Abstract
Background
Regadenoson is a novel pharmacological stress agent whose disposition during hemodialysis is not known. The purpose of this study was to determine the clearance of regadenoson under varying dialytic conditions using an in vitro hemodialysis model.
Methods and Results
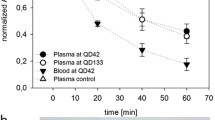
Whole human blood was used to analyze the effect of hemodialysis on the clearance of regadenoson. Regadenoson transmembrane clearance (CLD) was assessed for both a standard permeability and a high permeability polysulfone hemodialyzer with blood/dialysate flow rates of 300/600 and 400/800 mL/min. A two-tailed, paired Student’s t test was used to compare regadenoson CLD between hemodialyzer types and flow rates. The mean ± SD regadenoson CLD values ranged between 62.5 ± 11.8 and 89.1 ± 24.0 mL/min for all dialytic conditions. There was no significant difference in regadenoson CLD between hemodialyzer types and flow rates (p > .05).
Conclusions
Hemodialysis enhances the clearance of regadenoson independent of hemodialyzer permeability and blood/dialysate flow rate. This clearance is modest relative to total body clearance and is unlikely to produce a clinically significant outcome.

Similar content being viewed by others
Abbreviations
- CAD:
-
Coronary artery disease
- MPI:
-
Myocardial perfusion imaging
- SPECT:
-
Single-photon emission computed tomography
References
Miller TD, Askew JW, Anavekar NS. Noninvasive stress testing for coronary artery disease. Cardiol Clin 2014;32:387-404.
Lexiscan prescribing information handbook. Lexiscan (regadenoson) prescribing package insert. Northbrook, IL: Astellas Pharma; 2014.
Buhr C, Gössl M, Erbel R, Eggebrecht H. Regadenoson in the detection of coronary artery disease. Vasc Health Risk Manag 2008;4:337-40.
Ananthasubramaniam K, Weiss R, McNutt B, Klauke B, Feaheny K, Bukofzer S. A randomized, double-blind, placebo-controlled study of the safety and tolerance of regadenoson in subjects with stage 3 or 4 chronic kidney disease. J Nucl Cardiol 2012;19:319-29.
Farhad H, Murthy VL. Pharmacologic manipulation of coronary vascular physiology for the evaluation of coronary artery disease. Pharmacol Ther 2013;140:121-32.
Gordi T, Frohna P, Sun HL, Wolff A, Belardinelli L, Lieu H. A population pharmacokinetic/pharmacodynamic analysis of regadenoson, an adenosine A2A-receptor agonist, in healthy male volunteers. Clin Pharmacokinet 2006;45:1201-12.
Gordi T, Blackburn B, Lieu H. Regadenoson pharmacokinetics and tolerability in subjects with impaired renal function. J Clin Pharmacol 2007;47:825-33.
Sarnak MJ, Levey AS, Schoolwerth AC, Coresh J, Culleton B, Hamm LL, et al. Kidney disease as a risk factor for development of cardiovascular disease: A statement from the American Heart Association Councils on Kidney in Cardiovascular Disease, High Blood Pressure Research, Clinical Cardiology, and Epidemiology and Prevention. Circulation 2003;108:2154-69.
United States Renal Data System. USRDS annual data report: Epidemiology of kidney disease in the United States. Bethesda: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2015. p. 49-54.
Lentine KL, Costa SP, Weir MR, Robb JF, Fleisher LA, Kasiske BL, et al. Cardiac disease evaluation and management among kidney and liver transplantation candidates: A scientific statement from the American Heart Association and the American College of Cardiology Foundation. J Am Coll Cardiol 2012;60:434-80.
Venkataraman R, Hage FG, Dorfman T, Heo J, Agel RA, de Mattos AM, et al. Role of myocardial perfusion imaging in patients with end-stage renal disease undergoing coronary angiography. Am J Cardiol 2008;102:1451-6.
Doukky R, Fughhi I, Campagnoli T, Wassouf M, Ali A. The prognostic value of regadenoson SPECT myocardial perfusion imaging in patients with end-stage renal disease. J Nucl Cardiol 2015. doi:10.1007/s12350-015-0303-4.
AlJaroudi W, Hermann D, Hage F, Heo J, Iskandrian AE. Safety of regadenoson in patients with end-stage renal disease. Am J Cardiol 2010;105:133-5.
AlJaroudi W, Campagnoli T, Fughhi I, Wassouf M, Ali A, Doukky R. Prognostic value of heart rate response during regadenoson stress myocardial perfusion imaging in patients with end stage renal disease. J Nucl Cardiol 2016;23:560-9.
Doukky R, Rangel MO, Wassouf M, Dick R, Alqaid A, Morales Demori R. The safety and tolerability of regadenoson in patients with end-stage renal disease: The first prospective evaluation. J Nucl Cardiol 2013;20:205-13.
