to clear during washout [13], and MBG 3 is defined as normal myocardial blush or contrast density, comparable with that obtained during angiography of a contralateral or ipsilateral non-infarct-related coronary artery. The patients with no-reflow had serious outcomes, characterized by a significant increase in the incidence of congestive heart failure, cardiogenic shock, and death [14]. Two experienced cardiologists independently assessed the occurrence of no-reflow after stent implantation, TIMI flow grade, TIMI frame count, and MBG on the most recent angiogram. The number of angiogram frames required for the dye to reach a specified distal segment in the coronary artery was referred to as the corrected TIMI frame count [15]. All angiograms were recorded on a 21-mm cine film at 15 frames/second (UNIQ FD 10, Philips, USA). The thrombus burden was evaluated by the TIMI thrombus scale, which was classified as a grade between 0 and 5 [16]. The electrocardiographic resolution of the ST-segment elevation was defined as a reduction of > 50% of the ST-segment elevation in the same lead within 60 min after the index procedure [17].
The secondary outcomes were major adverse cardiovascular events, which were defined as any events of target vessel revascularization (TVR), recurrent MI, or cardiovascular mortality. These outcomes were examined 30 days and 1 year after the PPCI. The procedure time, total fluoroscopy time, and radiation dose were also assessed. The safety outcome of major bleeding was defined using a definition of major bleeding from the International Society on Thrombosis and Haemostasis [18]; the bleeding events that were not considered as major were considered as minor bleeding.
A subset of patients was included in the CMR examination approximately 3–5 days after the index procedure. The criteria among those who received CMR were infarct-related artery ≥ 2.5 mm in diameter and age > 18 years who provided informed consent was obtained for CMR. The exclusion criteria were as follows: cardiogenic shock, an intra-aortic balloon pump implant, or extracorporeal membrane oxygenation; thrombolysis; previous myocardial infarction; severe valvular disease; coronary artery bypass grafting; renal dysfunction (glomerular filtration rate of < 30 mL/min/1.73 m2); cardiomyopathy; congenital heart disease; malignant arrhythmia; chronic obstructive pulmonary disease; pregnancy; a contraindication to cardiac magnetic resonance (CMR) imaging (e.g., pacemaker and claustrophobia); and inability to give informed consent. Next, the infarct size, myocardial salvage index, presence and extent of MVO, myocardium hemorrhage, myocardial edema, and left ventricular ejection fraction (LVEF, was calculated by subtracting the volume at end systole from the volume at end diastole and dividing the result by the volume at end diastole) and left ventricular (LV) volume were assessed. The examinations were performed on a 3.0-T whole-body scanner with an 18-element body phased array coil (Skyra; Siemens Medical Solutions, Erlangen, Germany). Standard two-, three-, and four-chamber cine images were acquired using a TrueFISP sequence. The area at risk was assessed on the initial examination using a T2-weighted short-tau inversion recovery sequence. The infarct size, LVEF, and LV volume were assessed on both examinations using delayed, contrast-enhanced, electrocardiogram-triggered inversion recovery images and steady-state free precession cine images. The myocardial salvage index was calculated as [area at risk (mass) − infarct size (mass)]/area at risk (mass). The delayed contrast-enhanced images were obtained 10 min after an intravenous injection of 0.1 mmol/kg body weight gadolinium-based contrasts (Gadovist, Bayer Schering, Berlin, Germany). All images were obtained in the short-axis plane, with 8-mm slices without gaps covering the entire LV [19,20,21].
A subgroup analysis was prespecified to examine the factors associated with an increased risk of the no-reflow phenomenon, which were comprised of the following: age (≥ 65 and < 65 years), thrombus burden, thrombosis aspiration, direct stenting, infarct location (anterior and nonanterior), multiple complex lesions, and door-to-balloon time.
Statistical analysis
On the basis of the previous research, no-reflow phenomenon was observed in 32% of the patients following PPCI for acute MI (AMI). No-reflow was defined as TIMI < 3 and as MBG < 2. Some studies on the current routine interventions for the no-reflow phenomenon in STEMI, such as the REOPEN-AMI study, showed that the additional intracoronary administration of adenosine results in a significantly reduced no-reflow by 12%, which was similar to the TAPAS study in which thrombus aspiration was evaluated. We calculated that a sample size of 53 patients in each group would provide the trial with a power of at least 80% and a two-side alpha of 5% to reject the null hypothesis of no difference between the groups, assuming that the adopted relative risk (RR) reduction of the primary outcome was 22% in the PBSG. Under an assumption that about 20% of the patients would be lost to follow, a total of 120 patients was deemed to be sufficient to evaluate the primary outcome. The data are expressed as percentages and means (standard deviations). The categorical variables were compared using the Chi-square test at a two-sided significance level of 5%. The continuous variables were compared using t test or analysis of variance. A P value < 0.05 was considered statistically significant. All statistical analyses were performed using the SPSS 17.0 software (SPSS Inc., Chicago, Illinois, USA).
