Abstract
Introduction
Diabetes-related healthcare costs are increasing in the United States, with inpatient hospitalization the largest component of medical expenditures. The aims of this study were to characterize hospitalized type 2 diabetes mellitus (T2DM) patients, understand the relationship between hospitalization and healthcare costs, and explore treatment modification after inpatient hospitalization.
Methods
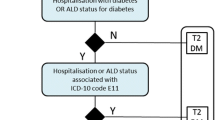
A retrospective cohort analysis of Humana Medicare Advantage and commercial members with T2DM was conducted. T2DM members were identified and assigned to three groups: (1) inpatient hospitalization (IPH) without a 30-day readmit (IPH group); (2) IPH with a 30-day readmission (IPH readmission group); and, (3) matched non-IPH group. Demographics, clinical characteristics, comorbidities and healthcare costs were measured based on enrollment data and claims. Descriptive statistics were used and the relationship between IPH and costs was assessed using generalized linear models.
Results
A total of 15,555 IPH patients, 1757 IPH readmission patients, and 17,312 matched non-IPH patients were included in the study. The IPH readmission group had the highest adjusted mean all-cause total costs ($76,806), followed by the IPH group ($42,011), and the non-IPH group ($9624). A similar trend was observed for adjusted all-cause mean medical and pharmacy costs. DM-related total healthcare costs were highest for the IPH readmission group ($13,714), followed by the IPH group ($7477), and non-IPH group ($1620). While overall therapy modification (discontinuation, addition, switch) was low, T2DM patients with an IPH (with or without a readmission) had greater rates of therapy modification relative to the non-IPH patients.
Conclusion
Adjusted all-cause and DM-related total costs were greatest for IPH readmission patients. Rates of treatment modification within 10 days of discharge after IPH were generally low. Identifying T2DM patients at high risk of readmission and employing methods to decrease that risk during the index hospitalization could have a significant impact on health system costs.
Funding
Novo Nordisk.

Similar content being viewed by others
References
American Diabetes Association. Economic costs of diabetes in the US in 2012. Diabetes Care. 2013;36(4):1033–46.
Alberti KGMM, Zimmet PF. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus. Provisional report of a WHO consultation. Diabet Med. 1998;15(7):539–53.
Moss SE, Klein R, Klein BE. Risk factors for hospitalization in people with diabetes. Arch Intern Med. 1999;159:2053–7.
Menzin J, Langley-Hawthorne C, Friedman M, Boulanger L, Cavanaugh R. Potential short-term economic benefits of improved glycemic control a managed care perspective. Diabetes Care. 2001;24(1):51–5.
Bergenstal RM, Fahrbach JL, Iorga SR, Fan Y, Foster SA. Preadmission glycemic control and changes to diabetes mellitus treatment regimen after hospitalization. Endocr Pract. 2012;18(3):371–5.
Wexler DJ, Beauharnais CC, Regan S, Nathan DM, Cagliero E, Larkin ME. Impact of inpatient diabetes management, education, and improved discharge transition on glycemic control 12 months after discharge. Diabetes Res Clin Pract. 2012;98(2):249–56.
Roman SH, Chassin MR. Windows of opportunity to improve diabetes care when patients with diabetes are hospitalized for other conditions. Diabetes Care. 2001;24(8):1371–6.
Braithwaite SS, Magee M, Sharretts JM, Schnipper JL, Amin A, Maynard G. The case for supporting inpatient glycemic control programs now: the evidence and beyond. J Hosp Med. 2008;3(S5):6–16.
Hart LG, Larson EH, Lishner DM. Rural definitions for health policy and research. Am J Public Health. 2005;95(7):1149.
Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45(6):613–9.
Chang H-Y, Weiner JP, Richards TM, Bleich SN, Segal JB. Validating the adapted Diabetes Complications Severity Index in claims data. Am J Manag Care. 2012;18(11):721–6.
Cook CB, Seifert KM, Hull BP, Hovan MJ, Charles JC, Miller-Cage V, et al. Inpatient to outpatient transfer of diabetes care: planing for an effective hospital discharge. Endocr Pract Off J Am Coll Endocrinol Am Assoc Clin Endocrinol. 2009;15(3):263–9.
Dungan KM. The effect of diabetes on hospital readmissions. J Diabetes Sci Technol. 2012;6(5):1045–52.
Draznin B, Gilden J, Golden SH, Inzucchi SE, Baldwin D, Bode BW, et al. Pathways to quality inpatient management of hyperglycemia and diabetes: a call to action. Diabetes Care. 2013;36(7):1807–14.
Jiang HJ, Stryer D, Friedman B, Andrews R. Multiple hospitalizations for patients with diabetes. Diabetes Care. 2003;26(5):1421–6.
Robbins JM, Webb DA. Diagnosing diabetes and preventing rehospitalizations: the urban diabetes study. Med Care. 2006;44(3):292–6.
Kim H, Ross JS, Melkus GD, Zhao Z, Boockvar K. Scheduled and unscheduled hospital readmissions among patients with diabetes. Am J Manag Care. 2010;16(10):760–7.
Burke RE, Coleman EA. Interventions to decrease hospital readmissions: keys for cost-effectiveness. JAMA Intern Med. 2013;173(8):695–8.
Z-Q Ma, Fisher MA. Characteristics driving higher diabetes-related hospitalization charges in Pennsylvania. Am J Manag Care. 2014;20(9):e408–17.
Eby E, Hardwick C, Yu M, Gelwicks S, Deschamps K, Xie J, et al. Predictors of 30 day hospital readmission in patients with type 2 diabetes: a retrospective, case–control, database study. Curr Med Res Opin. 2015;31(1):107–14. doi:10.1185/03007995.2014.981632 (Epub 2014 Nov 6).
Fallis BA, Dhalla IA, Klemensberg J, Bell CM. Primary medication non-adherence after discharge from a general internal medicine service. PLoS ONE. 2013;8(5):e61735.
Acknowledgments
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval to the version to be published. Editorial assistance in the preparation of this manuscript was provided by Donald Herdt, Eleanor Caplan and Mary Costantino, and funded by Comprehensive Health Insights. Comprehensive Health Insights was compensated in connection with development of this manuscript, and this support was funded by Novo Nordisk. The information contained in this manuscript was presented as a poster at the International Society for Pharmacoeconomics and Outcomes Research meeting in 2014.
Funding
Sponsorship and article processing charges for this study were funded by Novo Nordisk.
Conflict of interest
Vishal Saundankar, Jeffrey Ellis, Chad Moretz, and Brandon Suehs are employees of Comprehensive Health Insights, Inc. Yunus Meah is an employee of Humana, Inc. Elsie Allen, Tony DeLuzio, and Jonathan Bouchard are employees of Novo Nordisk.
Compliance with ethics guidelines
The analysis reported in this article was based on administrative and clinical data collected during the standard course of care, and does not involve any new studies of human or animal subjects performed by any of the authors. Prior to initiation, the study protocol was reviewed and approved by Schulman Associates Institutional Review Board.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Appendix
Rights and permissions
About this article
Cite this article
Saundankar, V., Ellis, J., Allen, E. et al. Type 2 Diabetes Mellitus Patients’ Healthcare Costs Related to Inpatient Hospitalizations: A Retrospective Administrative Claims Database Study. Adv Ther 32, 662–679 (2015). https://doi.org/10.1007/s12325-015-0223-3
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-015-0223-3