Abstract
High rates of maternal mortality remain a widespread problem in the developing world. Skilled anesthesia providers are required for the safe conduct of Cesarean delivery and resuscitation during obstetrical crises. Few anesthesia providers in low-resource settings have access to continuing education. In Rwanda, anesthesia technicians with only three years of post-secondary training must manage complex maternal emergencies in geographically isolated areas. The purpose of this special article is to describe implementation of the SAFE (Safer Anesthesia From Education) Obstetric Anesthesia course in Rwanda, a three-day refresher course designed to improve obstetrical anesthesia knowledge and skills for practitioners in low-resource areas. In addition, we describe how the course facilitated the knowledge-to-action (KTA) cycle whereby a series of steps are followed to promote the uptake of new knowledge into clinical practice. The KTA cycle requires locally relevant teaching interventions and continuation of knowledge post intervention. In Rwanda, this meant carefully considering educational needs, revising curricula to suit the local context, employing active experiential learning during the SAFE Obstetric Anesthesia course, encouraging supportive relationships with peers and mentors, and using participant action plans for change, post-course logbooks, and follow-up interviews with participants six months after the course. During those interviews, participants reported improvements in clinical practice and greater confidence in coordinating team activities. Anesthesia safety remains challenged by resource limitations and resistance to change by health care providers who did not attend the course. Future teaching interventions will address the need for team training.
Résumé
Les forts taux de mortalité maternelle restent un problème général dans les pays en développement. Des praticiens compétents en anesthésie sont nécessaires pour mener à bien et sans danger un accouchement par césarienne et la ressuscitation en cas d’urgence obstétricale. Peu de praticiens en anesthésie ont accès à une éducation continue dans des contextes aux ressources limitées. Au Rwanda, des techniciens en anesthésie n’ayant que trois années de formation post secondaire doivent gérer des urgences maternelles complexes dans des régions géographiquement isolées. L’objectif de cet article spécial est de décrire la mise en œuvre du cours d’anesthésie obstétricale SAFE (pour Safer Anesthesia From Education) au Rwanda, un cours de rappel de trois journées destiné à améliorer les connaissances en anesthésie obstétricale et les compétences des praticiens exerçant dans des zones à faibles ressources. De plus, nous décrivons comment le cours a facilité le cycle de passage des connaissances à l’action (KTA: knowledge-to-action) pendant lequel une série d’étapes sont suivies pour encourager l’intégration des nouvelles connaissances dans la pratique clinique. Les cycles de KTA nécessitent des interventions pédagogiques localement pertinentes et le maintien du savoir après l’intervention. Au Rwanda, cela a signifié de prendre soigneusement en compte les besoins éducatifs, réviser les programmes pour s’adapter au contexte local rwandais, utiliser un apprentissage actif des expériences pendant le cours d’anesthésie obstétricale SAFE, encourager des relations de soutien avec les pairs et les mentors et en utilisant les plans d’action des participants pour le changement, tenus de registres après le cours, et des entretiens de suivi avec les participants six mois après le cours. Pendant ces entrevues, les participants ont noté des améliorations dans la pratique clinique et une plus grande confiance dans la coordination des activités en équipe. La sécurité de l’anesthésie demeure mitigée par des ressources limitées et la résistance au changement de la part du personnel de soins de santé qui n’ont pas assisté aux cours. Les futures interventions d’enseignement aborderont le besoin d’une formation en équipe.
Similar content being viewed by others
“The risk of a woman dying as a result of pregnancy or childbirth during her lifetime is about one in six in the poorest parts of the world compared with about one in 30,000 in Northern Europe.” 1
The purpose of this special article is to describe work that has been undertaken to improve maternal morbidity and mortality in Rwanda through the SAFE (Safer Anesthesia From Education) Obstetric Anesthesia course. This three-day refresher course was developed by the Association of Anaesthetists of Great Britain and Ireland (AAGBI) to improve obstetric anesthesia practice for practitioners in low-resource countries.Footnote 1
Worldwide, the maternal mortality rate remains unacceptably high. In 2010, approximately 287,000 women around the world died from complications of pregnancy and childbirth.2 Despite improvements in obstetrical anesthesia in many low-resource countries,3 there is an urgent need for safer maternal care.