Result
Patient characteristics
Between November 2016 and May 2018, 156 patients with STEMI were considered for inclusion, of which 120 were enrolled according to the eligibility criteria (Fig. 1). After CAG, the patients were randomly assigned into either PBSG (n = 60) or CDSG (n = 60) during PPCI. The baseline clinical characteristics were similar in both groups (Table 1). The procedural and angiographic characteristics of the study patients are shown in Table 1. After undergoing randomization, the mean inflation time was 35.87 and 10.07 s in the PBSG and CDSG, respectively. None of the patients who underwent randomization were lost to follow-up.
Procedural outcomes
Primary outcome
The proportion of patients with an immediate TIMI flow grade < 3 was lower in the PBSG than that in the CDSG after stent deployment (3.3% vs. 36.6%, respectively, P = 0.005) (Table 2). The no-reflow proportion of patients was lower in the PBSG than that in the CDSG (0% vs. 30%, respectively, P = 0.002). The corrected TIMI frame count was lower in the PBSG than that in the CDSG (35.6 ± 14.5 vs. 49.18 ± 25.2, respectively, P = 0.014), and more patients in the PBSG had ST-segment resolution ≥ 50% than that in the CDSG (90% vs. 66.7%, respectively, P = 0.028). The percentage of patients who achieved an MBG of 3 was higher in the PBSG than that in the CDSG (60% vs. 20%, P = 0.001).
Secondary outcome
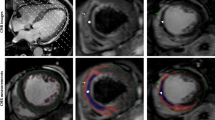
There was no significant difference in the procedure time, radiation exposure time, or contrast volume between the two groups. The number of bleeding events and clinical end points were also not significantly different between the two groups (Table 2). The result of the subgroup analysis (Fig. 2) showed that male patients (RR = 1.46; 95% confidence interval [CI] = 1.09–1.94), non-thrombectomy (RR = 1.40; 95% CI = 1.05–1.86), high thrombus burden (RR = 1.52; 95% CI = 1.07–2.16), door-to-balloon time < 90 min (RR = 1.81; 95% CI = 1.24–2.64), and non-anterior wall infarction (RR = 2.53; 95% CI = 1.60–4.02) had a lower risk for no-reflow phenomenon, which favors PBSG (P for interaction = 0.07). According to the CMR subset, the PBSG can reduce the incidence of MVO and improve cardiac function (Table 3, Fig. 3).
Cardiac magnetic resonance image. The top row was from a patient who under prolonged balloon inflation during stent deployment strategy, there is no imaging features of microvascular obstruction (MVO). Bottom row was from a patient with anteroseptal infarct who under conventional deployment strategy, there is imaging features of MVO (asterisk *)
Discussion
To the best of our knowledge, this study is the first to investigate the effect of prolonged balloon inflation during stent deployment strategy in PPCI. We designed this proof-of-concept pilot study to determine whether prolonged balloon inflation during stent deployment or rapid balloon inflation strategies could provide more short- and long-term benefits for patients with STEMI. The major findings of the present study were as follows: (1) the prolonged balloon inflation strategy lessened the occurrence of the no-reflow phenomenon and improved the myocardial microcirculation perfusion, but the difference between 30-day and 1 year clinical outcomes is not observed; (2) there were no significant differences between the study groups in terms of the procedure time, radiation exposure time, and number of bleeding events; (3) according to the subset analysis, it seems that the prolonged balloon inflation strategy was more effective in patients who were male and had a thrombectomy, heavy thrombosis burden, and non-anterior wall infraction; and (4) as evaluated by the CMR subset, the prolonged balloon inflation strategy can reduce the incidence of MVO and improve cardiac function.
