Abstract
This systematic review aims to assess the effect of mindfulness-based interventions carried out during pregnancy exploring mindfulness and mental health outcomes. A systematic review was conducted to appraise the current literature on the subject area. Inclusion and exclusion criteria were agreed and after reviewing titles, abstracts and full papers, 14 articles met the inclusion criteria and were included in the review. The quality of included articles was checked using the Quality Assessment Tool for Quantitative Studies. Pooled results of the randomised controlled trials (RCTs) reporting outcomes on anxiety, depression and perceived stress indicated no differences between the mindfulness intervention group and the control group. Pooled results of the non-RCTs reporting anxiety, depression and perceived stress showed a significant benefit for the mindfulness group. Mindfulness as an outcome was assessed in four RCTs for which the pooled results show a significant difference in favour of the mindfulness intervention when compared to a control group. The pooled results of the four non-RCTs also indicate a significant difference following mindfulness intervention. Results suggest that mindfulness-based interventions can be beneficial for outcomes such as anxiety, depression, perceived stress and levels of mindfulness during the perinatal period. Further research would be useful to explore if such benefits are sustained during the post-natal period.
Similar content being viewed by others
Introduction
Pregnancy and childbirth are some of the most significant, exciting and scary experiences that a woman will experience in her lifetime. The experiences and mental health of the woman during pregnancy and throughout the post-pregnancy period are of utmost importance for the well-being of both the mother and her child. Depression or anxiety in pregnancy has been associated with an increase in obstetric complications including stillbirth, low birth weight infants, postnatal specialist care for the infant and susceptibility to more adverse neurodevelopmental outcomes including behavioural, emotional and cognitive problems (Bonari et al. 2004; Glover 2011; Talge et al. 2007). Anxiety and stress during pregnancy have been linked with premature delivery, low birth weight, and neonatal morbidity and mortality (Dole 2003; Maina et al. 2008).
While some women welcome the challenges of childbirth, others may feel a significant amount of anxiety and concern (Escott et al. 2004; Huizink et al. 2004). Anxiety and stress in pregnancy have been found to be associated with gestational length, with increases in stress and anxiety leading to preterm delivery and declines in stress and anxiety resulting in delivery at term (Glynn et al. 2008; Schetter and Tanner 2012). Preterm birth has adverse implications for foetal neurodevelopment and child outcomes and is the leading cause of infant mortality and morbidity (Schetter and Tanner 2012; Wadhwa et al. 2011). The management of anxiety in pregnant women is therefore of importance to prevent poor outcomes for both the mother and child.
Evidence suggests that up to 20% of women are affected by depression during pregnancy, and during the post-partum period, which indicates a need to support women from pregnancy to post-partum (Evans et al. 2001; Liberto 2012; Rich-Edwards et al. 2006). Untreated maternal depression can lead to illness persistence and an increase in symptom severity (Robertson et al. 2003).
Pregnancy is a key time to be caring for the mothers’ mind and mental attitude (Donegan 2015). One way in which this can be supported is through mindfulness, known to promote emotional positivity and stability. Kabat-Zinn (1994) described mindfulness as “paying attention in a particular way: on purpose, in the present moment, and nonjudgmentally” (p. 4). The process of accepting things as they are and approaching situations with an open mind reduces tension and fear and increases trust. Mindfulness can offer support to a mother both during the perinatal period and beyond (Cohen 2010; Fisher et al. 2012). Mindfulness-based interventions show promise in addressing a number of adverse outcomes, such as antenatal depression and anxiety, providing pregnant women with more empowerment and satisfaction with labour (Fisher et al. 2012). While planning for birth can be a positive experience and has its advantages, this should be flexible because if a birth plan does not come together, it could cause distress and strain on the body (Sparkes 2015). It is therefore important to focus on moment-to-moment changes, allowing some trust in the body.
Mindfulness-based interventions allow the development of abilities that are important for pregnant women and new mothers (Hall et al. 2015). These interventions encourage practice of awareness and acceptance of one’s thoughts, emotions and body sensations, building stress tolerance, reducing reactivity and avoidance of uncomfortable experiences. The seven-attitudinal factors covered in mindfulness-based interventions include non-judging, patience, beginner’s mind, trust, non-striving, acceptance and letting go (Kabat-Zinn 1990).
