Abstract
Objectives
To compare extubation failure rate between the heated humidified high-flow nasal cannula (HHHFNC) and continuous positive airway pressure (CPAP) groups.
Methods
Intubated infants with gestational age (GA) <32 wk, who were ready to extubate, were randomized to receive respiratory support with either CPAP or HHHFNC after extubation. In CPAP group, nasal mask CPAP with preset pressure and fraction of inspired oxygen (FiO2) equal to positive end-expiratory pressure (PEEP) and FiO2 of ventilator before extubation was applied. In the HHHFNC group, predefined flow rate according to the protocol was applied. Primary outcome was extubation failure within 72 h after endotracheal tube removal.
Results
Forty-nine infants were enrolled; 24 in the HHHFNC and 25 in the CPAP group. Baseline demographic and respiratory conditions before extubation were similar. There was no difference in infants who met failed extubation criteria between the two groups [8 (33%) in HHHFNC vs. 6 (24%) in CPAP group (p = 0.47)]. However, 6 infants (75%) in HHHFNC and 4 infants (66%) in CPAP group who met failed extubation criteria could be rescued by bilevel CPAP. Therefore, the reintubation rate was comparable [2 infants (8.3%) in HHHFNC vs. 2 infants (8%) in CPAP group]. Morbidities or related complications were not different but infants in the HHHFNC group had significantly less nasal trauma (16.7% vs. 44%; p = 0.03).
Conclusions
In the index study, the extubation failure rate was not statistically different between infants who were on HHHFNC or CPAP support.
Similar content being viewed by others
Introduction
In the past, endotracheal intubation was the main respiratory support in preterm infants, but prolonged intubation can increase risks of infection, lung injury, and chronic lung disease. Therefore, the strategy has been shifted to initiate non-invasive respiratory support as soon as possible to minimize duration of mechanical ventilator.
Nasal continuous positive airway pressure (nasal CPAP) has been widely used as a non-invasive respiratory support for preterm infants [1]. It is not only used as a primary respiratory support but also used after extubation to prevent alveolar collapse. However, it also has some drawbacks such as nasal trauma, head deformity, gaseous bowel distension and the difficulty to maintain the device on infant’s face at all time to obtain the constant pressure [2]. Heated humidified high-flow nasal cannula (HHHFNC) therapy in preterm infants means the delivery of heated, humidified and blended oxygen or air flow at a flow rate of >1 L/min [3]. HHHFNC is now increasingly used as a CPAP substitute in many situations [4, 5]. The advantages of HHHFNC are its ease in usage, more comfortable for infants and less nasal trauma [6].
HHHFNC has been used as a respiratory support for various purposes including apnea of prematurity [7], primary respiratory support in respiratory distress syndrome (RDS) [8], CPAP weaning [9, 10] and post extubation. Previous studies found that HHHFNC is subordinate to CPAP in the aspect of increasing rate of reintubation and oxygen requirement [11]. However, recent randomized controlled studies illustrated the safety and efficacy of HHHFNC for prevention of extubation failure [12–14]. Even though these trials used different extubation protocols, all concluded that HHHFNC is as effective as or non-inferior to CPAP. Nonetheless, the latest systematic review states that the safety and efficacy of HHHFNC still needs further study, especially in extremely preterm subgroup [15]. Since there is contradictory evidence and different HHHFNC protocols after extubation, the authors, therefore, conducted a study to compare the efficacy between HHHFNC and CPAP for prevention of extubation failure.
