Abstract
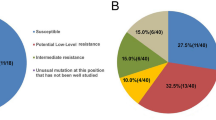
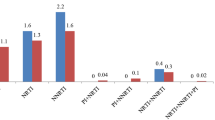
Little is known about the prevalence of drug-resistant mutations in HIV-1-positive individuals in Suzhou, China. To elucidate the transmitted drug resistance (TDR) and acquired drug resistance mutation (ADR) profiles, we collected blood specimens from 127 drug-naïve and 117 first-line drug-treated HIV-1-infected individuals sampled from 2014 to 2016 in Suzhou. We successfully amplified pol fragments from 100 drug-naïve and 20 drug-treated samples. We then determined the drug-resistant mutations to protease (PR) and reverse-transcriptase (RT) inhibitors according to the Stanford drug resistance database. Overall, 11 and 13 individuals had transmitted (drug-naïve group) and acquired (treated group) resistance mutations, respectively. Six transmitted drug-resistant mutations were found, including two mutations (L33F and L76V) in the protease region and four (K70N/E and V179D/E) in the RT region. Only L76V was a major mutation, and K70N/E and V179D/E are known to cause low-level resistance to RT inhibitors. All 13 treated participants who had major drug resistance mutations demonstrated intermediate to high resistance to efavirenz and nevirapine, and six had a treatment duration of less than three months. No major mutations to RT inhibitors were found, implying that the epidemic of transmitted resistance mutations was not significant in this area. Our results suggest that more frequent virus load and drug resistance mutation tests should be conducted for individuals receiving antiretroviral treatment, especially for newly treated patients. Our research provides insights into the occurrence of HIV-1 drug resistance in Suzhou and will help to optimize the treatment strategy for this population.

Similar content being viewed by others
References
Barbour JD, Hecht FM, Wrin T, Liegler TJ, Ramstead CA, Busch MP, Segal MR, Petropoulos CJ, Grant RM. 2004. Persistence of primary drug resistance among recently HIV-1 infected adults. AIDS, 18: 1683–1689.
Boyd MA, Cooper DA. 2007. Second-line combination antiretroviral therapy in resource-limited settings: facing the challenges through clinical research. AIDS, 21(Suppl 4): S55–S63.
Chen X, Ye M, Zhou YH, Liu FL, Duo L, Li H, Pang W, Zheng YT. 2015. High seroprevalence of toxoplasma gondii and HIV-1 co-infection among drug users in Yunnan province, southwest China. Sci China Life Sci, 59: 857–859.
Cohen MS, Chen YQ, McCauley M, Gamble T, Hosseinipour MC, Kumarasamy N, Hakim JG, Kumwenda J, Grinsztejn B, Pilotto JH, Godbole SV, Chariyalertsak S, Santos BR, Mayer KH, Hoffman IF, Eshleman SH, Piwowar-Manning E, Cottle L, Zhang XC, Makhema J, Mills LA, Panchia R, Faesen S, Eron J, Gallant J, Havlir D, Swindells S, Elharrar V, Burns D, Taha TE, Nielsen-Saines K, Celentano DD, Essex M, Hudelson SE, Redd AD, Fleming TR. 2016. Antiretroviral Therapy for the Prevention of HIV-1 Transmission. N Engl J Med, 375: 830–839.
Cohen MS, Smith MK, Muessig KE, Hallett TB, Powers KA, Kashuba AD. 2013. Antiretroviral treatment of HIV-1 prevents transmission of HIV-1: where do we go from here?. Lancet, 382: 1515–1524.
D’Aquila RT, Johnson VA, Welles SL, Japour AJ, Kuritzkes DR, DeGruttola V, Reichelderfer PS, Coombs RW, Crumpacker CS, Kahn JO, Richman DD. 1995. Zidovudine resistance and HIV-1 disease progression during antiretroviral therapy. AIDS Clinical Trials Group Protocol 116B/117 Team and the Virology Committee Resistance Working Group. Ann Intern Med, 122: 401–408.
Guo H, Xu X, Hu H, Zhou Y, Yang H, Qiu T, Fu G, Huan X. 2015. Low prevalence of the transmitted HIV-1 drug resistance among newly diagnosed HIV-1 individuals in Jiangsu Province, China during 2009–2011. BMC Public Health, 15: 120.
Gupta RK, Jordan MR, Sultan BJ, Hill A, Davis DH, Gregson J, Sawyer AW, Hamers RL, Ndembi N, Pillay D, Bertagnolio S. 2012. Global trends in antiretroviral resistance in treatmentnaive individuals with HIV after rollout of antiretroviral treatment in resource-limited settings: a global collaborative study and meta-regression analysis. Lancet, 380: 1250–1258.
Hall TA. 1999. BioEdit: a user-friendly biological sequence alignment editor and analysis program for Windows 95/98/NT. Nucl Acids SympSer 1999, 41: 95–98.