In the early days of coronary angioplasty, an auto perfusion balloon angioplasty catheter was used for long balloon inflation, which was based on the hypothesis that the loose flap of dissection may be definitively “tacked back” and might deliver a better result [22,23,24]. Another study found that approximately half of patients whose initial angioplasty failed could be treated by prolonged balloon dilation [25]. With the wide application of stents, this technique was not used. Subsequently, an in vitro study investigated the duration of balloon inflation for optimal stent deployment [10, 11]. Prolonged balloon inflation could have a significant impact on stent expansion and strut apposition, as evaluated by intravascular ultrasound or optical coherence tomography [26,27,28]. However, these studies were not limited to patients with STEMI.
Despite the use of PPCI and the development of emergency transports resulting in shorter ischemic times, STEMI-related mortality remains considerable [29]. The no-reflow phenomenon can offset, at least in part, the benefits of PPCI [30]. Coronary microvascular dysfunction plays a key role in the development of the no-reflow phenomenon [31], which occurs in approximately 50% of patients with STEMI after PPCI [21]. Thrombotic material and thromboembolisms will distally travel, either spontaneously or at the time of PPCI, when an angioplasty balloon is expanded or a stent is deployed [3]. The debris released from a PPCI can also include soluble substances, such as vasoactive agents or inflammatory mediators that may stimulate microvascular arteriolar spasms [32, 33]. Thus, removing an intravascular thrombus using an extraction catheter during the procedure to reduce atherothrombotic embolization is an active strategy that has been evaluated in RCT and meta-analysis [34]. Although there were negative results from the TASTE and TOTAL trials and recent guidelines no longer recommend routine aspiration for STEMI [35, 36], neither study have allowed us to rule out the possibility that thrombus aspiration might be beneficial in high-risk patients [37, 38]. However, with more than 30% of patients showing minimal particles after thrombectomy and persistent residual thrombus in in vitro models, distal embolization may not fully prevent thrombectomy [39, 40]. Direct stenting is another strategy to reduce the risk of distal embolization of thrombus fragments [41, 42]. A meta-analysis found that direct stenting significantly reduced the short-term and 1-year mortality and the after-procedural no-reflow phenomenon [43]. However, few of these studies have been limited to patients with STEMI. The Thrombectomy Trialists Collaboration conducted a patient-level meta-analysis and found that direct stenting was not significantly associated with improved clinical outcomes compared with conventional stenting among patients with STEMI undergoing PPCI [44]; approximately 37% of the patients in that study underwent direct stenting [45]. In our study, direct stenting and thrombectomy were performed more often in the PBSG than in the CDSG (50% and 33.3%, respectively), but the differences were not significant. Although the data from the Thrombectomy Trialists Collaboration affirm the facilitation of direct stenting by aspiration thrombectomy, there was no significant interaction between thrombus aspiration and any of the clinical outcome variables investigated [45]. According to our subset analysis, patients with thrombectomy and a heavy thrombosis burden may have better angiographic myocardial reperfusion outcomes, but there was not enough statistical power to confirm this, and the interaction was not excluded.
In the present study, prolonged balloon inflation during stent deployment may work through the following mechanisms. First, a long balloon inflation time with low pressure could reduce the iatrogenic rupture of thin-cap fibroatheroma through stent expansion, which induces distal embolization, particularly in lesions with low-echoic structures and large amounts of atherosclerotic plaque with vulnerable components. Second, although thrombectomy may reduce the thrombus burden, persistent residual thrombus may also cause distal embolization [39]. When added to direct stenting, the loosened atherothrombus material was affixed to the vessel wall under the stent struts. However, incomplete stent deployment and inadequate apposition may weaken the “confinement effect” for atherothrombus material. Therefore, the conventional rapid balloon inflation/deflation strategy was not enough [10], especially in the PPCI setting in which postdilation should be avoided. Third, prolonged balloon inflation may be analogous to the postcondition that was performed within one minute of reflow by brief episodes of reversible ischemia reperfusion during angioplasty. A meta-analysis found that postconditioning following PPCI induced by transient coronary ischemia in patients with STEMI may reduce myocardial injury biomarkers and improve cardiac function [46]. However, the POST and DANAMI 3-iPOST trials found that ischemic postconditioning did not improve myocardial reperfusion and clinical outcomes [47, 48]. The primary end point results contribute to the theory that the postconditioning algorithm, in which postconditioning is instituted after a very short reperfusion time, might be a more effective method. In the present study, if the occlusion persisted for more than 30 s after the stent was deployed, the conditioning therapy was completed before reperfusion injury could occur. Therefore, this postconditioning algorithm may be effective.