Material and Methods
A randomized controlled study was conducted between December 2012 and Febuary 2014, at the Neonatal Intensive Care Unit, Faculty of Medicine Ramathibodi Hospital, Mahidol University, Bangkok, Thailand. Intubated preterm infants, gestational age (GA) of <32 wk or birth weight (BW) of <1500 g, who were ready to extubate were eligible. Infants were considered to be ready for extubation when the settings of ventilator were at peak inspiratory pressure (PIP) of ≤15 cm H2O, positive end-expiratory pressure (PEEP) of ≤6 cm H2O, fraction of inspired oxygen (FiO2) of ≤0.3 and intermittent mandatory rate of ≤20/min, and had an acceptable blood gas (pH ≥7.25, pCO2 ≤ 55) and hematocrit (Hct) of >30%. Before extubation, a loading dose of 8 mg/kg/dose aminophylline was given with a maintenance dose of 1.5 mg/kg/dose every 8–12 h. Exclusion criteria included infant’s body weight < 700 g at the time of enrollment, major congenital heart diseases, airway anomalies, lung hypoplasia, and neuromuscular disorders. The study was approved by the Institutional Review Board, and informed consent from parents or guardians was obtained before randomization. Enrolled infants were randomly assigned to receive HHHFNC or CPAP after extubation under block-of-four randomization stratified by GA (<28 wk, 28 to 30 wk and >30 wk). Concealed, opaque envelopes with the computer generated sequence number were opened by research nurses immediately before extubation.
As per protocol, infants in the HHHFNC group were on binasal cannula (BC2425 model, Fisher and Paykel Healthcare, Auckland, New Zealand), 2.4 mm in outer diameter, occupying approximately half of the nares diameter. A flow rate of 4 L/min for infants’ weight < 1000 g or 6 L/min for infants’ weight ≥ 1000 g was applied to obtain an estimated intrapharyngeal pressure of 5–6 cm H2O as mentioned in a previous study [16]. The authors also used humidifier (MR 850, Fisher and Paykel Healthcare) with an invasive mode to obtain optimal humidity [37 °C, 100% relative humidity (RH) and absolute humidity (AH) of 44 mg/L] as per the manufacturer’s recommendation. Meanwhile infants in the CPAP group were on variable flow CPAP generator (Fabian, Acutronic, Hirzel, Switzerland) via nasal mask. The CPAP pressure was set similar to the pressure of PEEP of ventilator setting, with the same FiO2 as before enrollment. The study protocol is shown in Fig. 1.
The primary outcome was the rate of extubation failure within 72 h after endotracheal tube removal [17]. Criteria for extubation failure was defined as one of the five following: (1) increased work of breathing defined as having any sign of increase in respiratory rate by >25%, accessory respiratory muscle usage, grunting or chest wall retractions, (2) apnea, a cessation of breathing for at least 20 s, or shorter with bradycardia that occurred >3 times within 1 h during 6 h observation, (3) apnea requiring positive pressure ventilation, (4) FiO2 requirement >0.6 to keep SpO2 88–93%, (5) worsening blood gas, pH <7.25 or pCO2 > 65 mmHg.
If infants in the HHHFNC group met extubation failure criteria, they were rescued by CPAP 6 cm H2O with similar FiO2. Changes of support in both groups to non-synchronized nasal intermittent positive pressure ventilation (NIPPV) or bi-level CPAP or immediate intubation depended on the physician’s discretion. After 72 h of study period, the pressure or flow rate was weaned as per the weaning protocol [18].
Secondary outcomes were related morbidities including moderate to severe bronchopulmonary dysplasia (BPD), intraventricular hemorrhage (IVH) grade ≥ 3, patent ductus arteriosus (PDA) requiring medical or surgical closure, surgical necrotizing enterocolitis (NEC), retinopathy of prematurity (ROP) and pneumothorax. Severity of BPD was defined according to the National Institute of Child Health and Human Development Neonatal Network Criteria [19]. Cranial ultrasound screening for IVH was done in all infants and the severity of IVH was classified according to Papile’s classification [20]. Nasal trauma, defined as any sign of skin redness or skin breakdown related to interface application, was assessed and recorded by the primary care nurses and approved by the research nurse.
Chi-square test and Fischer exact test were used to compare categorical variables, while Mann-Whitney U test was used to compare continuous variables.
Sample size was calculated based on the previous studies by Campbell et al. [11] in which extubation failure rate in HHHFNC and CPAP groups were 60% and 15%, respectively. Estimated number of patients required to demonstrate a statistically significant difference with 80% power, alpha of 0.05, and two tailed test was 22 in each group. Considering a drop-out rate of 10%, the number of 24 per group was required.
