Abstract
Background
Death after withdrawal of mechanical ventilation frequently follows the sequence of progressive hypoxemia and hypotension leading to cardiac arrest. Accurate timing of the determination of death is fundamental to trust in controlled donation after circulatory death (cDCD) programs and is generally based on cessation of circulation (pulselessness), brain function (apnea), and the passage of time. If death is understood to be the unresuscitatable loss of brain function, the clinical determination that death following apnea and pulselessness has occurred is largely inferential. We sought to elucidate the relationship between the available clinical variables and the loss of brain function and its inability to be resuscitated.
Methods
We developed a rat model of progressive hypoxia resulting in apnea and circulatory failure. We monitored clinical physiological variables including heart rate, respiration, and arterial pulse pressure. In addition, we simultaneously monitored spontaneous and evoked brain activity within the hippocampus through microelectrode field potential recordings. We also examined neurological function following restoration of pulmonary and circulatory function.
Results
Our data provide evidence that in a model of progressive hypoxemia, loss of spontaneous and evoked brain activity preceded the loss of circulation. Importantly, the data suggest that the loss of brain function, in the presence of restored cardiopulmonary indices, occurred at a time point after apnea but before the loss of detectable arterial pulse pressure.
Conclusions
These are important data that act as a conceptual reference point when clinicians undertake the inferential activity of identifying the time prior to which a patient has died following progressive hypoxemia and while observing apnea and pulselessness.
Similar content being viewed by others
Introduction
Controlled donation after circulatory death (cDCD) has become an important source of transplantable organs [1]. The term ‘controlled’ refers to anticipated and imminent death after a decision to withdraw life-sustaining treatment, following the conversion of clinical goals from invasive physiological support to comfort care measures. Death after withdrawal of mechanical ventilation frequently follows the sequence of progressive hypoxemia and hypotension leading to cardiac arrest. The acceptance of this form of donation is grounded in the confidence in regard to the timing of the clinical determination of death. There are several approaches to declaring and understanding death as it relates to organ donation. In general, we observe three patterns of final common physiological pathways leading to death [2]. These include the loss of intracranial blood flow from raised intracranial pressure, sudden or precipitous cessation of systemic circulation followed by a period of time and the absence of any return of circulation, and progressive hypoxemia and/or hypotension followed by apnea and pulselessness. The last pattern is one that is typically observed during cDCD and is based on the permanent cessation of circulation associated with the cessation of brain function. However, if death is understood to be the unresuscitatable loss of brain function, the clinical determination that death following apnea and pulselessness has occurred is largely inferential. While there may be several ways to assert that the death of a person has occurred, an unresolved question is the timing of the loss of any possibility of functional brain resuscitation.
Apnea, pulselessness, and the progress of time are clinical features that are objectively available to the careful observer. Recent human observational studies confirm the feasibility and acceptability of enhanced physiological monitoring (invasive arterial blood pressure, electrocardiogram (EKG), oxygen saturation) and electroencephalography during the dying process in intensive care unit patients [3]. This monitoring improves upon commonly used surrogate endpoints such as breath sounds, palpable pulse, or detection of heart beat by auscultation.
In a rodent model of progressive hypoxemia and controlled circulatory arrest, this study aimed to elucidate the temporal relationship between the observable findings of apnea and pulselessness, and the conceptual time of death, as defined by both the loss of brain function, and the inability to restore brain function with resuscitation. Our data provide preclinical findings that shed light on the temporal course of events in relation to the cessation of breathing and loss of cardiac function. Importantly, we demonstrate the relationship between these clinically available variables and the loss of spontaneous and evoked brain activity. We also provide some insight on the effects of resuscitation on recovery of neurological activity at various time points in relation to apnea and loss of circulatory function. This may add reference information to aid in the confidence and decision making for the clinical inferential activity of the identification that death has occurred, following progressive hypoxemia, while observing apnea and the absence of pulse pressure.
Methods
We used a model of progressive hypoxia to induce respiratory and cardiac failure and measured arterial pulse pressure with an invasive arterial line catheter as well as noninvasively using pulse oximeter technology. We also recorded spontaneous brain activity through micro-EEG recordings as well as evoked potential within the CA1 region of the hippocampus.