Multiple factors contribute to poor maternal outcomes in low-resource settings, including lack of skilled birth attendants, late presentations to health centres, delays in transport for definitive care, shortages of essential medications and supplies, insufficient monitoring, and inadequate training of primary health responders.4 The major causes of maternal death worldwide are hemorrhage, hypertensive disorders, sepsis, and complications of abortion.5 Well-trained anesthesia providers are essential for managing these complications and for resuscitating critically ill patients. Cesarean delivery, the most common major surgical procedure in sub-Saharan Africa,6 requires anesthesia services. Perioperative mortality for Cesarean delivery in sub-Saharan Africa is high (1-2%), and one-third of deaths are attributable to anesthesia.7
The issue: high maternal mortality in Rwanda
Following the Rwandan genocide in 1994, only one physician anesthesiologist remained in the country.8 Despite an impressive countrywide regeneration, there are still only 12 physician anesthesiologists for a population of more than 11.5 million.9 All physician anesthesiologists are based at teaching hospitals in just two cities, Kigali and Huye (formerly Butare). Anesthesia services in the rest of the country are provided entirely by anesthesia technicians who, at most, have completed three years of post-secondary training. A few technicians have received only on-the-job training. Technicians who work under harsh circumstances and in geographic isolation must manage complex patient problems without supervision.10 They have few opportunities for continuing education or even professional interaction.
The Rwandan birth rate is high11 and Cesarean deliveries comprise the majority of surgical procedures in the district hospitals.12 Maternal mortality in Rwanda has been estimated to be 340 deaths per 100,000 live births in 2010 (as compared with Canada with 12 deaths per 100,000 live births in 2010).13 A prospective observational study at Muhima District Hospital in Kigali reveals substandard anesthetic management for patients undergoing Cesarean delivery.14 Pre-anesthetic assessment was omitted (95% of patients), general anesthesia was given with an unprotected airway (84% of patients), and the decision-to-delivery interval was consistently greater than 30 min. The investigators found the maternal mortality rate for Cesarean delivery at that hospital to be 500 deaths per 100,000 live births.
The intervention: knowledge translation through the SAFE Obstetric Anesthesia course
The authors are a group of Rwandan, Canadian, and American anesthesia providers and education specialists who have collaborated to build capacity for obstetric anesthesia care in Rwanda. The Canadian Anesthesiologists’ Society International Education Foundation (CAS IEF) has a long-standing partnership with the University of Rwanda for anesthesia resident education.15 Our collective experience confirms deficiencies in obstetric anesthetic care and non-technical skills (e.g., teamwork, leadership, and communication). Based on knowledge gained through the CAS IEF-Rwanda partnership and the compelling need for better maternal outcomes, we set out to improve capacity for obstetric anesthesia services in Rwanda by offering the SAFE course to anesthesia technicians.
Ethical considerations
Although our primary purpose in bringing the SAFE course to Rwanda was educational, we planned a preliminary investigation of program results. Accordingly, we obtained ethics approval for formal reporting from the Research Ethics Boards at both Dalhousie University, in Canada, and the University of Rwanda (Dalhousie University approval September 2012 – File 2012-2756; University of Rwanda approval November 2012). All anesthesia technicians who attended the SAFE course were given an opportunity to participate in subsequent evaluations. Immediately prior to the course, the participants were given a full explanation of our related study rationale in English, French, or Kinyarwanda, as required, and they were also given an opportunity to have their questions answered. Participants were assured that data would be confidential and de-identified. All ninety course participants gave informed written consent.
