Abstract
Purpose
Simulation is an important alternative to evaluate cricothyrotomy, a rare life-saving procedure. This crossover study aimed to determine whether contextualization of a crisis scenario would impact the performance of a cricothyrotomy procedural task.
Methods
Sixty-five anesthesia assistants and emergency medicine and anesthesia residents underwent a teaching session in surgical cricothyrotomy using one of two sets of cricothyrotomy kits: the Portex 6.0 and Melker 3.5 (n = 32) or the Portex 6.0 and Melker 5.0 (n = 33). Within six weeks following the session, the participants performed cricothyrotomies on a full-body patient mannequin simulator coupled with a porcine larynx (tissue-mannequin simulator) using the assigned two kits in a “cannot intubate, cannot ventilate” (CICV) contextualized scenario (CS) and in a CICV verbalized non-contextualized scenario (NCS). Each participant performed a total of four cricothyrotomies using the two kits in the two scenarios. The primary outcome measure was insertion time, and secondary outcome measures were severity of injuries and failure rate. Outcome measures were compared between scenarios for each kit.
Results
Mean (SD) insertion time for a successful cricothyrotomy was not significantly different between NCS and CS for the Melker 3.5 [83.0 (45.0) sec vs 63.3 (36.1) sec, respectively; P = 0.96; mean difference (MD), 19.7 sec; 95% confidence interval (CI), −1.9 to 41.3], the Melker 5.0 [86.5 (36.8) sec vs 107.1 (55.6) sec, respectively; P = 0.11; MD, −20.6 sec; 95% CI, −44.9 to 3.7], and the Portex 6.0 [59.5 (35.5) sec vs 59.0 (35.0) sec, respectively; P = 0.95; MD, 0.5 sec; 95% CI, −13.2 to 14.2]. Failure rate and severity of injuries, measured as mean average injury score for each kit, were also similar between scenarios.
Conclusions
Contextualization of a crisis scenario did not affect the performance of a cricothyrotomy procedural task on a tissue-mannequin simulator. These findings may have implications when considering the feasibility and cost-effectiveness for assessing the performance of cricothyrotomy procedural tasks.
Résumé
Objectif
La simulation est une alternative importante pour évaluer la cricothyrotomie, une intervention de sauvetage rare. Cette étude croisée avait pour objectif de déterminer si la mise en contexte d’un scénario de crise avait un impact sur la performance d’une tâche procédurale de cricothyrotomie.
Méthode
Soixante-cinq assistants en anesthésie et résidents en médecine d’urgence et en anesthésie ont suivi une séance d’enseignement en cricothyrotomie chirurgicale avec l’une de deux trousses de cricothyrotomie: la trousse Portex 6,0 et Melker 3,5 (n = 32) ou la trousse Portex 6,0 et Melker 5,0 (n = 33). Au cours des six semaines suivant le cours, les participants ont réalisé des cricothyrotomies sur un mannequin de simulation de corps humain complet doté d’un larynx porcin (le mannequin de simulation en tissu) à l’aide des deux trousses, dans un scénario contextualisé (SC) de « impossible d’intuber, impossible de ventiler » et dans un scénario non contextualisé (SNC) mais où le « impossible d’intuber, impossible de ventiler » avait été verbalisé. Chaque participant a réalisé quatre cricothyrotomies au total, à l’aide des deux trousses dans les deux scénarios. Le critère d’évaluation principal était le temps d’insertion, et les critères secondaires étaient le taux d’échec et la gravité des lésions au larynx. Les résultats ont été comparés entre les scénarios pour chacune des trousses.
Résultats
Aucune différence significative en matière de temps d’insertion moyen (ÉT) pour une cricothyrotomie réussie n’a été observée entre le SC et le SNC pour la trousse Melker 3,5 [83,0 (45,0) sec vs 63,3 (36,1) sec, respectivement; P = 0,96; différence moyenne (DM), 19,7 sec; intervalle de confiance (IC) 95 %, -1,9 à 41,3], la trousse Melker 5,0 [86,5 (36,8) sec vs 107,1 (55,6) sec, respectivement; P = 0,11; DM, -20,6 sec; IC 95 %, -44,9 à 3,7], et la trousse Portex 6,0 [59,5 (35,5) sec vs 59,0 (35,0) sec, respectivement; P = 0,95; DM, 0,5 sec; IC 95 %, -13,2 à 14,2]. Les taux d’échec et la gravité des lésions au larynx, mesurée en tant que score moyen de lésion pour chaque trousse, étaient également semblables pour les deux scénarios.