The indices of angiography for evaluating coronary microvascular circulation in the cardiac catheterization laboratory are semiquantitative and can be subjective. CMR is the gold standard when assessing the MVO, MI size, LV volume, and LVEF, but it is expensive and not yet widely available. The areas of no-reflow have been associated with MVO, as seen on magnetic resonance images, and correlate with a higher degree of myocardial damage. Therefore, in the present study, we designed a subset of CMR to assess the no-reflow phenomenon after PPCI. Approximately 50% of the patients included in this study underwent CMR. The incidence of MVO was 50% in the CDSG and was consistent with previous studies [49]. The prolonged balloon inflation strategy could reduce the incidence of MVO and improve cardiac function, but not infarction size, as evaluated by CMR. The no-reflow phenomenon is associated with poor healing of the infarct scar, including thinner scars and more infarct expansion; therefore, it appears that some therapies can reduce no-reflow without reducing infarct size [50].
Limitations
This study has the following limitations. Firstly, the study represents a single-center experience using surrogate end points with a relatively small sample that was underpowered to detect significant differences in the clinical end points. However, this trial implemented rigorous inclusion and exclusion criteria to reduce the risk of confounding bias. The primary outcome (the incidence of the no-reflow phenomenon) was well correlated with subsequent mortality in patients with STEMI. Even when transient, no-reflow during PPCI was associated with poor short- and long-term outcomes. In the future, large randomized clinical trials are necessary to confirm the efficacy of this new approach. Second, because high-risk patients with more complex lesions and unstable hemodynamics were excluded, the results cannot be applied to all patients with STEMI. Third, there may be selection bias in the CMR subset group because there was no randomization between the groups. Because limited by research funding, a randomization was not performed, and some patients did not obtain informed consent. Hence, the results of the CMR subset group should be interpreted with caution. Nonetheless, our study was the first to evaluate this novel approach for STEMI, which can contribute to the value of our trial. Fourth, the dual antiplatelet therapy (DAPT) is vital in patients with acute STEMI undergoing PPCI. But recently, an individual patient level meta-analysis found that aspirin cessation from 1 to 3 months after coronary revascularization and continuation with P2Y12 inhibitor monotherapy may be warranted instead of continuation of DAPT, especially it was associated with lower rates of major bleeding compared with DAPT [51]. In present study, the antiplatelet strategies did not detailed description in baseline characteristics and following up after PCI, this may be a confounding factor for 1 year clinical outcomes. At the same time, whether this treatment strategy has an impact on no reflow phenomenon has not been included in this study, this is one of the limitations in our study.
Conclusions
In our pilot trial, prolonged balloon inflation during stent deployment strategy during PPCI could lessen the occurrence of the no-reflow phenomenon and improve the myocardial microcirculation perfusion in patients with STEMI. However, these data are preliminary, and large-sample RCTs with a long-term follow-up period are needed to confirm this result.
Availability of data and materials
The dataset analyzed in the current study is not publicly available because of the lack of consent from the study participants, but it is available from the corresponding author on reasonable request for researchers who meet the criteria for access to confidential data.
References
Li J, Li X, Wang Q, Hu S, Wang Y, Masoudi FA, et al. ST-segment elevation myocardial infarction in China from 2001 to 2011 (The China PEACE-Retrospective Acute Myocardial Infarction Study): a retrospective analysis of hospital data. Lancet. 2015;385:441–51.
Kloner RA, King KS, Harrington MG. No-reflow phenomenon in the heart and brain. Am J Physiol Heart Circ Physiol. 2018;315(3):H550–62.
Rezkalla SH, Stankowski RV, Hann J, Kloner RA. Management of no-reflow phenomenon in the catheterization laboratory. JACC Cardiovasc Interv. 2017;10:215–23.
Allencherril J, Jneid H, Atar D, Alam M, Levine G, Kloner RA, et al. Pathophysiology, diagnosis, and management of the no-reflow phenomenon. Cardiovasc Drugs Ther. 2019;33:589–97.
Kloner RA. No-reflow phenomenon: maintaining vascular integrity. J Cardiovasc Pharmacol Ther. 2011;16(3):244–50.
Reffelmann T, Kloner RA. Microvascular alterations after temporary coronary artery occlusion: the no-reflow phenomenon. J Cardiovasc Pharmacol Ther. 2004;9(3):163–72.