Knowledge translation
Simply delivering an educational course does not ensure habits will be changed. This is addressed by the field of knowledge translation that examines the incorporation of new knowledge into practice.16 Indeed, the dynamic educational process that can lead to sustained change in clinical practice has been described by Graham et al. as the knowledge-to-action (KTA) cycle.17 Each step of the KTA cycle is informed by prior steps. Shaped by the interaction of teachers, learners, and context, there are abundant opportunities to modify strategies to achieve desired goals. The basic premise is that learners are more likely to implement changes in practice that are relevant to their needs and appropriate to their context. Consequently, we applied the KTA cycle in Rwanda by understanding the local needs, adapting the SAFE course for Rwandan circumstances, active hands-on learning, dialogue between participants and mentors, discussions around enablers and barriers to practice change, and follow-up visits with participants after the course (Fig. 1).
Adapted knowledge-to-action cycle. Shows the knowledge-to-action (KTA) cycle and its application in Rwanda. Adapted with permission from: Graham et al. 17
SAFE obstetric anesthesia course in Rwanda
The SAFE course is designed to improve participants’ knowledge and skills in obstetric anesthesia through interactive learning. The program contains only a few lectures, while most of the course involves active teaching methods with rotation through small group stations. Using low-fidelity models, participants practice skills and engage in simulated scenarios. Topics include essential obstetric anesthesia knowledge and skills, management of critical events, and non-technical skills (Table 1). The basics of the course are predesigned, but it can be modified to suit the learners and the environment. The planning committee for the SAFE course in Rwanda included knowledgeable faculty members, both physician and non-physician, in Rwanda and colleagues in Canada and the United States who were thoroughly familiar with the Rwandan environment.
A training-of-trainers (TOT) course is embedded in the SAFE course so that future programs can be offered without outside support. Just before the SAFE course began, trainers attended a one-day course to learn techniques for lecturing, skills teaching, and running simulated scenarios. During the SAFE course, experienced mentors supervised TOT participants as they applied their new teaching skills.
Prior to being offered in Rwanda, the SAFE course had been run successfully in Uganda, Liberia, and Ghana. The Rwandan course was the first for non-English speaking anesthesia providers. Most Rwandan anesthesia technicians have been educated in French, although their native language is Kinyarwanda. English was recently introduced as a third official language, but very few technicians are fluent. Language considerations prompted us to adapt the SAFE course for the local context by simplifying the curriculum, eliminating medical acronyms, and increasing opportunities for active learning. We also ensured that during small group sessions in the course, non-Rwandan teachers were always paired with a trainer capable of translating from English to French or Kinyarwanda.
A few months prior to the SAFE course, the Rwandan faculty selected ninety anesthesia technicians, representing about half of the Rwandan district hospitals, to participate in the course. Twenty-six trainers, including senior anesthesia technicians and anesthesia residents, were invited for the TOT course (Fig. 2).
In the weeks leading up to the SAFE course, we conducted a needs assessment for course participants to identify their learning goals. In particular, the participants expressed discomfort and/or inexperience with difficult airways, preeclampsia and eclampsia, postpartum hemorrhage, maternal sepsis, perioperative pain management, and the WHO Surgical Safety Checklist.18 Based on information obtained from the needs assessment, these topics were given special emphasis during the course.
On the day before the SAFE course, participants were invited to attend a full-day workshop to reflect on their current practice. They were encouraged to explore positive and negative anesthesia practice experiences in order to identify areas of difficulty that would require further development as well as areas of strength on which to build. Strengths that were identified included an expressed commitment to patient care and past experiences of positive communication in the operating room. Identified challenges included the resistance to change from other surgical team members and hospital administration, a lack of self-confidence on the part of the anesthesia providers (due to existing power dynamics, poor continuing education, or both), and a shortage of resources (e.g., staff, drugs, and equipment) necessary for good patient care. These pre-course discussions primed the participants to begin to contemplate change.
In January 2013, the first Rwandan SAFE course was held at a hotel in Rwamagana in the eastern part of the country. The venue was selected in a quiet location away from the major cities where participants and faculty could stay together for the duration of the course. This provided great opportunity for ongoing interaction, not just between faculty and students but also among participants from different regions. A sense of great camaraderie grew as anesthesia providers realized they were not alone in facing problems and challenges in their profession - many of these were common to all. The participants and faculty intermingled continuously and there was ample opportunity to discuss issues, ask and answer questions, and generally share concerns about the practice of anesthesia. This setup prepared the way for the development of a post-course peer and mentor network, which we called the “Anesthesia Practice Network” (APN).