Results
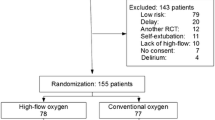
Sixty-two preterm infants were intubated during the study period. Thirteen infants were excluded. Therefore, 49 infants were enrolled; 24 in the HHHFNC and 25 in the CPAP group. Baseline demographic and respiratory conditions before enrollment were similar between groups (Table 1).
There was no significant difference in extubation failure between the two groups, (p 0.47). In HHHFNC group, 16 infants (67%) were successfully extubated. Eight infants (33%) met failed extubation criteria, out of which six (75%) were rescued by bilevel CAP, leaving two infants requiring reintubation; reintubation rate was 8.3%. In CPAP group, 19 infants (76%) were successfully extubated. Six infants (24%) met failed extubation criteria, out of which four (66%) were rescued by bilevel CAP leaving two infants requiring reintubation; reintubation rate was 8%. Ten infants [10 out of 14, (71%)] who met failed extubation criteria had GA <28 wk (six infants in HHHFNC and four infants in CPAP group) and all needed reintubation. Among infants who met failed extubation criteria, the main reason was an increase in work of breathing; six infants (75%) in HHHFNC and three infants (50%) in CPAP group. One infant in HHHFNC and two infants in CPAP group required FiO2 higher than 0.6. Finally, one infant in CPAP had frequent apnea and one infant in HHHFNC had apnea requiring PPV.
Morbidities and other complications were not different between the two groups. The secondary outcomes, including moderate to severe BPD (40% vs. 48%; p 0.73), NEC stage ≥II (8.3% vs. 8%; p 0.97), ROP stage ≥III (16% vs. 30%; p 0.83), PDA needed medical or surgical closure (54% vs. 72%; p 0.34), IVH grade III-IV (8% vs. 4%; p 0.52), were not different between HHHFNC and CPAP groups. However, infants in the HHHFNC group had significantly less nasal trauma (16.7% vs. 44%; p 0.03). No death before discharge or pneumothorax after enrollment was observed.
Discussion
The index study showed that there was no significant difference in extubation failure and reintubation rate between HHHFNC and CPAP groups. In the index study the extubation failure rate is quite similar to the previous studies by Manley et al. [12] (34.2% in HHHFNC and 25.8% in CPAP groups) and Collins et al. [13] (22% in HHHFNC and 34% in CPAP groups). However, reintubation rate in index study, approximately 8%, is lower than that of Manley’s study (17.8% in HHHFNC and 25.2% in CPAP group) [12]. This result may be due to the difference in the rescue protocols. The authors found that 75% and 66% of infants who met failed extubation criteria in HHHFNC and CPAP groups could be rescued by bilevel CPAP. These may be explained by the enhancement of lung recruitment and improvement of gas exchange from opening some microatelectasis after extubation by bilevel CPAP [21].
The main reason for extubation failure in index study was an increase in work of breathing, while frequent apnea was the main reason in other studies [12, 13]. This is probably due to the difference in predefined criteria for extubation failure. In the index study, 71% of infants who met the extubation failure criteria and all of the infants who needed reintubation were born at <28 wk of gestation. This finding is supported by a previous study [12] showing that using HHHFNC in infants <26 wk of gestation has very high extubation failure rate. Thus, using HHHFNC immediately after extubation in extremely preterm infants should be cautious.
In the index study, most of the infants received surfactant, except nine infants in HHHFNC and eight infants in CPAP group. However, apart from two infants in each group, these infants were still diagnosed as having mild RDS, which may not influence the primary outcome. The authors used aminophylline instead of caffeine because caffeine is not available in their unit. They excluded infants under 700 g because proper size of nasal cannula for these small infants is also not available. The humidifier system was set in an invasive mode to obtain optimal humidity at 37 °C in order to reduce respiratory epithelium dryness and maintain normal cilia function. The acceptable range of SpO2 was set at 88–93% due to the evidence at the time of the study period [22].