All animal procedures were performed in accordance with guidelines established by the Animal Care Committee at St. Michael’s Hospital in accordance with the standards set by the Canadian Council on Animal Care. The study was designed in accordance with ARRIVE (Animal Research: Reporting and In Vivo Experiments) guidelines.
Surgical Preparation
Male Sprague–Dawley rats weighing 450–550 g were anesthetized with mixture of ketamine/xylazine at 100 and 10 mg/kg, respectively, and mounted into a stereotaxic device. Given the likelihood of hypoventilation during hypoxemia and the potential for inadequate anesthetic maintenance with volatile gas delivery, an injectable anesthetic agent was used in order to maintain an adequate level of anesthesia for the duration of the hypoxemia protocol. In order to minimize physical perturbation of the rat which could influence electrophysiological recordings, a catheter and line attached to a syringe with the ketamine/xylazine anesthetic were inserted intraperitoneally to allow for subsequent injections of ketamine during the recording period. A 24-G catheter was inserted into the tail artery and sutured into place to prevent slippage. The arterial line was connected to a Luer-Lock bidirectional attachment. This was attached to a syringe filled with heparinized 0.9% saline and used to flush the line prior to arterial pulse pressure measurements and in the event of line blockage due to clotting which could influence arterial pulse pressure measurements. A midline incision was made on the head and soft tissues cleared to expose the skull. A burr hole was made in the right parietal skull plate large enough to accommodate the recording and stimulating electrodes. The trephined hole originated from the Bregma and extended occipitally approximately 4 mm. The width of the burr hole spanned approximately 3 mm originating at the midline suture extending laterally along the right parietal skull plate. A second 1-mm burr hole was made in the center of the left parietal skull plate, and a jeweler’s screw was inserted as the reference ground electrode.
Electrophysiological and Physiological Recording Setup
The rat was then transferred to the stereotaxic electrophysiology recording station. A nose cone was fitted to the rat and supplied breathing grade air delivered from a compressed gas cylinder. The air line was also connected to a HypoxyDial apparatus (Starr Life Sciences Corp, Oakmont, PA, USA) which was fed in parallel with a nitrogen gas line. The amount of oxygen delivery to the rat could be manually controlled via the HypoxyDial system at a range of inspired fraction of oxygen from 20 to 0% as required for the study.
Electrophysiological recordings were made in vivo from the CA1 region of the hippocampus using glass microcapillary pipettes pulled on a Narishige PP-830 pipette puller. Micropipettes were pulled with resistances of 2–3 MΩ. Pipettes were back-filled with 0.9% isotonic sterile saline. The microcapillary recording electrode was mounted onto a micromanipulator apparatus and attached to an Axopatch 200B headstage and amplifier. Recording microelectrodes were lowered into the dorsal CA1 region (AP = −3.5, ML 2.0 mm, DV −2.5 mm). Electrical stimulation of the hippocampus was performed using a concentric bipolar platinum/iridium electrode placed in the Schaeffer collateral fibers region (AP −3.0, ML 3.0 mm, DV −3.0 mm). Final placement of electrodes was optimized to achieve the largest evoked response and further confirmed by the shape of the evoked stimulus response. Stimulation pulses of constant current (0.1–0.5 mA amplitude, 0.05-ms duration) were generated by a Grass S88 stimulator (Grass Instrument, West Warwick, RI) and delivered through an isolation unit every 15 s. For data acquisition, the stimulation intensity was adjusted depending on the strength of signal obtained. A stimulation level that would achieve 70–80% maximum evoked response was used for data acquisition. Evoked fEPSP data were simultaneously captured using Clampex software (Molecular Devices, Sunnyvale, CA) and LabChart 7 (AD Instruments, Colorado Springs, CO). Spontaneous local field potential (LFP) electrophysiological activity was monitored with LabChart 7. Electrophysiological data were filtered at 5 kHz. Evoked fEPSP data were analyzed with the pCLAMP 10 Clampfit software.