The APN was designed to support participants in practice change after the course and to reduce their sense of isolation. During the course, mentors assigned to geographic regions met with small groups of participants from that area. These meetings formed the beginning of peer and mentor relationships of the APN. In guided discussions amongst APN members, participants considered barriers and enablers to practice change. They reflected on their own knowledge and confidence, capacity of colleagues, and available resources in their home hospitals. Mentors encouraged participants to develop realistic plans for implementing their new learning. Through these discussions, participants found support in their colleagues and realized that many practice obstacles are widespread.
At the start of the SAFE course, many participants appeared anxious because they were not used to small-group hands-on sessions. But once their familiarity grew, so did their confidence to speak out and participate actively (Fig. 3). This freedom permitted them to be much more active in their learning. The idea of working as a team with surgeons, nurses, and others to improve patient care was a new concept to many. It was clear to the faculty that most of the anesthesia technicians felt isolated in their institutions and that the idea of sharing knowledge or seeking assistance from other members of the surgical team was uncomfortable. It appeared that many considered that asking for help implied professional weakness and was somehow shameful. Participating in role-play scenarios to practice the Surgical Safety Checklist provided them with a great deal of insight into the issues facing the surgeons and the nurses.
The textbook, Obstetric Anaesthesia for Developing Countries,Footnote 2 developed by the Association of Anaesthetists of Great Britain and Ireland describes strategies to provide safe and practical anesthesia for obstetric patients in low-resource environments. The textbook includes discussion of maternal physiology, monitoring, pain relief, regional anesthesia, general anesthesia, obstetric complications, and neonatal resuscitation. As the textbook and the SAFE course address the same problems, we distributed copies of the book during the course as a supplement to the curriculum. The textbook is available only in English, but as it was written in straightforward language, we considered it would be valuable to participants.
Ninety Lifebox® Footnote 3 pulse oximeters were given to participants to begin countrywide distribution of 250 pulse oximeters (funded by donations to CAS IEF). In small group sessions, participants learned instructions for use of the pulse oximeters and algorithms for managing hypoxia.
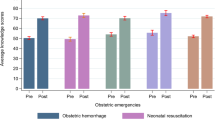
By design, the SAFE course includes pre- and post-course testing of skills and knowledge. These tests allow participants to realize improvements they made during the course. Gratifying improvements were seen in both skills and knowledge, but it is difficult to quantify these in a clinically relevant way.
To consolidate learning and promote knowledge translation, once participants had completed the course, they were asked to identify practice changes they intended to make and to identify factors they anticipated would help or hinder fulfillment of these plans. Each participant formally recorded his or her own action plans on a personal Commitment to Change form. De-identified copies of the Commitment to Change forms were given to the research team. The participants were asked three questions:
-
1.
What three changes do you intend to make in your anesthesia practice as a result of participating in this course?
-
2.
What obstacles do you anticipate in attempting to make these changes?
-
3.
What factors would help you to make these changes?
Accordingly, the intended changes listed on the Commitment to Change forms were:
-
Implementation of the WHO Surgical Safety Checklist18
-
Improved teamwork and communication
-
Conducting pre-anesthesia assessment
-
Performing left lateral tilt
-
Preparation of drugs and materials in advance
Participants identified obstacles to change as:
-
Lack of equipment and drugs
-
Training deficiencies
-
Resistance to change from other team members (e.g., surgeons, nurses)
-
Poor teamwork
-
Staff shortages
-
Limited engagement from hospital administrators
Factors that might enable change were reported to be:
-
Building relationships and communication with colleagues
-
Engaging authorities to secure adequate resources and equipment
-
Inclusive training for the whole operating team
-
Implementing hospital policies and protocols
On the final day of the SAFE course, participants were given logbooks to maintain after the course. They were asked to record cases where they considered knowledge or skills gained through the course had made a direct impact on patient outcome. It was explained to the participants that the logbook entries were intended to reinforce learning and to guide further case discussions with mentors.