Conclusion
La mise en contexte d’un scénario de crise n’a pas affecté la réalisation d’une tâche procédurale de cricothyrotomie sur un mannequin de simulation. Ces résultats pourraient avoir un impact lorsqu’on étudie la faisabilité et la rentabilité d’une évaluation de la performance de tâches procédurales de cricothyrotomie.
Similar content being viewed by others
Performing practical procedures is essential in many acute care specialties, including anesthesia, emergency medicine, and critical care. Although many procedures can be performed and assessed on patients, in the case of a rare emergency life-saving procedure, such as a cricothyrotomy,1 it is impractical and unethical to assess such a procedure on patients. Suboptimal performance of high-stakes procedures can lead to brain hypoxia or death, as in the clinical cases of a poorly performed or failed cricothyrotomy.2 It is therefore imperative to assess life-saving procedures to ensure they are properly performed.
Traditionally, medical procedures have been assessed on patients. Over the years, however, simulation has become an important education adjunct for evaluation of procedural tasks.3 Simulation can be broadly defined as any system that replicates a real-life system. Advances in simulation technology have enabled the assessment of procedures in the simulation laboratory without causing potential harm to patients. A full-body patient computerized mannequin can provide physiological feedback similar to patient feedback in a real-life situation,4 and it can facilitate recreating crisis situations where life-saving procedures must be performed quickly to prevent further physiological compromise.5
For rarely performed procedures, such as a cricothyrotomy, simulation is the only alternative for assessment. It has been proposed that, to be effective, such simulation must be realistic and grounded in an authentic clinical context that recreates key components of the clinical experience.6 Much of the research on contextualized simulation has focused on performing procedural tasks in a non-crisis situation, for example, the performance of an intravenous insertion on a mannequin arm that is integrated with an actor patient.3,6,7 Nevertheless, little is known on the degree of realism needed to assess rare life-saving procedures that must be performed quickly and safely. Such knowledge is important since it is presumed that performance in a contextualized simulation closely reflects performance in a clinical situation.6,7
The degree of realism in simulation is generally referred to as fidelity. Simulation fidelity is multidimensional, consisting of physical, functional, and psychological fidelity.8,9 Physical fidelity is the most easily recognized of the three dimensions of fidelity. It involves the degree to which a simulation recreates the elements in a clinical situation, including the sensory characteristics (e.g., look, feel, sound, smell), personnel (e.g., patient, nurse, technician, physician), and equipment/monitor (e.g., electrocardiogram, oxygen saturation, capnograph).8,9
The ultimate objective of an emergency cricothyrotomy in a clinical “cannot intubate, cannot ventilate” (CICV) situation is to insert an airway device in the patient’s trachea in an expedient and correct manner with minimal complications.10 In this study, a crisis scenario was contextualized by enhancing the physical fidelity of a clinical CICV situation. Specifically, the scenario took place in a mocked operating room with a fully activated computerized patient mannequin (SimMan®), full monitors, alarms, and the presence of actors. The aim of this crossover study was to determine the impact of contextualizing a crisis scenario on the performance of a cricothyrotomy procedural task. Insertion time and complications in performing a cricothyrotomy in a CICV situation were compared in a contextualized scenario (CS) with high physical fidelity vs a verbalized non-contextualized scenario (NCS) with low physical fidelity. We hypothesized that contextualization of a crisis scenario would affect the performance of a cricothyrotomy procedural task.
Methods
Study population
Sixty-five participants, anesthesia assistants (n = 6) and emergency medicine (n = 23) and anesthesia residents (n = 36) at the University of Toronto (Toronto, ON, Canada) completed the study. The levels of training of the medical residents were postgraduate year 1-5 (PGY1-5) and fellows. The Institutional Research Ethics Committee of Mount Sinai Hospital (Toronto, ON, Canada) approved the study (April 08, 2010), and written informed consent was obtained from each participant.