Physiological Data Acquisition
In addition to electrophysiological monitoring of evoked and spontaneous brain activity, arterial pulse pressure was recorded from the tail artery. EKG leads connected to a BioAmp unit (AD Instruments) were placed on the front limbs, and the rear hind limb was used as the ground reference. Arterial pulse pressure recordings and EKG data were fed into a PowerLab system (AD Instruments) and data acquired with LabChart. A MouseOx Plus system (Starr Life Sciences Corp) was also used to noninvasively capture data on arterial oxygen saturation, heart rate, breath rate, pulse distension (a surrogate for arterial pressure), and breath distension (a surrogate for breathing effort). MouseOx data were also acquired using LabChart. The MouseOx and tail artery pressure monitor and EKG provided some redundant information on heart rate and arterial pressure. However, as rats approached hypoxic levels that resulted in reduced heart rate and arterial pressure, readings from the MouseOx system became less reliable as the pulse oximeter technology depends on adequate blood flow to the recording limb. In our study, we used the rear left foot pad for MouseOx sensor placement. Data acquisition rates for physiological recording were 1–2 and 10 k/s for gap-free electrophysiological data collection from evoked and spontaneous brain activity, respectively.
Induced Hypoxia and Resuscitation Protocols
A baseline recording was made for 5–10 min at 20% inspired fraction of oxygen. The inspired oxygen fraction was reduced to 15% for 5 min followed by a reduction to 12% and then 10% at 5-min intervals. Thereafter, inspired oxygen fraction was decreased in 1% increments every 5 min until fractions were at 6–7% depending on the breath rate of the test rat. The aim was to achieve a level of hypoxia which did not result in acute and immediate respiratory failure, but did result in gradual decline of respiratory function leading to prolonged and sustained apnea. Apnea was defined as the loss of visible evidence of active breathing which could be observed from the displacement of the thoracic cavity and abdomen. Prolonged apnea which coincided with a loss of spontaneous neurological activity was marked as time zero (T = 0). The time to loss of measureable arterial pulse pressure was recorded following apnea using the intraarterial catheter and the MouseOx system. Rats were divided into resuscitated and nonresuscitated groups. Resuscitation groups were further divided into subgroups. Resuscitation consisted of assisted ventilation via the fitted nose cone and was applied using a mechanical ventilator (Kent Scientific, Torrington, CT). Ventilation rate was set at 105 breaths per minute with a flow rate of 4–5 L/min of room air. This provided sufficient pulmonary inflation to a level that resulted in observable lung distention in the rat. Following the onset of terminal apnea, mechanical ventilation was applied at 30-s incremental time points starting at T = 2 min from the onset of apnea up to 5 min from the time of apnea. Ventilation was applied for a minimum of 10 min before mechanically assisted ventilation was removed and the rat allowed to breathe spontaneously (Fig. 1a). We recorded the time to loss of spontaneous breathing following resuscitation and the time to undetectable arterial pulse pressure in instances where spontaneous breathing was not maintained after resuscitation.
a Summary of the overall study design. Baseline recordings were performed for 5–10 min followed by incremental reduction in oxygen delivery to induce prolonged hypoxia. The time of apnea was marked as time = 0. Mechanical ventilation was administered at various time points following initial apnea. Ventilation was applied for 10 min prior to removal to determine whether rats were able to maintain spontaneous breathing and monitor brain activity. b A representative summary graph of the measures physiological parameters during the course of the hypoxia/cardiac arrest protocol
Statistics
Correlation analysis was performed using the Pearson product-moment correlation to examine relationships between the time to apnea and the time to loss of detectable arterial pulse pressure, time to apnea and the loss of evoked fEPSP response, and the time to loss of evoked fEPSP response and the range of stimulation used to evoke the response.
Results
Effects of Progressive Ambient Hypoxia on Physiological Variables
The total number of animals used for this study was n = 18. While all attempts were made to record electrophysiological and physiological parameters simultaneously, not all data sets were reliably recorded and quantifiable. Hence, the number of animals in data analysis varies. The group sizes for data comparisons described below were as follows: time to apnea in relation to time to loss of evoked potentials (n = 16); time to loss of evoked potentials at over various stimulation ranges (n = 15); time to pulselessness from the onset of apnea (n = 10).