Anesthesia practice network
The description thus far has addressed steps in the KTA cycle from “identifying the problem” to “selecting and implementing interventions”. The remaining three steps of the KTA cycle apply to work undertaken following the course to enhance use of new knowledge and skills in practice. We considered that use of new knowledge would be sustained best by peer and mentor support in the APN.
Peer support was easily achieved, as peers work in the same region; however, the vision of the APN was only partially fulfilled. The intended vision had been for mentors to make visits to their geographic groups at three months and six months post-course. Due to funding restrictions, however, formal mentor visits following the course were possible only in Eastern Province, Rwanda. Nevertheless, a few participants contacted their mentors by telephone to discuss cases. Participants pointed out that, prior to the course, they would have been uncomfortable contacting an anesthesiologist in an urban centre, but after the course, they were more willing to ask advice from peers and mentors.
The mentors who had been able to make site visits to district hospitals had requested criteria to guide clinical practice discussions. Based on this request, we designed an anesthesia checklist for Cesarean delivery (Appendix 1). Mentors are now using this checklist as an educational tool, and it has been included as part of the Rwandan SAFE course materials.
Six months following the course, several of our group (G.N., E.N., P.L. in Eastern Province and G.N., E.N., P.B.R. in Kigali Province) made site visits to a purposive sample of participants who had completed the course and participated in the APN. Purposive sampling involves identifying participants and situations that best enable the researchers to understand the subject being studied.19 During these visits, we reviewed the contents of logbooks with participants and conducted semi-structured individual interviews (Table 2). The interviews were audio recorded and later transcribed.
Interviews were conducted in French, Kinyarwanda, or English in accordance with the comfort level of the participant. The interviews in French or Kinyarwanda were translated into English to allow data analysis by the full research team. Eleven interviews were conducted with participants in Eastern Province (rural district hospitals), and ten interviews were conducted in Kigali Province (urban hospitals).
Several members of the research team (P.L., G.N., E.N., and P.B.R.) independently read and analyzed the transcripts to identify initial themes and then discussed their findings to check for agreement and resolve any differences. Through this process, major themes were identified and subsequently clustered. Data collection and analysis were iterative rather than sequential; emerging themes informed subsequent data collection.19
The impact: post-course changes in knowledge and action
Major themes that emerged from the analysis included practice improvements, such as routinely performing preoperative assessment, better preparation for anesthesia, employing left lateral tilt, and systematic management of emergencies. Participants described greater confidence in sharing ideas for practice change and found support from peers who shared the SAFE course. They struggled with resistance to change by colleagues who had not received the training and difficulties in providing proper care due to shortages of resources. Participant quotes illustrate these themes.
An example of better preparation for anesthesia is described as:
“There are things we knew before but did not practice. By using the skills we learned during SAFE, anesthesia is safer and stress is reduced. Our complications are reduced and management is easy. I cannot forget preparation and assessment before any intervention. This means preparation of material, machine, oxygen, and the patient, even if it is an emergency.”
Left lateral tilt had not been commonly used prior to the course. Sixteen of the 21 participants identified this as a change they had made after the course, with fewer episodes of hypotension noted.
“We used to have more cases of hypotension but now we are using tilt we don’t have as many. We used to have much more problem and had to give ephedrine for falling blood pressure.”
Participants described confidence to manage emergencies systematically. The following quote describes successful management of a patient with severe postpartum hemorrhage. Prior to the SAFE course, she would have been transferred without resuscitation to a hospital one hour away, making survival unlikely.
“Prior to the SAFE course the patient would have been sent to [referral hospital]. This time I decided to do something. I learned in SAFE about the ABCs. The airway was okay but the problems were with B and C. We got two IVs and sent blood for cross match. We gave IV fluids and oxygen. We went to theatre and induced with ketamine, sux, and fentanyl and intubated. She was bleeding from inside and they opened her and repaired. The patient survived.”