Pregnant women may require support through their pregnancies with mindfulness-based interventions having been suggested as potentially beneficial to support these women. The aim of this systematic review is therefore to appraise the current available literature and assess the effect of mindfulness-based interventions carried out during pregnancy in mindfulness levels and mental health-related outcomes (i.e. anxiety, stress and depression).
Method
The systematic review protocol was registered with PROSPERO: CRD42016032627.
Search Strategy
A search was conducted to review the current literature on mindfulness-based interventions carried out during pregnancy. A search strategy was developed using a combination of both indexing and free text terms (see Supplementary Material 1 for sample search strategy). Electronic databases including the Cochrane Library (Wiley) (including CDSR, DARE, HTA and CENTRAL), MEDLINE (Ovid), MEDLINE in Process (Ovid), EMBASE (Ovid), Science Citation Index (Web of Science) and Conference Proceedings Citation Index (Web of Science) were initially searched from their inception to 11 February 2016, with no restriction on language, and updated up to 20 February 2017. Hand searching of reference lists of relevant studies and reviews was carried out. Literature search results were uploaded to and managed using Mendeley Desktop 1.16.1 software.
Study Selection
Two reviewers (AD, RD) independently screened the titles and abstracts of all retrieved citations. The following inclusion and exclusion criteria were applied to the citations identified by the literature search. Inclusion criteria were as follows: (i) pregnant females; (ii) mindfulness-based interventions (i.e. practices that incorporated the use of mindfulness including mindfulness-based yoga, mindfulness-based cognitive therapy, mindfulness-based stress reduction, acceptance and commitment therapy); (iii) comparative study design including randomised controlled trials (RCTs) and pre-post intervention studies and (iv) report of mental health-related outcomes (i.e. anxiety, stress, depression, levels of mindfulness). Exclusion criteria were as follows: (i) reviews or guidance papers that do not present original work; (ii) case reports; (iii) not including pregnant females or (iv) not mindfulness-based interventions. Where inclusion or exclusion could not be determined from the abstracts, full papers were retrieved. Full papers for studies deemed potentially relevant by the screening were retrieved. Disagreements were resolved through discussion and consensus between the reviewers; if consensus was not reached, a third reviewer (ES) was consulted.
Quality Assessment
The quality of included articles was checked using the Quality Assessment Tool for Quantitative Studies (Effective Public Health Practice Project 1998). This tool, recommended by Cochrane, covers any quantitative study design and assists reviewers to score study quality. The tool evaluates aspects such as confounding, where reviewers indicate whether confounders were controlled for in the design (i.e. if participants receive an unintended intervention that may have influenced the outcomes) and intervention integrity (i.e. whether the method of measuring the intervention is the same for all participants). The tool has been judged to be suitable to use in systematic reviews of effectiveness (Deeks et al. 2003). Two reviewers conducted the assessment independently. Disagreement were resolved by discussion and consensus and if necessary consultation of a third reviewer.
Data Extraction
For each included study, the data was extracted by one reviewer (AD) and checked for accuracy by a second reviewer (RD). Disagreements were resolved by discussion and if necessary consultation of a third reviewer. The data extracted included (1) general information including study ID, author, year, journal, study design and setting; (2) recruitment details, sample size, demographic characteristics (age, gender) and baseline health data; (3) nature of intervention, treatment duration, follow-up and (4) outcome measures. Where necessary and if possible, study authors were contacted for missing data by email. In case of no response, the authors were contacted at least twice over a 2-week period by email.
Data Analyses
A narrative synthesis was included as the review obtained information from a diverse body of evidence. Statistical pooling of the results was carried out using RevMan 5.2. For continuous variables, the use of the mean difference (MD) or standardised mean difference (SMD) in the analysis was determined by whether studies all report the outcome using the same scale (MD) or using different scales (SMD). A random effects model was used for the meta-analyses. For non-randomised controlled trials, meta-analyses of adjusted estimates were performed as an inverse-variance weighted average.