Han X, Zhang M, Dai D, Wang Y, Zhang Z, Liu J, Geng W, Jiang Y, Takebe Y, Shang H. 2007. Genotypic resistance mutations to antiretroviral drugs in treatment-naive HIV/AIDS patients living in Liaoning Province, China: baseline prevalence and subtype-specific difference. AIDS Res Hum Retroviruses, 23: 357–364.
Huang X. 1992. A contig assembly program based on sensitive detection of fragment overlaps. Genomics, 14: 18–25.
Li H, Chang S, Han Y, Zhuang D, Li L, Liu Y, Liu S, Bao Z, Zhang W, Song H, Li T, Li J. 2016. The prevalence of drug resistance among treatment-naive HIV-1-infected individuals in China during pre-and post- 2004. BMC Infect Dis, 16: 605.
Li J, Li L, Yang S, Li J, Zhang M, Yang C, Liu J, Li H. 2016. Identification and characterization of two human immunodeficiency virus type 1 unique recombinant forms from Yunnan, China. Virol Sin, 31: 184–187.
Li L, Sun B, Zeng H, Sun Z, Sun G, Yang R. 2014. Relatively high prevalence of drug resistance among antiretroviral-naive patients from Henan, Central China. AIDS Res Hum Retroviruses, 30: 160–164.
Liao L, Xing H, Shang H, Li J, Zhong P, Kang L, Cheng H, Si X, Jiang S, Li X, Shao Y. 2010. The prevalence of transmitted antiretroviral drug resistance in treatment-naive HIV-infected indi-viduals in China. J Acquir Immune Defic Syndr, 53(Suppl 1): S10–S14.
Lole KS, Bollinger RC, Paranjape RS, Gadkari D, Kulkarni SS, Novak NG, Ingersoll R, Sheppard HW, Ray SC. 1999. Fulllength human immunodeficiency virus type 1 genomes from subtype C-infected seroconverters in India, with evidence of intersubtype recombination. J Virol, 73: 152–160.
Mackie NE, Dunn DT, Dolling D, Garvey L, Harrison L, Fearnhill E, Tilston P, Sabin C, Geretti AM. 2013. The impact of HIV-1 reverse transcriptase polymorphisms on responses to first-line nonnucleoside reverse transcriptase inhibitor-based therapy in HIV-1-infected adults. Aids, 27: 2245–2253.
Chinese Center for Disease Control and Prevention (China CDC). 2016. Chinese National Free AIDS Antiretroviral Therapy Manual. (In Chinese)
Qiu T, Ding P, Liu X, Xu J, Guo H, Fu G, Xu X, Huan X. 2014. Epidemiological characteristics of HIV/AIDS patients newly received highly active antiretroviral therapy during 2005–2013 in Jiangsu province. Chin J Epidemiol, 35: 1320–1323. (In Chinese)
Rhee S-Y, Blanco JL, Jordan MR, Taylor J, Lemey P, Varghese V, Hamers RL, Bertagnolio S, de Wit TFR, Aghokeng AF, et al., 2015. Geographic and Temporal Trends in the Molecular Epidemiology and Genetic Mechanisms of Transmitted HIV-1 Drug Resistance: An Individual-Patient- and Sequence-Level Meta-Analysis. PLoS Med, 12: e1001810.
Richman DD, Havlir D, Corbeil J, Looney D, Ignacio C, Spector SA, Sullivan J, Cheeseman S, Barringer K, Pauletti D, et al. 1994. Nevirapine resistance mutations of human immunodeficiency virus type 1 selected during therapy. J Virol, 68: 1660–1666.
Gandhi RT, Wurcel A, Rosenberg ES, Johnston MN, Hellmann N, Bates M, Hirsch MS, Walker BD. 2003. Progressive reversion of human immunodeficiency virus type 1 resistance mutations in vivo after transmission of a multiply drug-resistant virus. Clin Infect Dis, 37: 1693–1698.
Little SJ, Frost SD, Wong JK, Smith DM, Pond SL, Ignacio CC, Parkin NT, Petropoulos CJ, Richman DD. 2008. Persistence of transmitted drug resistance among subjects with primary human. J Virol, 82: 5510–5518.
Stadeli KM, Richman DD. 2013. Rates of emergence of HIV drug resistance in resource-limited settings: a systematic review. Antivir Ther, 18: 115–123.
Tamura K, Stecher G, Peterson D, Filipski A, Kumar S. 2013. MEGA6: Molecular Evolutionary Genetics Analysis version 6.0. Mol Biol Evol, 30: 2725–2729.
Theys K, Deforche K, Vercauteren J, Libin P, van de Vijver DAMC, Albert J, Åsjö B, Balotta C, Bruckova M, Camacho RJ, et al., 2012. Treatment-associated polymorphisms in protease are significantly associated with higher viral load and lower CD4 count in newly diagnosed drug-naive HIV-1 infected patients. 9.