Participants identified a hierarchy amongst the caregivers, with surgeons who are medical doctors dominating over the relatively subordinate anesthesia technicians. This can hinder communication for patient care. After the course, participants described greater confidence in advocating for patient safety within the operating room team. At several hospitals, SAFE course graduates had gathered surgeons, nurses, and midwives together to implement the WHO Surgical Safety Checklist (SSCL) and to discuss strategies to improve team communication. The following quotes provide examples of improved confidence among anesthesia technicians in advocating for change even though there is a status differential.
“The team from anesthesia who attended the SAFE course had a meeting with the whole staff to explain the importance of the SSCL. We also explained the importance of preparation. This meeting was for doctors, nurses and midwives. We explained about SSCL, team communication and preparation. They had many questions. We explained that it is important to know about allergies and what is not functioning well. Finally, they have taken responsibility. If something is missing we make sure. Gradually we are getting more and more acceptance.”
“The SAFE course gave us confidence to do the best thing for patient safety without fearing the surgeons.”
Participants were more willing to ask for help.
“Before I was feeling it is shameful to call someone for help but after SAFE course I felt confident to call and no shame at all.”
When several anesthesia technicians from the same hospital had attended the SAFE course, they reinforced good practice with each other.
“If I encounter something I am not sure about, I discuss with colleagues. We reviewed the SAFE training to consider the best plan in our setting. We help one another.”
Participants found that failure to include the whole operating room team in the training was a barrier to implementing practice change. Despite difficulties making changes in team practice, participants expressed determination to persist.
“From the SAFE course we made commitment to change but all of these changes were not implemented due to the fact that the whole team in theatre didn’t have the same understanding. For example, with the Surgical Safety Checklist because gynecologists and surgeons were not trained they did not see it as useful.”
“After the SAFE course I wanted to improve relations with the surgeons and harmonize. There has been resistance to change but I keep trying.”
Shortages of drugs, equipment, and human resources were consistently identified as barriers to practice change:
“Anesthesia has to also act as circulating nurse and must resuscitate the baby.”
“There were things I wanted to change in practice such as medications and monitoring and human resources. They say there is no budget.”
Interview participants felt the course was useful in improving their practice and in building relationships with colleagues:
“Due to the competencies and teamwork we learned in the SAFE course there have been no maternal deaths in the operating theatre since the course.”
“We had a chance to share that experience with people from all over the country and to exchange and discuss how to do difficult cases. It’s better to practice anesthesia with others.”
Sustaining knowledge on an ongoing basis is perhaps the most difficult step of the KTA cycle. To build on momentum developed in the first SAFE course, a second Rwandan course was run in November 2013 for a smaller group of 32 participants. In response to feedback from the first course about the need for team training, the second course included surgeons, nurses, midwives, and anesthesia technicians. Some of the “training-of-trainers” graduates and faculty from the first course taught during the second course to enhance confidence and capacity for future teaching. The SAFE courses are now being integrated into ongoing continuing professional development programs in Rwanda. The future vision is for smaller regionally based courses to be taught by local faculty. As much as possible, future courses will include nurses, midwives, and surgeons.
The SAFE course began the process of building professional relationships between anesthesia providers working in diverse geographic regions of Rwanda. The Rwandan Society of Anesthesiologists is planning to offer a countrywide annual meeting for anesthesia providers. This is an important next step for strengthening the APN and building a community of practice.
To date, the SAFE Obstetric Anesthesia course has been offered 20 times in eight countries. The Association of Anaesthetists of Great Britain and Ireland has developed “e-SAFE”, a web-based resource containing interactive e-learning and educational material from the SAFE course.20 The World Federation of Societies of Anaesthesiologists has offered financial support for SAFE courses and provides additional resources, such as the “Anaesthesia Tutorial of the Week”.21 These initiatives increase learning opportunities for anesthesia practitioners worldwide.