Results
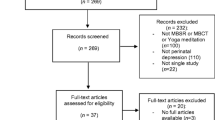
The search resulted in 469 abstracts screened and 26 papers identified as potentially relevant (Fig. 1). After reading the full-text, 12 articles were excluded for the following reasons: review articles (Arendt and Tessmer-Tuck 2013; Field 2008; Khianman et al. 2012; Marc et al. 2011; Smith et al. 2011), no original research presented (Beattie et al. 2014; Beddoe and Lee 2008; Donegan 2015), no mindfulness intervention (Curtis et al. 2012; Kim et al. 2008; Koyyalamudi et al. 2016), includes women at pre-conception, pregnant and postpartum stage and results are not presented separately (Miklowitz et al. 2015). Fourteen articles were found to meet the inclusion criteria. One of the articles included (Woolhouse et al. 2014) presented two studies, a one-group cohort study and a pilot RCT.
Characteristics of included studies are listed in Table 1. Prenatal or obstetric clinics and hospitals were the main source of participant recruitment. The duration of the mindfulness-based interventions varied from 6 to 9 weeks (Table 2). All of the studies carried out assessments at baseline and post-intervention. Some studies also collected post-partum data; however, the timings of post-partum assessment were variable between the studies ranging from 4 weeks to 6 months, therefore limiting the interpretation of the results. For that reason, post-partum data was not included in the meta-analyses. A number of patient reported outcome measures were used across the studies with the following measures being more commonly used in this population: Mindfulness Attention Awareness Scale (MAAS), State-Trait anxiety Inventory (STAI), Depression, Anxiety Stress Scales (DASS-21), Edinburgh postpartum Depression Scale (EPDS) and the Perceived Stress Scale (PSS). The overall global rating for quality using the using the Quality Assessment Tool for Quantitative Studies detailed in Supplementary Material 2 was moderate (n = 1) or weak (n = 14).
Three RCTs reported outcomes on anxiety (Guardino et al. 2014; Vieten and Astin 2008; Woolhouse et al. 2014). The pooled results indicated no differences between the mindfulness intervention group and the control group (−0.31, 95% CI −1.11 to 0.49, p = 0.45) (Fig. 2). Pooled results of six non-RCTs reporting anxiety (one study investigating two trimesters with different patients) showed a significant benefit for the mindfulness group (−0.48, 95% CI −0.86 to −0.10, p = 0.01).
The pooled results of RCTs evaluating depression indicated no difference between the mindfulness intervention group and the control group (−0.78, 95% CI −1.58 to 0.01, p = 0.05) (Fig. 3). Pooled results of the non-RCTs assessing depression suggested, however, a significant difference favouring mindfulness intervention (−0.59, 95% CI −0.93 to −0.26, p = 0.0005).
Perceived stress was assessed in six RCTs with pooled results demonstrating no significant differences between the mindfulness and the control group (−1.23, 95% CI −2.58 to 0.12, p = 0.07) (Fig. 4). The pooled results of four non-RCTs evaluating perceived stress showed a significant difference following mindfulness intervention (−3.28, 95% CI −5.66 to −0.89, p = 0.007).
Mindfulness as an outcome was assessed in four RCTs for which the pooled results showed a significant difference in favour of mindfulness intervention when compared to a control group (−0.57, 95% CI −0.92 to −0.22, p = 0.002) (Fig. 5). Consistently with this observed effect, the pooled results of the four non-RCTs also indicated a significant difference following mindfulness intervention (−0.60, 95% CI −0.93 to −0.27, p = 0.0004).
Discussion
The pooled results of RCTs included in this systematic review, although suggesting a trend in favour of mindfulness interventions, did not produce statistically significant results when assessing changes in anxiety, depression and perceived stress. This may be due to the limited number of RCTs and the small numbers of participants included in these RCTs. Furthermore, the RCTs available were either pilot or feasibility studies, or not adequately powered to demonstrate the effectiveness of a mindfulness-based intervention. The results of the pooled analysis of non-RCTs, although indicating statistically significant benefits, should be interpreted with caution as the analysis was based on studies with higher risk of bias, poor design and prone to confounding. Consistent results in the pooled analysis between RCTs and non-RCTs were observed for mindfulness, therefore demonstrating an increase in awareness following a mindfulness-based intervention. The ensuing paragraphs discuss in further detail the results observed in this review in terms of the effect of mindfulness-based interventions carried out during pregnancy in the mental health-related outcomes assessed (i.e. anxiety, stress and depression) and mindfulness levels.