Kloner RA. The importance of no-reflow/microvascular obstruction in the STEMI patient. Eur Heart J. 2017;38(47):3511–3.
Zhou H, He XY, Zhuang SW, Wang J, Lai Y, Qi WG, et al. Clinical and procedural predictors of no-reflow in patients with acute myocardial infarction after primary percutaneous coronary intervention. World J Emerg Med. 2014;5:96–102.
Yip HK, Chen MC, Chang HW, Hang CL, Hsieh YK, Fang CY, et al. Angiographic morphologic features of infarct-related arteries and timely reperfusion in acute myocardial infarction: predictors of slow-flow and no-reflow phenomenon. Chest. 2002;122:1322–32.
Hovasse T, Mylotte D, Garot P, Salvatella N, Morice MC, Chevalier B, et al. Duration of balloon inflation for optimal stent deployment: 5 s is not enough. Catheter Cardiovasc Interv. 2013;81:446–53.
Vallurupalli S, Bahia A, Ruiz-Rodriguez E, Ahmed Z, Hakeem A, Uretsky BF. Optimization of stent implantation using a high pressure inflation protocol. Catheter Cardiovasc Interv. 2016;87:65–72.
Schulz KF, Altman DG, Moher D, CONSORT Group. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. BMJ. 2010;340:c332.
van’t Hof AW, Liem A, Suryapranata H, Hoorntje JC, de Boer MJ, Zijlstra F. Angiographic assessment of myocardial reperfusion in patients treated with primary angioplasty for acute myocardial infarction: myocardial blush grade. Zwolle Myocardial Infarction Study Group. Circulation. 1998;97(23):2302–6.
Gibson CM, Murphy SA, Rizzo MJ, Ryan KA, Marble SJ, McCabe CH, et al. Relationship between TIMI frame count and clinical outcomes after thrombolytic administration. Thrombolysis in Myocardial Infarction (TIMI) Study Group. Circulation. 1999;99(15):1945–50.
Rezkalla SH, Stankowski RV, Hanna J, Kloner RA. Management of no-reflow phenomenon in the catheterization laboratory. JACC Cardiovasc Interv. 2017;10:215–23.
Gibson CM, de Lemos JA, Murphy SA, Marble SJ, McCabe CH, Cannon CP, et al. Combination therapy with abciximab reduces angiographically evident thrombus in acute myocardial infarction: a TIMI 14 substudy. Circulation. 2001;103(21):2550–4.
de Lemos JA, Antman EM, Giugliano RP, McCabe CH, Murphy SA, Van de Werf F, et al. ST-segment resolution and infarct-related artery patency and flow after thrombolytic therapy. Thrombolysis in Myocardial Infarction (TIMI) 14 investigators. Am J Cardiol. 2000;85(3):299–304.
Schulman S, Kearon C. Definition of major bleeding in clinical investigations of antihemostatic medicinal products in non-surgical patients. J Thromb Haemost. 2005;3(4):692–4.
Bonanad C, Monmeneu JV, Lopez-Lereu MP, Hervas A, de Dios E, Gavara J, et al. Prediction of long-term major events soon after a first ST-segment elevation myocardial infarction by cardiovascular magnetic resonance. Eur J Radiol. 2016;85(3):585–92.
Husser O, Monmeneu JV, Sanchis J, Nunez J, Lopez-Lereu MP, Bonanad C, et al. Cardiovascular magnetic resonance-derived intramyocardial hemorrhage after STEMI: influence on long-term prognosis, adverse left ventricular remodeling and relationship with microvascular obstruction. Int J Cardiol. 2013;167(5):2047–54.
van Kranenburg M, Magro M, Thiele H, de Waha S, Eitel I, Cochet A, et al. Prognostic value of microvascular obstruction and infarct size, as measured by CMR in STEMI patients. JACC Cardiovasc Imaging. 2014;7(9):930–9.
Colle JP, Delarche N. PTCA with side-by-side balloon using fixed guide wire systems: a potential alternative autoperfusion device—an in vitro study. Cathet Cardiovasc Diagn. 1992;27(4):303–8.
de Muinck ED, den Heijer P, van Dijk RB, Crijns HJ, Hillege HJ, Twisk SP, et al. Autoperfusion balloon versus stent for acute or threatened closure during percutaneous transluminal coronary angioplasty. Am J Cardiol. 1994;74(10):1002–5.