Conclusion
There are enormous challenges to providing anesthesia education in low-resource areas. These include a lack of anesthesia faculty members, relatively high costs, the need for travel, the limited ability of participants to obtain leave from work, poor facilities, and even poor notification of the opportunity to attend such courses. Assuming that all of those issues can be addressed, there remains the challenge of making the learning relevant to the participants so that they can, and will, make changes in their practice. The SAFE course participants were overwhelmingly enthusiastic about the value of this program and their desire for future training. In addition to improving their obstetric anesthesia knowledge and skills, participants appreciated collaboration with anesthesia practitioners from around Rwanda.
In follow-up interviews six months after the course, participants reported practice improvements – left lateral tilt, preoperative assessment, preparation for anesthesia, and systematic management of emergencies – and were more confident in speaking up for patient safety. They valued consultations with colleagues who had also attended the course. Based on participants’ recommendations to train the whole team, surgeons, nurses, and midwives were invited to join anesthesia technicians in the second Rwandan SAFE course. Future SAFE courses in Rwanda will continue to build teams to improve routine and emergent obstetrical care.
We applied the knowledge-to-action cycle for obstetric anesthesia knowledge translation in Rwanda. This model encouraged thoughtful consideration of the needs in Rwanda, curriculum modifications to suit the local context, active experiential learning, and building relationships to encourage changes in clinical practice. More than half of the anesthesia providers in Rwanda attended the SAFE course, and local anesthesia providers have been trained to run future courses. These clinicians have the potential to make a profound improvement in obstetric anesthesia care in Rwanda.
Notes
Grady K. Safer Anaesthesia From Education Obstetric Anesthesia Course (SAFE Course). Available from URL: http://www.aagbi.org/international/international-relations-committee/refresher-courses (accessed July 2014).
Obstetric Anaesthesia for Developing Countries. Clyburn P, Collis R, Harries S, editors. New York: Oxford University Press; 2010.
http://www.lifebox.org (accessed July 2014).
References
Ronsmans C, Graham WJ; Lancet Maternal Survival Series Steering Group. Maternal mortality: who, when, where, and why. Lancet 2006; 368: 1189-200.
World Health Organization. 10 Facts on Maternal Health 2013. Available from URL: http://www.who.int/features/factfiles/maternal_health/en/ (accessed July 2014).
Cooper GM, McClure JH. Anaesthesia chapter from Saving mothers’ lives; reviewing maternal deaths to make pregnancy safer. Br J Anaesth 2008; 100: 17-22.
Walker IA, Wilson IH. Anaesthesia in developing countries—a risk for patients. Lancet 2008; 371: 968-9.
Khan KS, Wojdyla D, Say L, Gulmezoglu AM, Van Look PF. WHO analysis of causes of maternal death: a systematic review. Lancet 2006; 367: 1066-74.
Fenton PM, Whitty CJ, Reynolds F. Caesarean section in Malawi: prospective study of early maternal and perinatal mortality. BMJ 2003; 327: 587.
Dyer RA, Reed AR, James MF. Obstetric anaesthesia in low-resource settings. Best Pract Res Clin Obstet Gynaecol 2010; 24: 401-12.
Enright A. Anesthesia training in Rwanda. Can J Anesth 2007; 54: 935-9.
The World Bank. Population (Total) 2013. Available from URL: http://data.worldbank.org/indicator/SP.POP.TOTL (accessed July 2014).
Notrica MR, Evans FM, Knowlton LM, Kelly McQueen KA. Rwandan surgical and anesthesia infrastructure: a survey of district hospitals. World J Surg 2011; 35: 1770-80.
Central Intelligence Agency. The World Factbook 2011. Available from URL: https://www.cia.gov/library/publications/the-world-factbook/fields/2054.html (accessed July 2014).
Petroze RT, Nzayisenga A, Rusanganwa V, Ntakiyiruta G, Calland JF. Comprehensive national analysis of emergency and essential surgical capacity in Rwanda. Br J Surg 2012; 99: 436-43.
World Health Organization. World Health Stastics 2013. Available from URL: http://www.who.int/gho/publications/world_health_statistics/EN_WHS2013_Full.pdf (accessed July 2014).
Ruhato P, Twugirumugabe T, Sami H. Quality assessment of the practice of obstetrical anaesthesia at Muhima District Hospital. Br J Anaesth 2012; 108(suppl 2): doi:10.1093/bja/aes070 (abstract).
