Abstract
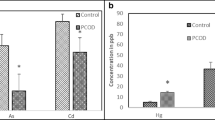
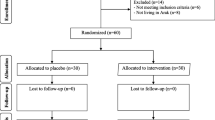
Polycystic ovarian syndrome is one of the most common hormonally leading cause infertility disorders. The effect of oxidant-antioxidant imbalance on disease progression has been studied in many disorders. The present study was aimed to evaluate prooxidant–antioxidant balance (PAB) in patients with polycystic ovarian syndrome compared to healthy subjects. We also studied the possible effect of treatment with available drugs on serum PAB. In this case–control study 100 polycystic ovary syndrome (PCOS) patients and 100 healthy individuals were enrolled in the study. The laboratory features of patients and controls like as serum LH and FSH concentration and hematological examinations were collected. PAB was evaluated by a colorimetric method. Serum PAB value was significantly higher before treatment compared to after treatment and healthy subjects. PAB values were also higher in subjects with irregular menstrual cycle compared to normal subjects. Our results represented that serum PAB values has an indirect significant correlation with serum LH concentration. We also found that drugs regimen containing spironolactone effectively reduced the serum PAB values. Our results showed that PCOS patients had increased level of PAB and treatment with spironolactone mainly decreases the level of serum PAB. Our results indicate that the measurements of PAB may be used as a potential laboratory marker for assessment of PCOS patients.

Similar content being viewed by others
References
Norman RJ, Dewailly D, Legro RS, Hickey TE. Polycystic ovary syndrome. Lancet. 2007;370(9588):685–97. doi:10.1016/S0140-6736(07)61345-2.
March WA, Moore VM, Willson KJ, Phillips DI, Norman RJ, Davies MJ. The prevalence of polycystic ovary syndrome in a community sample assessed under contrasting diagnostic criteria. Hum Reprod. 2010;25(2):544–51. doi:10.1093/humrep/dep399.
Alvarez-Blasco F, Botella-Carretero JI, San Millan JL, Escobar-Morreale HF. Prevalence and characteristics of the polycystic ovary syndrome in overweight and obese women. Arch Intern Med. 2006;166(19):2081–6. doi:10.1001/archinte.166.19.2081.
Kuscu NK, Var A. Oxidative stress but not endothelial dysfunction exists in non-obese, young group of patients with polycystic ovary syndrome. Acta Obstet Gynecol Scand. 2009;88(5):612–7. doi:10.1080/00016340902859315.
Escobar-Morreale HF, San Millan JL. Abdominal adiposity and the polycystic ovary syndrome. Trends Endocrinol Metab. 2007;18(7):266–72. doi:10.1016/j.tem.2007.07.003.
San Millan JL, Alvarez-Blasco F, Luque-Ramirez M, Botella-Carretero JI, Escobar-Morreale HF. The PON1-108C/T polymorphism, and not the polycystic ovary syndrome, is an important determinant of reduced serum paraoxonase activity in premenopausal women. Hum Reprod. 2006;21(12):3157–61. doi:10.1093/humrep/del300.
Kadowaki T, Yamauchi T. Adiponectin and adiponectin receptors. Endocr Rev. 2005;26(3):439–51. doi:10.1210/er.2005-0005.
Escobar-Morreale HF, Villuendas G, Botella-Carretero JI, Alvarez-Blasco F, Sanchon R, Luque-Ramirez M, et al. Adiponectin and resistin in PCOS: a clinical, biochemical and molecular genetic study. Hum Reprod. 2006;21(9):2257–65. doi:10.1093/humrep/del146.
Gonzalez F, Chang L, Horab T, Lobo RA. Evidence for heterogeneous etiologies of adrenal dysfunction in polycystic ovary syndrome. Fertil Steril. 1996;66(3):354–61.
Fernandez-Real JM, Broch M, Vendrell J, Ricart W. Insulin resistance, inflammation, and serum fatty acid composition. Diabetes Care. 2003;26(5):1362–8.
Fenkci V, Fenkci S, Yilmazer M, Serteser M. Decreased total antioxidant status and increased oxidative stress in women with polycystic ovary syndrome may contribute to the risk of cardiovascular disease. Fertil Steril. 2003;80(1):123–7. doi:10.1016/S0015-0282(03)00571-5.
Gonzalez F, Rote NS, Minium J, Kirwan JP. Reactive oxygen species-induced oxidative stress in the development of insulin resistance and hyperandrogenism in polycystic ovary syndrome. J Clin Endocrinol Metab. 2006;91(1):336–40. doi:10.1210/jc.2005-1696.
Ndefo UA, Eaton A, Green MR. Polycystic ovary syndrome: a review of treatment options with a focus on pharmacological approaches. Pharm Ther. 2013;38(6):336–55.