Previous evidence has found support for mindfulness when used to reduce anxiety and depression. A meta-analysis demonstrated that mindfulness-based therapy is a promising intervention for treating anxiety and mood problems in clinical populations (Hofmann et al. 2010). Additionally, a systematic review and meta-analysis of RCTs evaluating the effect of mindfulness-based therapy on symptoms of anxiety and depression in adult cancer patients and survivors found that mindfulness-based therapy was associated with significantly reduced symptoms of anxiety and depression from pre- to post-treatment (Piet et al. 2012). These studies demonstrate the beneficial use of mindfulness-based interventions to reduce anxiety and depression in clinical populations. As highlighted above, our pooled analysis of the RCT data suggested some benefit of using mindfulness-based interventions to reduce anxiety and depression in pregnant women. Although the results were not statistically significant and were based on either pilot, feasibility or underpowered RCTs, they do suggest that there is a need for more robust, controlled research in this area.
To further our understanding of perceived stress and the use of mindfulness in pregnancy, suggestions from other research should also be explored. According to Beddoe et al. (2009), a factor to be considered is that the differences in perceived stress between women in the second and third trimester could be due to normal changes resulting from pregnancy. Roth and Robbins (2004) have suggested that mindfulness does not only have a positive effect on stress reduction in specific populations, such as maternal health and pain, but can be beneficial for healthy individuals, emphasising mindfulness as a promising intervention to improve stress levels. Furthermore, mindfulness-based stress reduction was found to reduce ruminative thinking and trait anxiety, as well as to increase empathy and self-compassion, suggesting that mindfulness-based interventions are also able to reduce stress levels in healthy people (Chiesa and Serretti 2009). These studies support the notion that mindfulness may improve perceived stress not only in clinical populations but also in healthy individuals. However, Guardino et al. (2014) suggested that mindfulness training alone may not be sufficient to consistently reduce levels of perceived stress during pregnancy. It may therefore be of relevance to explore if mindfulness in combination with additional support/interventions may contribute to a more consistent reduction in perceived stress during pregnancy.
Levels of mindfulness were found to increase in pregnant women participating in a mindfulness intervention group and also to increase as pregnant women progressed through the intervention. Mindfulness practice has been hypothesised to develop the capacity to observe the changing mental and physiological states and sensations without necessarily trying to change them (Beattie et al. 2014). In a population with pregnant women, the individual will be more likely to accept what is happening and make clearer decisions about their response. Mindfulness benefits may include improvement in health outcomes for women and their families (Beattie et al. 2014).
This review has a number of limitations which must be considered when interpreting the results. There was considerable heterogeneity in the pooled analyses of the RCTs. The authors of two studies were contacted for additional data to include in the meta-analysis; however, no response was obtained. The results from the control groups of the RCTs may have been confounded; in the Guardino et al. (2014) study, 30% of the control group took a prenatal yoga class during their pregnancies, which could have resulted in a reduction on anxiety levels of the control group. Furthermore, the reading materials given to the control group may have also decreased their anxiety indirectly, by individuals gaining more knowledge about their pregnancy. This could suggest that people may improve on their own and not as a result of an intervention. It has been observed that participants in control conditions are often motivated to make their own improvements (McBride 2015). Additionally, Kinser and Robins (2013) found that control group participants ended up making more significant changes than was expected, due to discussions between the groups, social support and participating in other activities which promoted positive behaviour changes. Therefore, it would be useful for future research to explore mediational analyses to further understand this area.
In conclusion, the present systematic review suggests that mindfulness-based interventions may be beneficial for outcomes such as anxiety, depression, perceived stress and levels of mindfulness. However, there is a lack of evidence in this area. Further research including adequately powered RCTs is warranted to confirm the effectiveness of mindfulness in pregnant women. It would be of value to explore if benefits reported by pregnant women following a mindfulness-based intervention are of benefit during the post-natal period and to their offspring. If future evidence demonstrates that mindfulness-based programmes are effective, by recommending these interventions, health care professionals can help pregnant women to manage a number of pregnancy-related factors associated with the expectations and uncertainties of becoming a mother.
References
Arendt, K., & Tessmer-Tuck, J. (2013). Nonpharmacologic labor analgesia. Clinics in Perinatology, 40(3), 351–371.