UNAIDS. 2015. 2015 China AIDS Response Progress Report. Available: http://www.unaids.org/sites/default/files/country/documents/CHN_narrative_report_2015.pdf
Wainberg MA, Brenner BG, Turner D. 2005. Changing patterns in the selection of viral mutations among patients receiving nucleoside and nucleotide drug combinations directed against human immunodeficiency virus type 1 reverse transcriptase. Antimicrob Agents Chemother, 49: 1671–1678.
Wang J, Wang Z, Liu J, Yue Y, Yang S, Huang H, He C, Liao L, Xing H, Ruan Y, Shao Y. 2015. Efficacy and HIV drug resistance profile of second-line ART among patients having received long-term first-line regimens in rural China. Sci Rep, 5: 14823.
Wittkop L, Günthard HF, de Wolf F, Dunn D, Cozzi-Lepri A, de Luca A, Kücherer C, Obel N, von Wyl V, Masquelier B, et al., 2011. Effect of transmitted drug resistance on virological and immunological response to initial combination antiretroviral therapy for HIV (EuroCoord-CHAIN joint project): a European multicohort study. The Lancet Infectious Diseases, 11: 363–371.
Ye JR, Lu HY, Wang WS, Guo L, Xin RL, Yu SQ, Wu TC, Zeng Y, He X. 2012. The prevalence of drug resistance mutations among treatment-naive HIV-infected individuals in Beijing, China. AIDS Res Hum Retroviruses, 28: 418–423.
Zeng H, Sun B, Li L, Li Y, Liu Y, Xiao Y, Jiang Y, Yang R. 2014. Reconstituting the epidemic history of mono lineage of HIV-1 CRF01_AE in Guizhou province, Southern China. Infection, Genetics and Evolution, 26: 139–145.
Zhang F, Haberer JE, Wang Y, Zhao Y, Ma Y, Zhao D, Yu L, Goosby EP. 2007. The Chinese free antiretroviral treatment program: challenges and responses. Aids, 21(Suppl 8): S143–S148.
Zhao B, Han X, Dai D, Liu J, Ding H, Xu J, Chu Z, Bice T, Diao Y, Shang H. 2011. New trends of primary drug resistance among HIV type 1-infected men who have sex with men in Liaoning Province, China. AIDS Res Hum Retroviruses, 27: 1047–1053.
Zhao B, Han X, Xu J, Hu Q, Chu Z, Zhang J, Lu L, Wang Z, Fu J, Chen X, Yan H, Zhuang M, Wang L, Sun A, Zhang CM, Shang H. 2015. Increase of RT-related transmitted drug resistance in non-CRF01_AE among HIV type 1-infected men who have sex with men in the 7 cities of China. J Acquir Immune Defic Syndr, 68: 250–255.
Zhou Y, Lu J, Wang J, Yan H, Li J, Xu X, Zhang Z, Qiu T, Ding P, Fu G, Huan X, Hu H. 2016. Prevalence of HIV Antiretroviral Drug Resistance and Its Impacts on HIV-1 Virological Failures in Jiangsu, China: A Cross-Sectional Study. BioMed Research International, 2016: 1752437.
Acknowledgments
This study was supported by grants from the Natural Science Foundation of Jiangsu Province (BL2013017) and the Suzhou Science and Technology Bureau (SYS201156) to Dr. Feng Qian, the Suzhou Health and Family Planning Commission (LCZX201413) to Ming Li, and the Key National Science and Technology Program in the Thirteen Five-Year Plan Period of China (2017ZX10201102-007-002).
Author information
Authors and Affiliations
Contributions
TL, FQ, TY, RY, YG, CZ and BS conceived the experiments; WX, LZ, JH, HW, YZ, YW, XL, SG, ZT, XL, WZ, PX, HC, WL and ML collected the samples; TL and YC performed the experiments; TL analyzed the data; TL, FQ and BS wrote and finalized the manuscript. All authors have read and approved the final manuscript.
Corresponding authors
Ethics declarations
The authors declare that there is no conflict of interest. The study was approved by the Ethics Committees of the Fifth People’s Hospital of Suzhou and Wuhan Institute of Virology. Informed consent was obtained from all participants in this study.
Electronic supplementary material
12250_2017_4002_MOESM1_ESM.pdf
Drug resistance mutation profiles of the drug-naïve and first-line regimen-treated HIV-1-infected population of Suzhou, China
Rights and permissions
About this article
Cite this article
Li, T., Qian, F., Yuan, T. et al. Drug resistance mutation profiles of the drug-naïve and first-line regimen-treated HIV-1-infected population of Suzhou, China. Virol. Sin. 32, 271–279 (2017). https://doi.org/10.1007/s12250-017-4002-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12250-017-4002-y