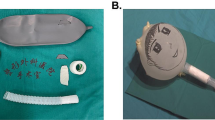
Tissue-mannequin simulator porcine larynx coupled to a SimMan mannequin (Fig. 1)
To address various issues related to performing a surgical cricothyrotomy on a tissue larynx in the context of a simulated CICV situation, a porcine larynx was coupled to a full-body computerized mannequin (SimMan, Laerdal Medical, Toronto, ON, Canada). The porcine larynx closely replicates the anatomy and texture of a human larynx.11 The tissue larynx also provides a more accurate assessment of complications associated with a cricothyrotomy when compared with the plastic trachea of the SimMan mannequin.
The tissue-mannequin simulator model. (A) The porcine larynx with a balloon attached at the end of the trachea and the skin-like silicone membrane. (B) The skin-like silicone membrane was secured on top of the porcine larynx. The larynx was then mounted on the neck of the SimMan® mannequin, secured with strings, and prepped with green towels. A 0.5-cm thick polystyrene board (4 × 4 cm) was placed behind the larynx to provide stability on the uneven neck of the mannequin. A white sheet was placed on top of the SimMan to cover the balloon and expose only the head and neck area. Rise of the white sheet with bag-mask ventilation confirmed successful insertion of the cricothyrotomy device in the trachea
Cricothyrotomy devices
Three cricothyrotomy kits were used in this study because of the variable availability in each academic hospital (eight hospitals) in the Departments of Anesthesia and Emergency Medicine at our institution (University of Toronto, Toronto, ON, Canada). Each department in each hospital is equipped with only one of the three kits in the difficult airway cart. Anesthesia and emergency medicine residents rotating in these hospitals during their residency training are required to become familiar with these kits. The three cricothyrotomy kits we used in the study were the Portex cuffed 6.0 mm (Portex 6.0), the Melker cuffed 5.0 mm (Melker 5.0), and the Melker uncuffed 3.5 mm (Melker 3.5). The Melker kits (Cook Medical, Bloomington, IN, USA) use the wire-guided Seldinger technique.12 The Portex 6.0 kit (Smiths Medical, Markham, ON, Canada) uses a tube-over-trocar technique with a red flag indication.13 Since the two different techniques (i.e., Seldinger and tube-over-trocar) have been shown to affect performances,13,14 each participant performed a cricothyrotomy with each of the two techniques using either the Portex 6.0 and Melker 3.5 cricothyrotomy kits or the Portex 6.0 and Melker 5.0 kits.
Teaching session
Two staff anesthesiologists conducted the teaching session in groups of four participants. Participants received a 30-min didactic lecture and a hands-on demonstration on how to perform a cricothyrotomy using the assigned devices. Participants were randomized to even and odd numbers using the online program RANDOMIZE.NET. Even-numbered participants (n = 32) were assigned the Portex 6.0 and Melker 3.5 kits and odd-numbered participants (n = 33) were assigned the Portex 6.0 and Melker 5.0 kits.
After the didactic lecture and hands-on demonstration, participants were familiarized with the kits and practiced with each kit on a plastic tube trachea model12 for a minimum of five times until they achieved plateau performance.15 Thereafter, participants practiced performing a cricothyrotomy once on a porcine larynx using each of the assigned kits. The porcine larynx was dissected after each practice to comment on tube placement and complications, with instructor feedback after each practice attempt.
Randomization of the first scenario to scenario type and kit
Within six weeks of the teaching session, the test session was conducted with individual participants. Each participant was expected to perform a cricothyrotomy using the assigned set of two cricothyrotomy kits (as in the teaching session) in each of NCS and CS, for a total of four cricothyrotomies on the tissue-mannequin simulator (Fig. 2). The order of scenario type and cricothyrotomy kit was randomly assigned for the first scenario only using RANDOMIZE.NET. Thereafter, each participant performed the second to fourth cricothyrotomies in the following sequence: after completing the first cricothyrotomy in the first scenario type, each participant performed a cricothyrotomy in the other scenario type using the same kit as in the first scenario. The third and fourth cricothyrotomies were performed using the other assigned kit in the same order of scenario type as the first and second cricothyrotomies.
Each participant waited in the debriefing room after completing each scenario while the porcine larynx was replaced with a freshly prepared larynx. After completing the four scenarios, each participant was debriefed by the study investigators and given feedback.