Escobar-Morreale HF, Luque-Ramirez M, San Millan JL. The molecular-genetic basis of functional hyperandrogenism and the polycystic ovary syndrome. Endocr Rev. 2005;26(2):251–82. doi:10.1210/er.2004-0004.
Turrens JF. Mitochondrial formation of reactive oxygen species. J Physiol. 2003;552(Pt 2):335–44. doi:10.1113/jphysiol.2003.049478.
Lee JY, Baw C, Gupta S, Aziz N, Agarwal A. Role of oxidative stress in polycystic ovary syndrome. Curr Women’s Health Rev. 2010;6(2):96–107. doi:10.2174/157340410791321336.
Gupta S, Malhotra N, Sharma D, Chandra A, Ashok A. Oxidative stress and its role in female infertility and assisted reproduction: clinical implications. Int J Fertil Steril. 2009;2(4):147–64.
Agarwal A, Aponte-Mellado A, Premkumar BJ, Shaman A, Gupta S. The effects of oxidative stress on female reproduction: a review. Reprod Biol Endocrinol. 2012;10:49. doi:10.1186/1477-7827-10-49.
Agarwal A, Gupta S, Sharma R. Oxidative stress and its implications in female infertility—a clinician’s perspective. Reprod Biomed Online. 2005;11(5):641–50.
Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group. Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome. Fertil Steril. 2004;81(1):19–25. doi:10.1016/j.fertnstert.2003.10.004.
Ferriman D, Gallwey JD. Clinical assessment of body hair growth in women. J Clin Endocrinol Metab. 1961;21:1440–7. doi:10.1210/jcem-21-11-1440.
Ludwig E. Classification of the types of androgenetic alopecia (common baldness) occurring in the female sex. Br J Dermatol. 1977;97(3):247–54.
Alamdari DH, Paletas K, Pegiou T, Sarigianni M, Befani C, Koliakos G. A novel assay for the evaluation of the prooxidant–antioxidant balance, before and after antioxidant vitamin administration in type II diabetes patients. Clin Biochem. 2007;40(3–4):248–54. doi:10.1016/j.clinbiochem.2006.10.017.
Tavana S, Amini S, Hakhamaneshi MS, Andalibi P, Hajir MS, Ardalan A, et al. Prooxidant–antioxidant balance in patients with phenylketonuria and its correlation to biochemical and hematological parameters. J Pediatr Endocrinol Metab. 2016;. doi:10.1515/jpem-2015-0398.
Palacio JR, Iborra A, Ulcova-Gallova Z, Badia R, Martinez P. The presence of antibodies to oxidative modified proteins in serum from polycystic ovary syndrome patients. Clin Exp Immunol. 2006;144(2):217–22. doi:10.1111/j.1365-2249.2006.03061.x.
Sabuncu T, Vural H, Harma M. Oxidative stress in polycystic ovary syndrome and its contribution to the risk of cardiovascular disease. Clin Biochem. 2001;34(5):407–13. doi:10.1016/S0009-9120(01)00245-4.
Zhang D, Luo WY, Liao H, Wang CF, Sun Y. The effects of oxidative stress to PCOS. Sichuan Da Xue Xue Bao Yi Xue Ban. 2008;39(3):421–3.
Karadeniz M, Erdogan M, Tamsel S, Zengi A, Alper GE, Caglayan O, et al. Oxidative stress markers in young patients with polycystic ovary syndrome, the relationship between insulin resistances. Exp Clin Endocrinol Diabetes. 2008;116(4):231–5. doi:10.1055/s-2007-992154.
Dursun P, Demirtas E, Bayrak A, Yarali H. Decreased serum paraoxonase 1 (PON1) activity: an additional risk factor for atherosclerotic heart disease in patients with PCOS? Hum Reprod. 2006;21(1):104–8. doi:10.1093/humrep/dei284.
Fenkci IV, Serteser M, Fenkci S, Kose S. Paraoxonase levels in women with polycystic ovary syndrome. J Reprod Med. 2007;52(10):879–83.
Nacul AP, Andrade CD, Schwarz P, de Bittencourt PI Jr., Spritzer PM. Nitric oxide and fibrinogen in polycystic ovary syndrome: associations with insulin resistance and obesity. Eur J Obstet Gynecol Reprod Biol. 2007;133(2):191–6. doi:10.1016/j.ejogrb.2006.09.009.
Daneasa A, Cucolas C, Furcea M, Bolfa P, Dudea S, Olteanu D, et al. Spironolactone and dimethylsulfoxide effect on glucose metabolism and oxidative stress markers in polycystic ovarian syndrome rat model. Exp Clin Endocrinol Diabetes. 2014;122(3):154–62. doi:10.1055/s-0033-1363685.