In the past, a flow rate of HHHFNC was not allowed to exceed 2 L/min due to unpredicted intrapulmonary pressure delivered by HHHFNC [9, 11]. However, recent studies have shown that using a flow rate of 4–6 L/min with a suitable size of nasal cannula, diameter approximately 50–80% of infants’ nares, would be safe for preterm infants [12–14]. A meta-analysis has also shown no differences in mortality or pulmonary air leak between HHHFNC and other forms of non-invasive respiratory support [23]. Rates of BPD, ROP and PDA needing treatment were higher in the CPAP group but did not reach statistical significance. These findings may be accidental findings due to the small sample size. In addition, infants who met failed extubation criteria in HHHFNC group were rescued by bilevel CPAP, therefore, it is difficult to draw any conclusion.
Incidence of nasal trauma in the HHHFNC group was significantly lower than that of the CPAP group. Most of the lesions were minor trauma such as skin redness or blanching and did not require other interventions. Traumatic sites were mostly located on nasal bridge and columella from the pressure effect of the devices, especially in extremely premature infants. These findings are supported by a meta-analysis which reveals that nasal mucosa injury scores are significantly lower in HHHFNC compared to other forms of non-invasive ventilation [23]. Delivering accurate pressure of variable flow via CPAP requires a tightly sealed nasal interface; the tighter it is, the more likely for skin breakdown and mucosa injuries to occur. Conversely, the major mechanism of HHHFNC is to wash out nasopharyngeal dead space with humidified and warm gas [24] and, for that reason, a gap between nasal cannula and nares is required to wash out the gas. Therefore, the direct pressure effect between the appropriate size of cannula of HHHFNC and nares is much lower than those of CPAP nasal interfaces, resulting in less nasal trauma.
The strengths of this study are the predefined study protocol and failed extubation criteria. The authors used the same types of equipment for each group along the study. However, some limitations include small sample size, being conducted in one center, and a non-blinded study. Possible bias could occur because some of the failed extubation criteria were subjective and depended on physician’s discretion. Type II error can not be excluded because the hypothesis of this study was based on the limited evidence from the previous study by Campbell et al. [11] at the time of protocol preparation. They had shown that infants who are placed on HHHFNC after extubation have a much higher rate of extubation failure compared to those placed on CPAP. The post hoc power calculation of the primary outcome (extubation failure rate) is low, as a result of an unexpectedly low extubation failure rate in HHHFNC group with an absolute difference of only 9%. To detect this small difference, with a power of 80%, the required number of infants would be 416 in each group.
In conclusion, the present study shows that there is no significant difference between HHHFNC and CPAP in extubation failure rate within 72 h after endotracheal tube removal. HHHFNC could be considered as an alternative respiratory support for infants after extubation. However, a study with larger sample size is needed, especially in extremely preterm infants.
References
Diblasi RM. Nasal continuous positive airway pressure (CPAP) for the respiratory care of the newborn infant. Respir Care. 2009;54:1209–35.
Garg S, Sinha S. Non-invasive ventilation in premature infants: based on evidence or habit. J Clin Neonatol. 2013;2:155–9.
Wilkinson D, Andersen C, O'Donnell CP, De Paoli AG. High flow nasal cannula for respiratory support in preterm infants. Cochrane Database Syst Rev. 2011:CD006405.
Hough JL, Shearman AD, Jardine LA, Davies MW. Humidified high flow nasal cannulae: current practice in Australasian nurseries, a survey. J Paediatr Child Health. 2012;48:106–13.
Nath P, Ponnusamy V, Willis K, Bissett L, Clarke P. Current practices of high and low flow oxygen therapy and humidification in UK neonatal units. Pediatr Int. 2010;52:893–4.
Manley BJ, Dold SK, Davis PG, Roehr CC. High-flow nasal cannulae for respiratory support of preterm infants: a review of the evidence. Neonatology. 2012;102:300–8.
Sreenan C, Lemke RP, Hudson-Mason A, Osiovich H. High-flow nasal cannulae in the management of apnea of prematurity: a comparison with conventional nasal continuous positive airway pressure. Pediatrics. 2001;107:1081–3.