Doukky R, Morales Demori R, Jain S, Kiriakos R, Mwansa V, Calvin JE. Attenuation of the side effect profile of regadenoson: A randomized double-blinded placebo-controlled study with aminophylline in patients undergoing myocardial perfusion imaging “The ASSUAGE trial”. J Nucl Cardiol 2012;19:448-57.
Doukky R, Rangel MO, Dick R, Wassouf M, Alqaid A, Marget B. Attenuation of the side effect profile of regadenoson: A randomized double-blind placebo-controlled study with aminophylline in patients undergoing myocardial perfusion imaging and have severe chronic kidney disease—the ASSUAGE-CKD trial. Int J Cardiovasc Imaging 2013;29:1029-37.
Fresenius Medical Care. Dialysers and filters product range. Waltham, MA: Fresenius Medical Care; 2007.
Fresenius Medical Care. Fresenius optiflux dialyzers. Waltham, MA: Fresenius Medical Care; 2011.
Palani G, Husain Z, Salinas RC, Karthikeyan V, Karthikeyan AS, Ananthasubramaniam K. Safety of regadenoson as a pharmacologic stress agent for myocardial perfusion imaging in chronic kidney disease patients not on hemodialysis. J Nucl Cardiol 2011;18:605-11.
Levy G. Pharmacokinetics in renal disease. Am J Med 1977;62:461-5.
Tattersall JE, Chamney P, Aldridge C, Greenwood RN. Recirculation and the post-dialysis rebound. Nephrol Dial Transplant. 1996;11:75-80.
Hsi DH, Marreddy R, Moshiyakhov M, Luft U. Regadenoson induced acute ST-segment elevation myocardial infarction and multivessel coronary thrombosis. J Nucl Cardiol 2013;20:481-4.
Andrikopoulou E, Lloyd SG, Hage FG. Ventricular tachycardia during regadenoson SPECT myocardial perfusion imaging. J Nucl Cardiol 2015. doi:10.1007/s12350-015-0339-5.
Rai M, Ahlberg AW, Marwell J, Chaudhary W, Savino JA 3rd, Alter EL, et al. Safety of vasodilator stress myocardial perfusion imaging in patients with elevated cardiac biomarkers. J Nucl Cardiol 2016. doi:10.1007/s12350-016-0448-9.
Johnson NP, Gould KL. Physiological basis for angina and ST-segment change PET-verified thresholds of quantitative stress myocardial perfusion and coronary flow reserve. JACC Cardiovasc Imaging 2011;4:990-8.
Naya M, Murthy VL, Taqueti VR, Foster CR, Klein J, Garber M, et al. Preserved coronary flow reserve effectively excludes high-risk coronary artery disease on angiography. J Nucl Med 2014;55:248-55.
Rangel MO, Morales Demori R, Voll ST, Wassouf M, Dick R, Doukky R. Severe chronic kidney disease as a predictor of benefit from aminophylline administration in patients undergoing regadenoson stress myocardial perfusion imaging: A substudy of the ASSUAGE and ASSUAGE-CKD trials. J Nucl Cardiol 2015;22:1008-18.
Stevenson JM, Patel JH, Churchwell MD, Vilay AM, DePestel DD, Sörgel F, et al. Ertapenem clearance during modeled continuous renal replacement therapy. Int J Artif Organs 2008;31:1027-34.
Eyler RF, Vilay AM, Nader AM, Heung M, Pleva M, Sowinski KM, et al. Pharmacokinetics of ertapenem in critically ill patients receiving continuous venovenous hemodialysis or hemodiafiltration. Antimicrob Agents Chemother 2014;58:1320-6.
Churchwell MD, Pasko DA, Mueller BA. Daptomycin clearance during modeled continuous renal replacement therapy. Blood Purif 2006;24:548-54.
Vilay AM, Grio M, DePestel DD, Sowinski KM, Gao L, Heung M, et al. Daptomycin pharmacokinetics in critically ill patients receiving continuous venovenous hemodialysis. Crit Care Med 2011;39:19-25.
Acknowledgments
Dr Katherine Gharibian was an employee of the University of Michigan College of Pharmacy at the time this study was conducted. The authors would like to acknowledge the contributions of Weerachai Chaijamorn and Alexander Shaw in the conduct of this study.
Disclosure
The authors have no conflicts of interest to report.
Funding
This study was sponsored by Astellas Pharma Global Development, Inc.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gharibian, K.N., Murthy, V.L. & Mueller, B.A. Influence of hemodialysis on regadenoson clearance in an in vitro hemodialysis model. J. Nucl. Cardiol. 25, 234–239 (2018). https://doi.org/10.1007/s12350-016-0667-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-016-0667-0