Test scenarios: CS and NCS
Prior to starting the first scenario, each participant was oriented to the simulation room, monitors, and equipment (SimSinai Centre, Mount Sinai Hospital, Toronto, ON, Canada). The simulation room included a fully computerized SimMan, full monitors (electrocardiogram, noninvasive blood pressure, pulse oximeter, end-tidal capnogram), alarms, and basic airway devices. The airway devices included a Macintosh laryngoscope blade (in sizes 3 and 4), a Miller laryngoscope blade, a gum elastic bougie, and a laryngeal maks (in sizes 3-5). A GlideScope® video laryngoscope (Verathon, Burnaby, BC, Canada) and a fibreoptic bronchoscope were supplied on request. The difficult airway cart was placed outside the room and contained the Melker 3.5, Melker 5.0, and Portex 6.0 cricothyrotomy kits. Following the orientation, the participant waited in the debriefing room while a porcine larynx covered with the skin-like silicone membrane was mounted on the neck of the SimMan mannequin.
The CS was conducted in a mocked operating room with a tissue-mannequin simulator and monitors and alarms that were activated. Actors playing the scripted roles of an operating room nurse and a respiratory therapist were present in the operating room. The scenario started when each participant was called to assist with an intubation attempt already underway in a patient with an unanticipated difficult airway who was induced with general anesthesia and paralyzed with rocuronium. On arrival, the oxygen saturation was 89% and decreasing 10% every minute to reach a nadir of 65%. A Cormack-Lehane grade 4 view of the larynx was simulated by inducing tongue swelling and pharyngeal blockage. All methods of intubation and ventilation were intended to be unsuccessful as the mannequin was set up in the CICV configuration. No backup help was available when requested. The scenario was designed to necessitate an emergency cricothyrotomy. The scenario terminated after completion of a cricothyrotomy with successful ventilation or at 300 sec after opening the cricothyrotomy kit package.
The NCS was also conducted in the same mocked operating room; however, the actors were absent and the tissue-mannequin simulator and monitors and alarms were not activated. A research assistant was present in the operating room to assist with the equipment and to verbalize the scenario: “A simulated patient underwent a general anesthesia and was paralyzed with rocuronium. Direct laryngoscopy intubation was unsuccessful on two attempts because of an unanticipated grade 4 view. Bag-mask and laryngeal mask were inadequate, and the oxygen saturation declined to 65%”.
After the scenario was verbalized, the participant was then instructed to proceed with managing the scenario. Termination of the NCS was identical to that of the CS.
Outcome measures
The porcine larynx was dissected after termination of each scenario to assess for device position and complications. The outcome measures were compared between the CS and NCS scenarios for each cricothyrotomy kit. The primary outcome measure was insertion time, measured from the time (sec) of opening the cricothyrotomy kit package to successful ventilation, defined as positive movement of the balloon (Fig. 1A) with bag-mask ventilation via the cricothyrotomy airway device. All kits were sealed in their original packaging prior to use. Secondary outcomes were: 1) Severity of injuries to the posterior pharyngeal and laryngeal wall – defined as average injury score using the grading system described by Murphy et al.16 – where 0 = none; 1 = mild (partial thickness puncture or laceration < 5 mm); 2 = moderate (partial thickness puncture or laceration > 5 mm); and 3 = severe (full thickness perforation). Average injury score was calculated by dividing the total score of each injury by the total number of injuries. 2) Failure – defined as any attempt in which the trachea was not cannulated or ventilated or which took >300 sec to perform after the kit package was opened.
Sample size
Sample size calculation was based on insertion time in a previous study17 and our observation of anesthesia residents in an airway course at the University of Toronto. A previous study of needle cricothyrotomy insertion time on a plastic mannequin reported a mean difference (MD) of 14 sec between CS and NCS.17 We observed a mean (SD) insertion time of 90 (35) sec with the cricothyrotomy kits in the anesthesia airway course. Assuming that the cricothyrotomy performed on a porcine larynx with the cricothyrotomy kits was more complex than performing a needle cricothyrotomy on a plastic mannequin,17 we estimated a larger difference in insertion time of 30 sec between CS and NCS. With an alpha of 0.05 and a power of 0.8, 21 participants were required to detect a difference of 30 sec between scenarios for each kit. Thirty-two participants were recruited to use the Portex 6.0 and Melker 3.5 kits, and 33 participants were recruited to use the Portex 6.0 and Melker 5.0 kits.