The typical physiological response to gradual reduction of inspired fraction of oxygen is illustrated in Fig. 1b. This hypoxic challenge resulted in a progressive decrease in systemic oxygen saturation over time. Pulse distension, used as a surrogate for arterial pulse pressure, was observed to increase initially (also confirmed through the arterial pulse pressure measurements), along with respiratory rate. Just prior to the onset of apnea, arterial pulse pressure declined along with heart rate. Breath distension, a surrogate for breathing effort, progressively increased over the course of the hypoxia treatment protocol.
The onset of apnea was determined as the loss of any visible breathing activity. The mean time to the onset of apnea with the gradual hypoxia challenge was 48.1 ± 20.9 min (SD). The time to loss of detectable arterial pulse pressure (asystole) following apnea as measured by the arterial line catheter was 4.3 ± 1.0 min (SD). We postulated that there could be a relationship between the time required to achieve apnea and the time to asystole. For example, a rapid onset of apnea from hypoxic challenge could conceivably result in greater resilience in residual circulatory function compared to a rat that had been metabolically challenged with hypoxia over a prolonged duration. We found no correlation between the time to apnea and the time to loss of arterial pulse pressure (P > 0.05) Fig. 2.
Effects of Hypoxia on Evoked and Spontaneous Brain Activity
Local field potential recordings in the anesthetized rat were characterized by large-amplitude slow delta oscillations (<1.5 Hz) and smaller-amplitude gamma oscillations (Fig. 3a) which has been well documented in other rodent anesthetic studies [4, 5]. The frequency of delta oscillations was reduced in response to hypoxia. At terminal levels of hypoxia (at inspired oxygen fractions of 6–7%), slow oscillations were found to parallel observed breathing activity. The onset of apnea corresponded with a loss of delta wave oscillations as well as an absence of gamma oscillations (Fig. 3b). Cessation of active breathing resulted in loss of spontaneous electrical activity but was still associated with a detectable arterial pulse signal (Fig. 3c).
a Representative micro-EEG traces (upper traces) of spontaneous brain electrical activity in the hippocampus at baseline, 10% oxygen, 7% oxygen, and 6% oxygen. Corresponding arterial pulse pressure signal measured via the arterial line catheter is presented in the lower traces. b Representative tracing of brain activity (upper traces) and corresponding arterial pulse pressure (lower traces) at the moments just preceding the onset of apnea. The onset of apnea was identified by the lack of visible breathing movements in the thoracic cavity which also correlated with brain activity. c Representative traces of micro-EEG recording (upper trace) and corresponding arterial pulse pressure (lower trace) at 1 min following the cessation of spontaneous brain activity
Evoked field potential amplitudes were stable in baseline recordings and at 15% O2 (Fig. 4a). fEPSP amplitudes gradually decreased over time with the hypoxia challenge. At the time of final apnea, there was still a detectable evoked fEPSP response. Stimulation of the Schaffer collaterals was maintained during the apnea phase. Rats were continuously monitored until the loss of evoked fEPSP signal. The mean time to loss of evoked fEPSP response following apnea was 2.3 ± 1.0 min, notably earlier than the time to loss of arterial pulse pressure. We also examined the relationship between time to loss of fEPSP response and the level of stimulation used to elicit the evoked response to account for any potential biases in results due to recruitment of fEPSP response with higher stimulation levels (Fig. 4b). We found no significant correlation between the level of stimulation used to elicit evoked responses and the time to loss of evoked potentials following apnea. We also examined the relationships between the time to onset of apnea and the time to loss of evoked fEPSP response. The r value was 0.667 and a p value was 0.004 indicating that longer time to apnea was also associated with longer time to achieve loss of evoked potentials (Fig. 4c).