Virdis A, Neves MF, Amiri F, Viel E, Touyz RM, Schiffrin EL. Spironolactone improves angiotensin-induced vascular changes and oxidative stress. Hypertension. 2002;40(4):504–10.
Renke M, Tylicki L, Knap N, Rutkowski P, Neuwelt A, Larczynski W, et al. Spironolactone attenuates oxidative stress in patients with chronic kidney disease. Hypertension. 2008;52(5):e132–3. doi:10.1161/HYPERTENSIONAHA.108.120568 (author reply e4).
Queisser N, Happ K, Link S, Jahn D, Zimnol A, Geier A, et al. Aldosterone induces fibrosis, oxidative stress and DNA damage in livers of male rats independent of blood pressure changes. Toxicol Appl Pharmacol. 2014;280(3):399–407. doi:10.1016/j.taap.2014.08.029.
Pincemail J, Vanbelle S, Gaspard U, Collette G, Haleng J, Cheramy-Bien JP, et al. Effect of different contraceptive methods on the oxidative stress status in women aged 40 48 years from the ELAN study in the province of Liege, Belgium. Hum Reprod. 2007;22(8):2335–43. doi:10.1093/humrep/dem146.
Finco A, Belcaro G, Cesarone MR. Assessment of the activity of an oral contraceptive on the levels of oxidative stress and changes in oxidative stress after co-treatment with two different types of physiological modulators with antioxidant action. Contraception. 2011;84(4):418–22. doi:10.1016/j.contraception.2011.02.008.
Durand P, Blache D. Enhanced platelet thromboxane synthesis and reduced macrophage-dependent fibrinolytic activity related to oxidative stress in oral contraceptive-treated female rats. Atherosclerosis. 1996;121(2):205–16. doi:10.1016/0021-9150(95)05720-X.
Cai J, Cao S, Chen J, Yan F, Chen G, Dai Y. Progesterone alleviates acute brain injury via reducing apoptosis and oxidative stress in a rat experimental subarachnoid hemorrhage model. Neurosci Lett. 2015;600:238–43. doi:10.1016/j.neulet.2015.06.023.
Aksoy AN, Toker A, Celik M, Aksoy M, Halici Z, Aksoy H. The effect of progesterone on systemic inflammation and oxidative stress in the rat model of sepsis. Indian J Pharmacol. 2014;46(6):622–6. doi:10.4103/0253-7613.144922.
Ghanem H, Shaeer O, El-Segini A. Combination clomiphene citrate and antioxidant therapy for idiopathic male infertility: a randomized controlled trial. Fertil Steril. 2010;93(7):2232–5. doi:10.1016/j.fertnstert.2009.01.117.
Hayon T, Dvilansky A, Oriev L, Nathan I. Non-steroidal antiestrogens induce apoptosis in HL60 and MOLT3 leukemic cells; involvement of reactive oxygen radicals and protein kinase C. Anticancer Res. 1999;19(3A):2089–93.
Anedda A, Rial E, Gonzalez-Barroso MM. Metformin induces oxidative stress in white adipocytes and raises uncoupling protein 2 levels. J Endocrinol. 2008;199(1):33–40. doi:10.1677/JOE-08-0278.
Chakraborty A, Chowdhury S, Bhattacharyya M. Effect of metformin on oxidative stress, nitrosative stress and inflammatory biomarkers in type 2 diabetes patients. Diabetes Res Clin Pract. 2011;93(1):56–62. doi:10.1016/j.diabres.2010.11.030.
Yilmaz M, Bukan N, Ayvaz G, Karakoc A, Toruner F, Cakir N, et al. The effects of rosiglitazone and metformin on oxidative stress and homocysteine levels in lean patients with polycystic ovary syndrome. Hum Reprod. 2005;20(12):3333–40. doi:10.1093/humrep/dei258.
Kocer D, Bayram F, Diri H. The effects of metformin on endothelial dysfunction, lipid metabolism and oxidative stress in women with polycystic ovary syndrome. Gynecol Endocrinol. 2014;30(5):367–71. doi:10.3109/09513590.2014.887063.
Acknowledgments
The authors wish to thank all patients and health stuffs who participated in this study. This work has no financially support.
Author Contribution
N. Heshmati: Data collection; S. Shahgheibi: Project development, manuscript editing; B. Nikkhoo: Data collection; S. Amini: Project development; M. Abdi: Project development data management, data analysis, manuscript writing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Rights and permissions
About this article
Cite this article
Heshmati, N., Shahgheibi, S., Nikkhoo, B. et al. Association of Prooxidant–Antioxidant Balance with Clinical and Laboratory Parameters and Its Relation to Different Drug Regimens in Polycystic Ovary Syndrome Women with Normal BMI. Ind J Clin Biochem 32, 315–322 (2017). https://doi.org/10.1007/s12291-016-0613-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12291-016-0613-6