Twagirumugabe T, Carli F. Rwandan anesthesia residency program: a model of north-south educational partnership. Int Anesthesiol Clin 2010; 48: 71-8.
Sargeant J, Borduas F, Sales A, Klein D, Lynn B, Stenerson H. CPD and KT: models used and opportunities for synergy. J Contin Educ Health Prof 2011; 31: 167-73.
Graham ID, Logan J, Harrison MB, et al. Lost in knowledge translation: time for a map? J Contin Educ Health Prof 2006; 26: 13-24.
World Health Organization. Surgical Safety Checklist, First Edition. Available from URL: http://www.who.int/patientsafety/safesurgery/tools_resources/SSSL_Checklist_finalJun08.pdf (accessed July 2014).
Creswell J. Research Design: Qualitative, Quantitative, and Mixed Methods Approaches. 3rd ed. Thousand Oaks, CA: Sage Publications; 2009 .
e-SAFE. Safer Anesthesia throught Education. Available from URL: http://www.e-safe-anaesthesia.org (accessed July 2014).
World Federation of Societies of Anaesthesiologists. Education and Training http://www.wfsahq.org/our-work/education-training (accessed July 2014).
Acknowledgements
We gratefully acknowledge the work of Dr. Iain Wilson and Dr. Kate Grady of the AAGBI. Dr. Wilson, immediate AAGBI Past President, developed the concept for the SAFE Obstetric Anesthesia course. Dr. Grady created and implemented the original SAFE Obstetric Anesthesia course curriculum and the follow-up program of logbooks and interviews.
Conflicts of interest
None declared.
Funding sources
Canadian Anesthesiologists’ Society International Education Foundation, the World Federation of Societies of Anaesthesiologists, Gradian Health Systems, and the Canadian International Development Agency (CIDA) Maternal Newborn and Child Health Program for Rwanda.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is accompanied by an editorial. Please see Can J Anesth 2014; 61: this issue.
Author contributions
See Appendix 2.
Appendices
Appendix 1
Checklist for Safe Anesthesia Practice for Cesarean Section

Appendix 2 Author contributions and disclosures
Author | Contribution | Disclosure |
|---|---|---|
Patricia Livingston Principal investigator | ∙ Study design ∙ SAFE course curriculum revisions ∙ SAFE course co-director and facilitator ∙ Data collection and analysis ∙ Manuscript writing and revisions ∙ Dr Livingston had access to all the data and takes full responsibility for the integrity of the data and accuracy of the data analysis. | Board of Directors, Canadian Anesthesiologists’ Society International Education Foundation (CAS IEF) |
Faye Evans | ∙ Study design ∙ SAFE course curriculum revisions ∙ SAFE course co-director and facilitator ∙ Manuscript revisions | None |
Etienne Nsereko | ∙ SAFE course facilitator ∙ Data collection and analysis | None |
Gaston Nyirigira | ∙ SAFE course facilitator ∙ Data collection and analysis | None |
Paulin Banguti Ruhato | ∙ SAFE course facilitator ∙ Data collection and analysis | None |
Joan Sargeant | ∙ Proposed knowledge-to-action cycle model for knowledge translation ∙ Study design | None |
Megan Chipp | ∙ SAFE course administration ∙ Data collection and analysis ∙ Manuscript revisions | None |
Angela Enright | ∙ SAFE course leadership and liaison with external partners (WFSA, AAGBI, Lifebox) | Board of Directors, Lifebox Foundation; |
∙ SAFE course facilitator ∙ Manuscript writing and revisions | Board of Directors, Canadian Anesthesiologists’ Society International Education Foundation (CAS IEF) |
Rights and permissions
About this article
Cite this article
Livingston, P., Evans, F., Nsereko, E. et al. Safer obstetric anesthesia through education and mentorship: a model for knowledge translation in Rwanda. Can J Anesth/J Can Anesth 61, 1028–1039 (2014). https://doi.org/10.1007/s12630-014-0224-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-014-0224-8