Beattie, J., Hall, H., Biro, M., & East, C. (2014). Does mindfulness training reduce the stress of pregnancy? Australian Nursing & Midwifery Journal, 22(1), 39.
Beddoe, A., & Lee, K. (2008). Mind-body interventions during pregnancy. Journal of Obstetric, Gynecologic & Neonatal Nursing, 37(2), 165–175.
Beddoe, A. E., Paul Yang, C. P., Kennedy, H. P., Weiss, S. J., & Lee, K. A. (2009). The effects of mindfulness-based yoga during pregnancy on maternal psychological and physical distress. Journal of Obstetric, Gynecologic & Neonatal Nursing, 38(3), 310–319.
Bonari, L., Pinto, N., Ahn, E., Einarson, A., Steiner, M., & Koren, G. (2004). Perinatal risks of untreated depression during pregnancy. Canadian Journal of Psychiatry, 49(11), 726–735.
Bowen, A., Baetz, M., Schwartz, L., Balbuena, L., & Muhajarine, N. (2014). Antenatal group therapy improves worry and depression symptoms. The Israel Journal of Psychiatry and Related Sciences, 51(3), 226–231.
Byrne, J., Hauck, Y., Fisher, C., Bayes, S., & Schutze, R. (2014). Effectiveness of a mindfulness-based childbirth education pilot study on maternal self-efficacy and fear of childbirth. Journal of Midwifery & Women’s Health, 59(2), 192–197.
Chiesa, A., & Serretti, A. (2009). Mindfulness-based stress reduction for stress management in healthy people: a review and meta-analysis. The Journal of Alternative and Complementary Medicine, 15(5), 593–600.
Cohen, J. S. (2010). Mindfulness and self-compassion in the transition to motherhood: a prospective study of postnatal mood and attachment. New York: Columbia University.
Curtis, K., Weinrib, A., & Katz, J. (2012). Systematic review of yoga for pregnant women: current status and future directions. Evidence-based Complementary and Alternative Medicine, 2012, 1–13.
Deeks, J. J., Dinnes, J., D'Amico, R., Sowden, A. J., Sakarovitch, C., Song, F., Petticrew, M., Altman, D. G., & International Stroke Trial Collaborative Group; European Carotid Surgery Trial Collaborative Group. (2003). Evaluating non-randomised intervention studies. Health Technology Assessment, 7(27), 1–173.
Dimidjian, S., Goodman, S. H., Felder, J. N., Gallop, R., Brown, A. P., & Beck, A. (2015). An open trial of mindfulness-based cognitive therapy for the prevention of perinatal depressive relapse/recurrence. Archives of Women's Mental Health, 18(1), 85–94.
Dimidjian, S., Goodman, S. H., Felder, J. N., Gallop, R., Brown, A. P., & Beck, A. (2016). Staying well during pregnancy and the postpartum: a pilot randomized trial of mindfulness-based cognitive therapy for the prevention of depressive relapse/recurrence. Journal of Consulting and Clinical Psychology, 84(2), 134–145.
Dole, N. (2003). Maternal stress and preterm birth. American Journal of Epidemiology, 157(1), 14–24.
Donegan, T. (2015). Mindfulness: an intervention for improving the health of mothers and babies. Midwifery Today, 113, 62–63.
Duncan, L. G., & Bardacke, N. (2010). Mindfulness-based childbirth and parenting education: promoting family mindfulness during the perinatal period. Journal of Child and Family Studies, 19(2), 190–202.
Dunn, C., Hanieh, E., Roberts, R., & Powrie, R. (2012). Mindful pregnancy and childbirth: effects of a mindfulness-based intervention on women’s psychological distress and well-being in the perinatal period. Archives of Women's Mental Health, 15(2), 139–143.
Effective Public Health Practice Project. (1998). Quality assessment tool for quantitative studies. http://www.ephpp.ca/index.html. Accessed 7 March 2016.
Escott, D., Spiby, H., Slade, P., & Fraser, R. (2004). The range of coping strategies women use to manage pain and anxiety prior to and during first experience of labour. Midwifery, 20(2), 144–156.
Evans, J., Heron, J., Francomb, H., Oke, S., & Golding, J. (2001). Cohort study of depressed mood during pregnancy and after childbirth. BMJ, 323(7307), 257–260.