Statistical analyses
Statistical analyses were performed using SAS® 9.2 (SAS Institute Inc., NC, USA). To determine whether insertion time, average injury score, and failure rate differed across kits and across scenario type, a series of mixed models were constructed. Unlike traditional approaches to analysis that typically assume independence of observations, mixed models are appropriate for use in situations where we anticipate some degree of relatedness between outcome measures, such as in a crossover study. Full maximum likelihood estimation was selected as the method of estimation for each of the outcome analyses, and a variety of potential covariance structures were investigated (variance components, compound symmetric and heterogeneous compound symmetric covariance, first-order autoregressive and heterogeneous first-order autoregressive covariance, and unstructured covariance).
In this crossover study, participants were exposed to two conditions, i.e., scenario type and cricothyrotomy kit. The magnitude of the effect of these conditions may be dependent on the order in which the conditions were presented. Thus, we must consider two distinct types of order effects, namely, order effects of scenario type (CS and NCS) and order effects of cricothyrotomy kits (Melker and Portex kits). To determine whether order of scenario type and kit had an effect on insertion time and injury score, we used a first-order autoregressive covariance structure for analysis. To assess the effects of the order of scenario type and kit on failure rate, a series of generalized estimating equations were used for analysis. After we determined that the order of the scenario type and cricothyrotomy kit did not affect the outcome measures, the data for each outcome measure were pooled for each scenario and for each kit. A paired Student’s t test was used to analyze the pooled insertion time and average injury score between NCS and CS for each kit. The pooled failure rate between NCS and CS for each kit was analyzed using Fischer’s exact test. All reported P values are two sided.
Results
The characteristics of the participants are shown in Table 1. Sixty-five participants completed the study, 36 anesthesia residents, 23 emergency medicine residents, and six anesthesia assistants (Table 1). The majority of the resident participants were PGY 1-3. The anesthesia assistants had a minimum of five years of clinical experience. Over half of all participants had received previous formal training in the use of the Melker kit, but only anesthesia trainees and anesthesia assistants had received previous formal training in the use of the Portex kit. All participants had previous experience in simulation; however, none of the participants had previously performed a cricothyrotomy on a patient.
Since the order of scenario type and kit did not affect insertion time, average injury score, and failure rate (Table 2), each outcome measure was pooled for each device and each scenario. Table 3 shows that the primary outcome measure, mean (SD) insertion time of successful cricothyrotomy, did not differ significantly between NCS and CS for the Melker 3.5 [83.0 (45.0) sec vs 63.3 (36.1) sec, respectively; P= 0.96; MD, 19.7 sec; 95% confidence interval (CI) −1.9 to 41.3], the Melker 5.0 [86.5 (36.8) sec vs 107.1 (55.6) sec, respectively; P =0.11; MD, −20.6 sec; 95% CI, −44.9 to 3.7], and the Portex 6.0 [59.5 (35.5) sec vs 59.0 (35.0) sec; P = 0.95; MD, 0.5 sec; 95% CI, −13.2 to 14.2].
Secondary outcome measures for severity of injuries, measured as the mean (SD) of the average injury score, were similar between NCS and CS for the Melker 3.5 [0.71 (0.79) vs 0.75 (0.78), respectively; P = 0.88; MD, 0.04; 95% CI, −0.39 to 0.46], the Melker 5.0 [1.45 (0.69) vs 1.32 (0.73), respectively; P = 0.80; MD, 0.13; 95% CI, −0.24 to 0.50], and the Portex 6.0 [1.74 (0.63) vs 1.73 (0.56), respectively; P = 0.98; MD, 0.01; 95% CI, −0.23 to 0.24] (Table 4). Furthermore, the failure rate for each kit was also similar between scenarios (Table 4).
Discussion
This crossover study aimed to assess a cricothyrotomy procedural task performed on a tissue-mannequin simulator using two cricothyrotomy kits in both a contextualized and a verbalized non-contextualized CICV scenario. Our results showed that, despite using different techniques and cricothyrotomy kits (the Seldinger technique with the Melker kits and the tube-over-trocar technique with the Portex kit), mean insertion time, mean average injury score, and mean failure rate in performing cricothyrotomy using each kit were not significantly different between CS and NCS. Contrary to our hypothesis, the results suggest that contextualization of a crisis scenario did not affect the performance of a cricothyrotomy procedural task. These findings may have important implications for the feasibility and cost-effectiveness of evaluating the performance of cricothyrotomy procedural tasks.