Turic ZG, Campbell CA, Gottimukkala MV, Kloner RA. Preservation of distal coronary perfusion during prolonged balloon inflation with an autoperfusion angioplasty catheter. Circulation. 1987;75(6):1273–80.
van der Linden LP, Bakx AL, Sedney MI, Buis B, Bruschke AV. Prolonged dilation with an autoperfusion balloon catheter for refractory acute occlusion related to percutaneous transluminal coronary angioplasty. J Am Coll Cardiol. 1993;22(4):1016–23.
Asano T, Kobayashi Y, Fukushima K, Iwata Y, Kitahara H, Ishio N, et al. Effect of balloon inflation time on expansion of sirolimus-eluting stent. Heart Vessels. 2009;24(5):335–9.
Hee Ann S, Chung JW, De Jin C, Ho Lee J, Min Kim J, Garg S, et al. Better inflation time of stent balloon for second-generation drug-eluting stent expansion and apposition: an optical coherence tomography study. J Interv Cardiol. 2014;27(2):171–6.
Cook JR, Mhatre A, Wang FW, Uretsky BF. Prolonged high-pressure is required for optimal stent deployment as assessed by optical coherence tomography. Catheter Cardiovasc Interv. 2014;83(4):521–7.
Torabi A, Cleland JGF, Khan NK, Loh PH, Clark AL, Alamgir F, et al. The timing of development and subsequent clinical course of heart failure after a myocardial infarction. Eur Heart J. 2008;29(7):859–70.
Brosh D, Assali AR, Mager A, Porter A, Hasdai D, Teplitsky I, et al. Effect of no-reflow during primary percutaneous coronary intervention for acute myocardial infarction on 6-month mortality. Am J Cardiol. 2007;99(4):442–5.
Durante A, Camici PG. Novel insights into an “old” phenomenon: the no reflow. Int J Cardiol. 2015;187:273–80.
Hildebrandt HA, Patsalis PC, Al-Rashid F, Neuhäuser M, Rassaf T, Heusch G, et al. Quantification and characterisation of released plaque material during bioresorbable vascular scaffold implantation into right coronary artery lesions by multimodality intracoronary imaging. EuroIntervention. 2016;12(12):1481–9.
Kleinbongard P, Konorza T, Böse D, Baars T, Haude M, Erbel R, et al. Lessons from human coronary aspirate. J Mol Cell Cardiol. 2012;52(4):890–6.
Dominguez AC, Bittl JA, El-Hayek G, Contreras E, Tamis-Holland JE. Meta-analysis of randomized controlled trials comparing percutaneous coronary intervention with aspiration thrombectomy versus conventional percutaneous coronary intervention during ST-segment elevation myocardial infarction. Catheter Cardiovasc Interv. 2016;87(7):1203–10.
Fröbert O, Lagerqvist B, Olivecrona GK, Omerovic E, Gudnason T, Maeng M, et al. Thrombus aspiration during ST-segment elevation myocardial infarction. N Engl J Med. 2013;369(17):1587–97.
Jolly SS, Cairns JA, Yusuf S, Meeks B, Pogue J, Rokoss MJ, et al. Randomized trial of primary PCI with or without routine manual thrombectomy. N Engl J Med. 2015;372(15):1389–98.
Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39(2):119–77.
Crea F. Coronary microvascular obstruction—a puzzle with many pieces. N Engl J Med. 2015;372(15):1464–5.
Serdoz R, Pighi M, Konstantinidis NV, Kilic ID, Abou-Sherif S, Di Mario C. Thrombus aspiration in primary angioplasty for ST-segment elevation myocardial infarction. Curr Atheroscler Rep. 2014;16(8):431.
Müller-Hülsbeck S, Grimm J, Leidt J, Jahnke T, Heller M. Comparison of in vitro effectiveness of mechanical thrombectomy devices. J Vasc Interv Radiol. 2001;12(10):1185–91.
Barbato E, Marco J, Wijns W. Direct stenting. Eur Heart J. 2003;24:394–403.
Loubeyre C, Morice MC, Lefèvre T, Piéchaud JF, Louvard Y, Dumas P. A randomized comparison of direct stenting with conventional stent implantation in selected patients with acute myocardial infarction. J Am Coll Cardiol. 2002;39(1):15–21.
Ozdemir R, Sezgin AT, Barutcu I, Topal E, Gullu H, Acikgoz N. Comparison of direct stenting versus conventioncal stent implantation on blood flow in patients with ST-segment elevation myocardial infarction. Angiology. 2006;57(4):453–8.