Kugelman A, Riskin A, Said W, Shoris I, Mor F, Bader D. A randomized pilot study comparing heated humidified high-flow nasal cannulae with NIPPV for RDS. Pediatr Pulmonol. 2015;50:576–83.
Abdel-Hady H, Shouman B, Aly H. Early weaning from CPAP to high flow nasal cannula in preterm infants is associated with prolonged oxygen requirement: a randomized controlled trial. Early Hum Dev. 2011;87:205–8.
Sasi A, Malhotra A. High flow nasal cannula for continuous positive airway pressure weaning in preterm neonates: a single-centre experience. J Paediatr Child Health. 2015;51:199–203.
Campbell DM, Shah PS, Shah V, Kelly EN. Nasal continuous positive airway pressure from high flow cannula versus infant flow for preterm infants. J Perinatol. 2006;26:546–9.
Manley BJ, Owen LS, Doyle LW, et al. High-flow nasal cannulae in very preterm infants after extubation. N Engl J Med. 2013;369:1425–33.
Collins CL, Holberton JR, Barfield C, Davis PG. A randomized controlled trial to compare heated humidified high-flow nasal cannulae with nasal continuous positive airway pressure postextubation in premature infants. J Pediatr. 2013;162:949–54.e1.
Yoder BA, Stoddard RA, Li M, King J, Dirnberger DR, Abbasi S. Heated, humidified high-flow nasal cannula versus nasal CPAP for respiratory support in neonates. Pediatrics. 2013;131:e1482–90.
Wilkinson D, Andersen C, O'Donnell CP, De Paoli AG, Manley BJ. High flow nasal cannula for respiratory support in preterm infants. Cochrane Database Syst Rev. 2016;2:CD006405.
Wilkinson DJ, Andersen CC, Smith K, Holberton J. Pharyngeal pressure with high-flow nasal cannulae in premature infants. J Perinatol. 2008;28:42–7.
Rothaar RC, Epstein SK. Extubation failure: magnitude of the problem, impact on outcomes, and prevention. Curr Opin Crit Care. 2003;9:59–66.
Soonsawad S, Tongsawang N, Nuntnarumit P. Heated humidified high-flow nasal cannula for weaning from continuous positive airway pressure in preterm infants: a randomized controlled trial. Neonatology. 2016;110:204–9.
Jobe AH, Bancalari E. Bronchopulmonary dysplasia. Am J Respir Crit Care Med. 2001;163:1723–9.
Papile LA, Burstein J, Burstein R, Koffler H. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J Pediatr. 1978;92:529–34.
Migliori C, Motta M, Angeli A, Chirico G. Nasal bilevel vs. continuous positive airway pressure in preterm infants. Pediatr Pulmonol. 2005;40:426–30.
Askie LM, Henderson-Smart DJ, Irwig L, Simpson JM. Oxygen-saturation targets and outcomes in extremely preterm infants. N Engl J Med. 2003;349:959–67.
Kotecha SJ, Adappa R, Gupta N, Watkins WJ, Kotecha S, Chakraborty M. Safety and efficacy of high-flow nasal cannula therapy in preterm infants: a meta-analysis. Pediatrics. 2015;136:542–53.
Dysart K, Miller TL, Wolfson MR, Shaffer TH. Research in high flow therapy: mechanisms of action. Respir Med. 2009;103:1400–5.
Acknowledgements
The authors express their sincere thanks and gratitude to Sam Ormond for her editorial assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
SS: Developed research proposal, data collection, analysis and wrote the manuscript; BS and AL: Data collection and wrote the manuscript; PN: Developed research proposal, analysis, wrote the manuscript and will act as guarantor for the paper.
Compliance with Ethical Standards
ᅟ
Conflict of Interest
None.
Source of Funding
This study was supported by the Ramathibodi Research Fund No. 56051.
Rights and permissions
About this article
Cite this article
Soonsawad, S., Swatesutipun, B., Limrungsikul, A. et al. Heated Humidified High-Flow Nasal Cannula for Prevention of Extubation Failure in Preterm Infants. Indian J Pediatr 84, 262–266 (2017). https://doi.org/10.1007/s12098-016-2280-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12098-016-2280-2