Our findings are in contrast to a study by John et al.17 who showed that needle cricothyrotomy insertion time was significant longer in the context of a simulated CICV scenario (i.e., on an activated full-body patient simulator mannequin in a mock operating room with actors, activated monitors, and alarms) when compared with a verbalized scenario on an inanimate mannequin in a classroom without the clinical context. Possible reasons for the differences in results could be due to different techniques, devices, and models used between studies. In our study, performing a cricothyrotomy on a porcine larynx using the Portex and Melker kits is technically more complex than performing a needle cricothyrotomy on a plastic mannequin.17
Our results are similar to those in a crossover study by Finan et al. who showed that performing neonatal resuscitation on a full-body infant simulator during a simulated cardiac arrest scenario was not different from performing a verbalized cardiac arrest scenario on a training infant mannequin.18 A possible explanation for our findings and those of the previous study18 is that, although the degree of physical fidelity differed between the two scenarios, psychological fidelity may be equally high for both. Psychological fidelity involves the extent to which participants engage in tasks that generate actions and processing demands that are similar to those in the clinical environment.19 Accurately reproducing stressful conditions is a prime example. In task domains where life and death are at stake, a high degree of psychological fidelity can achieve a level of stress closer to that experienced in the real-life situation. This view is supported by the study of Finan et al.18 who showed that the level of stress cortisol was similarly elevated in both NCS and CS, suggesting that psychological fidelity was high in both scenarios. There is some evidence to suggest that there can be a disconnect between psychological and physical fidelity and that psychological fidelity may be a more important factor in influencing the performance of procedural tasks. Limited studies comparing low and high physical fidelity simulations in the presence of high psychological fidelity have shown equivalent performance.20,21 This may also be true in our study, implying that participants may be fully immersed in CS and NCS and perceive both scenarios as life-threatening. The participants would therefore perform an emergency cricothyrotomy with equal expediency and safety regardless of the physical fidelity and clinical content.
A second potential explanation for the lack of differences in outcomes between scenarios is that, by the time the participants decided to open the cricothyrotomy kit, they were extremely focused and motivated to complete the procedural task as quickly as possible in order to provide oxygenation. Evidence has shown that physicians can perform highly motivated tasks equally well under various conditions because task motivation obviates background distraction.22 In this study, task motivation may obviate the effects of the distractors (actors, monitors, alarms) experienced in the CS.
Insertion time and complications in performing a cricothyrotomy procedural task were assessed in this study. These outcomes are critical when performing an emergency cricothyrotomy since a prolonged insertion time and severity of complications can result in brain hypoxia and death.2 Although we did not find an effect of contextualization on task performance, it is possible that our outcome measures were inadequate to detect differences in performance between scenarios. Currently, evidence suggests that the combination of a checklist and a global rating scale provides a comprehensive assessment to evaluate procedural skills23 and may capture differences in performance between NCS and CS. A future study using these assessment tools to compare cricothyrotomy procedural skills of NCS vs CS merits further research.
It is argued that a procedural task should be assessed in simulations that are realistic and grounded in an authentic clinical context that recreates key components of the clinical experience.6 Performing a procedural task in isolation on a bench top model may not reflect performances that are encountered in various clinical situations. Kneebone et al. proposed that contextualizing a simulation allows for the assessment of medical procedures in a range of diverse contexts that may be encountered in the clinical settings.6,7 For example, performing an intravenous on a plastic mannequin arm with an integrated patient actor who is angry can become very challenging compared with performing the same procedure on a calm patient.6,7 These findings imply that performance of procedural tasks can be influenced by the clinical context of the simulation. In contrast, our findings showed that contextualization had a lack of effect on the performance of a cricothyrotomy procedural task. Unlike procedural tasks performed in non-crisis situations, it would seem that emergency procedural tasks, such as a cricothyrotomy, that must be performed quickly in a crisis situation may appear to be resistant to the effects of the clinical context.
A full-body patient mannequin coupled with a porcine larynx that closely replicates the anatomy and texture of a human larynx represents a simulator model of high fidelity that can simulate a CICV situation.11 The tissue-mannequin simulator may represent an ideal simulation to assess both cricothyrotomy procedural skills and cognitive behaviours (i.e., individual and team) in a simulated CICV scenario. Nevertheless, our findings showed that embedding a clinical context in a crisis scenario did not influence the performance of a cricothyrotomy procedural task. This outcome is important for evaluating this life-saving procedural task since replicating a clinical context and enhancing physical fidelity simulation is resource extensive and costly.6,7,24 A part task trainer of an isolated porcine larynx would likely be more feasible and cost-effective for evaluating insertion time and complications in performing a cricothyrotomy.