Mahmoud KD, Jolly SS, James S, Džavík V, Cairns JA, Olivecrona GK, et al. Clinical impact of direct stenting and interaction with thrombus aspiration in patients with ST-segment elevation myocardial infarction undergoing percutaneous coronary intervention: Thrombectomy Trialists Collaboration. Eur Heart J. 2018;39(26):2472–9.
Neumann FJ, Gick M. Direct stenting in ST-elevation myocardials infarction: convenient, but not improving outcomes. Eur Heart J. 2018;39(26):2480–3.
Gick M, Jander N, Bestehorn HP, Kienzle RP, Ferenc M, Werner K, et al. Short- and long-term effects of ischemic postconditioning in STEMI patients: a meta-analysis. Lipids Health Dis. 2015;14(1):147.
Høfsten DE, Kelbæk H, Helqvist S, Kløvgaard L, Holmvang L, Clemmensen P, et al. The third Danish study of optimal acute treatment of patients with ST-segment elevation myocardial infarction: ischemia postconditioning or deferred stent implantation versus conventional primary angioplasty and complete revascularization versus treatment of culprit lesion only: rationale and design of the DANAMI 3 trial program. Am Heart J. 2015;169(5):613–21.
Kim EK, Hahn JY, Song YB, Lee SC, Choi JH, Choi SH, et al. Effect of ischemic postconditioning on myocardial salvage in patients undergoing primary percutaneous coronary intervention for ST-segment elevation myocardial infarction: cardiac magnetic resonance substudy of the POST randomized trial. Int J Cardiovasc Imaging. 2015;31(3):629–37.
Rezkalla SH, Kloner RA. Coronary no-reflow phenomenon: from the experimental laboratory to the cardiac catheterization laboratory. Catheter Cardiovasc Interv. 2008;72(7):950–7.
Reffelmann T, Hale SL, Dow JS, Kloner RA. No-reflow phenomenon persists long-term after ischemia/reperfusion in the rat and predicts infarct expansion. Circulation. 2003;108(23):2911–7.
Valgimigli M, Gragnano F, Branca M, Franzone A, Baber U, Jang Y, et al. P2Y12 inhibitor monotherapy or dual antiplatelet therapy after coronary revascularisation:individual patient level meta-analysis of randomised controlled trials. BMJ. 2021;373:n1332.
Acknowledgements
We would like to thank the patients who participated in the study and the staff from Departments of Cardiology and Radiology.
Funding
This work was supported by the Applied and fundamental study of Sichuan Province (No. 2017JY0026), the Fellowship of China Postdoctoral Science Foundation (No. 2020M683325), the Post-Doctor Research Project, West China Hospital, Sichuan University (No. 2020HXBH048), 1.3.5 project for disciplines of excellence Clinical Research Incubation Project, West China Hospital,Sichuan University (No. 2021HXFH021), and the Innovative scientific research project of medical youth in Sichuan Province (No. Q20061). Specifically, the funding was used to image data analysis, purchase of consume material in present study, publication costs, and instrument use costs, etc. Also, the stipend of graduate students comes from the funding.
Author information
Authors and Affiliations
Contributions
YH conceived of the study, and participated in its design. MM and LW coordination, drafted the manuscript, collect data and algorithms. KYD and SCL are take responsibility of the imaging data analysis. YZ, HW, MW, and LZ are senior experienced cardiologists. They are responsible for including patients and excluding patients, patients’ surgery and coronary imaging data analysis. ZGY is experienced and senior radiology specialist and responsibility for the selection of study, extraction of data, and assessment of study quality independently. YH and ZGY are the study guarantors, had full access to the data in the study and take responsibility of the study design and the accuracy of the data analysis, and had the final responsibility to submit for publication. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study complied with the Declaration of Helsinki and was approved by the Institutional Ethics Committee of West China Hospital, Sichuan University, Chengdu, Sichuan, China (Ethical approval No. 2016 (337)). Written informed consents were obtained from all the study participants.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ma, M., Wang, L., Diao, Ky. et al. A randomized controlled clinical trial of prolonged balloon inflation during stent deployment strategy in primary percutaneous coronary intervention for ST-segment elevation myocardial infarction: a pilot study. BMC Cardiovasc Disord 22, 30 (2022). https://doi.org/10.1186/s12872-022-02477-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-022-02477-0