Field, T. (2008). Pregnancy and labor alternative therapy research. Alternative Therapies in Health and Medicine, 14(5), 28–34.
Fisher, C., Hauck, Y., Bayes, S., & Byrne, J. (2012). Participant experiences of mindfulness-based childbirth education: a qualitative study. BMC Pregnancy and Childbirth, 12(1), 126.
Glover, V. (2011). Annual research review: prenatal stress and the origins of psychopathology: an evolutionary perspective. Journal of Child Psychology and Psychiatry, 52(4), 356–367.
Glynn, L., Schetter, C., Hobel, C., & Sandman, C. (2008). Pattern of perceived stress and anxiety in pregnancy predicts preterm birth. Health Psychology, 27(1), 43–51.
Goodman, J. H., Guarino, A., Chenausky, K., Klein, L., Prager, J., Petersen, R., Forget, A., & Freeman, M. (2014). CALM pregnancy: results of a pilot study of mindfulness-based cognitive therapy for perinatal anxiety. Archives of Women's Mental Health, 17(5), 373–387.
Guardino, C. M., Dunkel Schetter, C., Bower, J. E., Lu, M. C., & Smalley, S. L. (2014). Randomised controlled pilot trial of mindfulness training for stress reduction during pregnancy. Psychology & Health, 29(3), 334–349.
Hall, H., Beattie, J., Lau, R., East, C., & Biro, M. (2015). The effectiveness of mindfulness training on perinatal mental health; a systematic review. Women and Birth, 29(1), 62–71.
Hofmann, S., Sawyer, A., Witt, A., & Oh, D. (2010). The effect of mindfulness-based therapy on anxiety and depression: a meta-analytic review. Journal of Consulting and Clinical Psychology, 78(2), 169–183.
Huizink, A. C., Mulder, E. J., Robles de Medina, P. G., Visser, G. H., & Buitelaar, J. K. (2004). Is pregnancy anxiety a distinctive syndrome? Early Human Development, 79(2), 81–91.
Iyengar, B. K. S. (1979). Light on yoga. New York: Schocken Books.
Kabat-Zinn, J. (1990). Full catastrophe living: using the wisdom of your body and mind to face stress, pain, and illness. New York: Dellacourt.
Kabat-Zinn, J. (1994). Wherever you go, there you are. London: Piatkus.
Khianman, B., Pattanittum, P., Thinkhamrop, J., & Lumbiganon, P. (2012). Relaxation therapy for preventing and treating preterm labour. Cochrane Database of Systematic Reviews, 8, CD007426.
Kim, H. H., Nava-Ocampo, A. A., Kim, S. K., Kim, S. H., Kim, Y. J., Han, J. Y., Ahn, H. K., Ryu, H. M., Yang, J. H., & Kim, M. Y. (2008). Is prenatal childbirth preparation effective in decreasing adverse maternal and neonatal response to labor? A nested case-control study. Acta Biomedica de l'Ateneo Parmense, 79(1), 18–22.
Kinser, P., & Robins, J. (2013). Control group design: enhancing rigor in research of mind-body therapies for depression. Evidence-based Complementary and Alternative Medicine, 2013, 1–10.
Koyyalamudi, V., Sidhu, G., Cornett, E., Nguyen, V., Labrie-Brown, C., Fox, C., & Kaye, A. (2016). New labor pain treatment options. Current Pain and Headache Reports, 20(2), 11.
Liberto, T. L. (2012). Screening for depression and help-seeking in postpartum women during well-baby pediatric visits: an integrated review. Journal of Pediatric Health Care, 26(2), 109–117.
Maina, G., Saracco, P., Giolito, M. R., Danelon, D., Bogetto, F., & Todros, T. (2008). Impact of maternal psychological distress on fetal weight, prematurity and intrauterine growth retardation. Journal of Affective Disorders, 111(2–3), 214–220.
Marc, L., Toureche, N., Hodnett, E., Blanchet, C., Dodin, S., & Njoya, M. (2011). Mind-body interventions during pregnancy for preventing or treating women’s anxiety. Cochrane Database of Systematic Reviews, 7, CD007559.
Matvienko-Sikar, K., & Dockray, S. (2016). Effects of a novel positive psychological intervention on prenatal stress and well-being: a pilot randomised controlled trial. Women and Birth. doi:10.1016/j.wombi.2016.10.003.