There are several limitations to this study. Carryover effects between scenarios may confound the outcomes in this crossover study. A washout period between scenarios can minimize carryover effects; however, this study did not have washout periods between scenarios because the duration of washout periods is often unknown.25 Although the order of the scenario and kit was randomly assigned and ordering effects were excluded as a source of bias, learning over the course of the test session (i.e., four cricothyrotomies) could arguably influence the outcomes. Nevertheless, it is unlikely that using the Seldinger technique with the Melker kits would influence the tube-over-trocar technique with the Portex kit (and vice versa) since these two techniques and devices are very different. Many factors can affect clinical performance, including environmental, patient, and operator factors.26 Since these factors were not investigated, the performances observed in this study cannot be directly extrapolated to real-life cricothyrotomies. Many simulations, including human cadavers, plastic mannequins, animal larynx, and live animals, have been used as a surrogate for the human larynx.12-17 Fresh human cadaver is considered the simulation with the highest degree of fidelity to teach and evaluate cricothyrotomy skills; however, supply and ethical considerations limit its availability. The porcine larynx is considered an acceptable model with anatomical structures similar to the human neck11 and is frequently employed in cricothyrotomy studies.16 The porcine larynx of our tissue-mannequin simulator lacks blood vessels and significant subcutaneous tissue below the skin-like silicone membrane. Thus, the tissue-mannequin simulator does not reflect the complexity of neck tissue and bleeding that could affect a cricothyrotomy performed on a patient.
In summary, insertion time and complications in performing a cricothyrotomy on a tissue-mannequin simulator using two different cricothyrotomy kits were similar between CS and NCS. These results suggest that contextualization of a crisis scenario did not affect the performance of a cricothyrotomy procedural task. Our findings may have important implications for the feasibility and cost-effectiveness in using simulation to evaluate the performance of a cricothyrotomy procedural task.
References
Wong DT, Lai K, Chung FT, Ho RY. Cannot intubate-cannot ventilate and difficult intubation strategies: results of a Canadian national survey. Anesth Analg 2005; 100: 1439-46.
Cook TM, Woodall N, Frerk C. Fourth National Audit Project. Major complications of airway management in the UK: results of the Fourth National Audit Project of the Royal College of Anaesthetists and the Difficult Airway Society. Part 1: anesthesia. Br J Anaesth 2011; 106: 617-31.
Kneebone R, Kidd J, Nestel D, Asvall S, Paraskeva P, Darzi A. An innovative model for teaching and learning clinical procedures. Med Educ 2002; 36: 628-34.
Hubert V, Duwat A, Deransy R, Mahjoub Y, Dupont H. Effect of simulation training on compliance with difficult airway management algorithms, technical ability, and skills retention for emergency cricothyrotomy. Anesthesiology 2014; 120: 999-1008.
Vadodaria BS, Gandhi SD, McIndoe AK. Comparison of four different emergency airway access equipment sets on a human patient simulator. Anaesthesia 2004; 59: 73-9.
Kneebone R, Nestel D, Yadollahi F, et al. Assessing procedural skills in context: exploring the feasibility of an Integrated Procedural Performance Instrument (IPPI). Med Educ 2006; 40: 1105-14.
Kneebone R. Evaluating clinical simulations for learning procedural skills: a theory-based approach. Acad Med 2005; 80: 549-53.
Hays RT, Singer MJ. Simulator Fidelity in Training Systems Design - Bridging the Gap Between Reality and Training. NY: Springer-Verlag; 1989 .
Rehmann AJ, Mitman RD, Reynolds MC. A Handbook of Flight Simulation Fidelity Requirements for Human Factors Research. Federal Aviation Administration Technical Center; 1995.
Sulaiman L, Tighe SQ, Nelson RA. Surgical vs wire-guided cricothyrotomy: a randomised crossover study of cuffed and uncuffed tracheal tube insertion. Anaesthesia. 2006; 61: 565-70.