McBride, D. (2015). The process of research in psychology. Los Angeles: SAGE.
Miklowitz, D., Semple, R., Hauser, M., Elkun, D., Weintraub, M., & Dimidjian, S. (2015). Mindfulness-based cognitive therapy for perinatal women with depression or bipolar spectrum disorder. Cognitive Therapy and Research, 39(5), 590–600.
Muthukrishnan, S., Jain, R., Kohli, S., & Batra, S. (2016). Effect of mindfulness meditation on perceived stress scores and autonomic function tests of pregnant Indian women. Journal of Clinical and Diagnostic Research, 10(4), 5–8.
Piet, J., Würtzen, H., & Zachariae, R. (2012). The effect of mindfulness-based therapy on symptoms of anxiety and depression in adult cancer patients and survivors: a systematic review and meta-analysis. Journal of Consulting and Clinical Psychology, 80(6), 1007–1020.
Rich-Edwards, J. W., Kleinman, K., Abrams, A., Harlow, B. L., McLaughlin, T. J., Joffe, H., & Gillman, M. W. (2006). Sociodemographic predictors of antenatal and postpartum depressive symptoms among women in a medical group practice. Journal of Epidemiology and Community Health, 60(3), 221–227.
Robertson, E., Celasun, N., & Stewart, D. E. (2003). Risk factors for postpartum depression. In D. E. Stewart, E. Robertson, C. L. Dennis, S. L. Grace, & T. Wallington (Eds.), Postpartum depression: literature review of risk factors and interventions (pp. 9–70). Toronto: Toronto Public Health.
Roth, B., & Robbins, D. (2004). Mindfulness-based stress reduction and health-related quality of life: findings from a bilingual inner-city patient population. Psychosomatic Medicine, 66(1), 113–123.
Schetter, C. D., & Tanner, L. (2012). Anxiety, depression and stress in pregnancy: implications for mothers, children, research, and practice. Current Opinion in Psychiatry, 25(2), 141–148.
Shahtaheri, E., Hosseinian, S., Ebrahimi, M., Jalilabadi, Z., & Mirderikvand, F. (2016). The impact of stress reduction program based on mindfulness and conscious yoga on depression, perceived stress and quality of life in pregnant women. Acta Medica Mediterranea, 32(5), 2047–2050.
Smith, C. A., Levett, K. M., Collins, C. T., & Crowther, C. (2011). Relaxation techniques for pain management in labour. Cochrane Database of Systematic Reviews, 12, CD009514.
Sparkes, E. (2015). The birth plan? Really? The Huffington Post. http://www.huffingtonpost.co.uk/dr-elizabeth-sparkes/the-birth-plan-really_b_8070282.html. Accessed 9 May 2016.
Talge, N. M., Neal, C., & Glover, V. (2007). Antenatal maternal stress and long-term effects on child neurodevelopment: how and why? Journal of Child Psychology and Psychiatry, 48(3–4), 245–261.
Vieten, C., & Astin, J. (2008). Effects of a mindfulness-based intervention during pregnancy on prenatal stress and mood: results of a pilot study. Archives of Women's Mental Health, 11(1), 67–74.
Wadhwa, P. D., Entringer, S., Buss, C., & Lu, M. C. (2011). The contribution of maternal stress to preterm birth: issues and considerations. Clinics in Perinatology, 38(3), 351–384.
Woolhouse, H., Mercuri, K., Judd, F., & Brown, S. J. (2014). Antenatal mindfulness intervention to reduce depression, anxiety and stress: a pilot randomised controlled trial of the MindBabyBody program in an Australian tertiary maternity hospital. BMC Pregnancy and Childbirth, 14, 369.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
None of the authors had any direct or indirect funding in support of this study.
Ethical Approval
This article does not contain any studies with human participants performed by any of the authors.
Conflict of Interest
The authors declare that they have no conflicts of interest.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Dhillon, A., Sparkes, E. & Duarte, R.V. Mindfulness-Based Interventions During Pregnancy: a Systematic Review and Meta-analysis. Mindfulness 8, 1421–1437 (2017). https://doi.org/10.1007/s12671-017-0726-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12671-017-0726-x