Olshaker JS, Brown CK, Arthur DC, Tek D. Animal procedure laboratory surveys: use of the animal laboratory to improve physician confidence and ability. J Emerg Med 1989; 7: 593-7.
Friedman Z, You-Ten KE, Bould MD, Naik V. Teaching lifesaving procedures: the impact of model fidelity on acquisition and transfer of cricothyrotomy skills to performance on cadavers. Anesth Analg 2008; 107: 1663-9.
Assmann NM, Wong DT, Morales E. A comparison of a new indicator-guided with a conventional wire-guided percutaneous cricothyrotomy device in mannequins. Anesth Analg 2007; 105: 148-54.
Benkhadra M, Lenfant F, Nemetz W, Anderhuber F, Feigl G, Fasel J. A comparison of two emergency cricothyroidotomy kits in human cadavers. Anesth Analg 2008; 106: 182-5.
Wong DT, Prabhu AJ, Coloma M, Imasogie N, Chung FF. What is the minimum training required for successful cricothyrotomy?: a study in mannequins. Anesthesiology 2003; 98: 349-53.
Murphy C, Rooney SJ, Maharaj CH, Laffey JG, Harte BH. Comparison of three cuffed emergency percutaneous cricothyroidotomy devices to conventional surgical cricothyroidotomy in a porcine model. Br J Anaesth 2011; 106: 57-64.
John B, Suri I, Hillermann C, Mendonca C. Comparison of cricothyroidotomy on manikin vs. simulator: a randomised cross-over study. Anesthesia 2007; 62:1029-32.
Finan E, Bismilla Z, Whyte HE, Leblanc V, McNamara PJ. High-fidelity simulator technology may not be superior to traditional low-fidelity equipment for neonatal resuscitation training. J Perinatol 2012; 32: 287-92.
Khan K, Pattison T, Sherwood M. Simulation in medical education. Med Teach 2011; 33: 1-3.
Matsumoto ED, Hamstra SJ, Radomski SB, Cusimano MD. The effect of bench model fidelity on endourological skills: a randomized controlled study. J Urol 2002; 167: 1243-7.
Chandra DB, Savoldelli GL, Joo HS, Weiss ID, Naik VN. Fiberoptic oral intubation: the effect of model fidelity on training for transfer to patient care. Anesthesiology 2008; 109: 1007-13.
Hayter MA, Friedman Z, Katznelson R, Hanlon JG, Borges B, Naik VN. Effect of sleep deprivation on labour epidural catheter placement. Br J Anaesth 2010; 104: 619-27.
Morgan PJ, Cleave-Hogg D, Guest CB. A comparison of global ratings and checklist scores from an undergraduate assessment using an anesthesia simulator. Acad Med 2001; 76: 1053-5.
Hoffman KI, Abrahamson S. The ‘cost-effectiveness’ of Sim One. J Med Educ 1975; 50(12 Pt 1): 1127-8.
Senn S. Cross-Over Trials in Clinical Research, Second Edition. Wiley; 2002.
Greenland KB, Acott C, Segal R, Goulding G, Riley RH, Merry AF. Emergency surgical airway in life-threatening acute airway emergencies–why are we so reluctant to do it? Anaesth Intensive Care 2011; 39: 578-84.
Acknowledgement
We thank Larni Guerina, the research assistant, for recruiting the participants and helping to conduct the study and collect the data.
Funding
This work was supported by a research grant from the Canadian Anesthesiologists’ Society, Toronto, ON, Canada.
Conflicts of interest
None declared.
Author information
Authors and Affiliations
Corresponding author
Additional information
Author contributions
Kong E. You-Ten designed the study, conducted the study, analyzed the data, and wrote the manuscript. Catherine Wong helped analyze the data and write the manuscript. Catherine Wong, Cristian Arzola, Jessica Cheung, and Naveed Siddiqui helped conduct the study. Catherine Wong, Cristian Arzola, Jessica Cheung, Naveed Siddiqui, Zeev Friedman, and Sev Perelman helped review the manuscript. Zeev Friedman and Sev Perelman helped design the study.
Rights and permissions
About this article
Cite this article
You-Ten, K.E., Wong, C., Arzola, C. et al. Role of contextualizing a crisis scenario on the performance of a cricothyrotomy procedural task. Can J Anesth/J Can Anesth 62, 1104–1113 (2015). https://doi.org/10.1007/s12630-015-0430-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-015-0430-z