a Representative evoked fEPSP traces from the CA1 hippocampus at baseline, 10% oxygen, 7% oxygen, 6% oxygen, immediately following apnea (post-apnea) and at the time of mechanical ventilation protocols. b The time to loss of evoked fEPSP signal following the onset of apnea was not related to the strength of stimulation suggesting that the results were not biased due to artifacts of minimal or over-stimulation parameters. c There was a significant correlation (p = 0.004) between the time to achieve apnea due to hypoxia and the length of time required for the loss of fEPSP signal (R 2 value = 0.667)
Physiological Changes Following Resuscitation Protocols
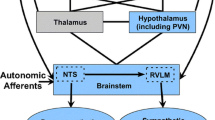
Rats which underwent resuscitative mechanical ventilation for 10 min demonstrated a recovery in fEPSP response of varying degrees dependent on the time to initiation of resuscitation. Evoked fEPSP amplitudes in resuscitated rats did not reach baseline amplitudes. In rats that were successfully resuscitated, LFP activity was observed but with varying degrees of activity. Responses ranged from recovery of delta and gamma oscillations to stochastic brain patterns. In rats resuscitated at 2:30 min or earlier following the onset of apnea, all resuscitated rats were able to maintain spontaneous breathing activity without mechanical assistance. At 3:00–3:30 min following apnea, resuscitated rats regained neurological activity but were characterized by intermittent brain activity with quiescent periods. Moreover, only 3 of 7 rats were able to maintain unassisted breathing activity following discontinuation of mechanical ventilation. Rats that had ventilation initiated at 4 min or longer following the onset of apnea did not demonstrate a recovery of neurological activity with mechanical resuscitation with the exception of 1 of 6 rats in this group. However, none of the rats in this group was capable of maintaining cardiopulmonary function in the absence of mechanical assistance. The general results of our findings are summarized in the flowchart in Fig. 5.
Flowchart summary of protocol and generalized findings. Application of the hypoxia protocol until apnea coincided with a loss of detectable mEEG spontaneous brain activity. Evoked potentials were persistent as was a detectable pulse at this time period. In the absence of a resuscitation protocol, evoked brain activity was lost at 2.3 ± 1.0 min following apnea. Notably, a detectable pulse was lost at a later time point at 4.3 ± 1.0 min after apnea. When a resuscitation protocol was implemented, three categorical physiological responses were observed. Those animals that underwent resuscitation at 2 min and 30 s or less from the onset of apnea regained evidence of neurological activity and were able to maintain cardiopulmonary activity without assistance. Animals that were resuscitated between 3:00 and 3 min and 30 s after the onset of apnea had evidence of neurological recovery characterized with intermittent mEEG activity and reduced fEPSP amplitudes. Three of 7 subjects could sustain unassisted cardiopulmonary function. Animals given mechanical ventilation 4 min or greater after the onset of apnea did not recover neurological function except for one rat*. Moreover, cardiopulmonary self-maintenance was not observed in this resuscitation group
Discussion
In a rodent model of progressive hypoxemia and controlled circulatory arrest, this study aimed to elucidate the temporal relationship between the observable findings of apnea and pulselessness, and invasively monitored cardiorespiratory and neurologic function. This study may begin to inform the time that death has occurred, as defined by both the loss of brain function and the inability to restore brain function with resuscitation. The observations made in this model were of a sequence of events that started with progressive reduction in the inspired fraction of oxygen in order to generate a model of progressive hypoxemia. We observed a progressive reduction in pulse pressure followed by apnea and subsequently followed by pulselessness. With the aid of electrophysiological monitoring of the hippocampus, we observed the loss of spontaneous electrical activity at about the same time as we observed apnea. With active resuscitation, we observed the absence of the ability to generate a stimulated hippocampal response in the presence of an adequate pulse pressure and systemic oxygen tension, when this systemic resuscitation was conducted at a time point after apnea and before the onset of pulselessness. While there are various conceptual definitions of death, if the definition of death is the physiological state where fundamental brain function cannot return despite systemic resuscitation, then we have described an animal model of progressive hypoxemia leading sequentially to apnea, death, and then pulselessness. It is not new that we identify death in the presence of a pulse. This is the essence of death by neurological criteria or so-called brain death. It is not surprising that a sustained hypoxic insult of sufficient severity could lead to the irreversible loss of fundamental brain function even with the restoration of systemic normoxia and blood pressure. Further, it is not surprising that an otherwise healthy heart would likely persevere functionally longer than an otherwise healthy brain, when both are exposed to equal degrees of hypoxemia and hypotension. Indeed, our observation that spontaneous electrical activity of fundamental structures of the brain ceased at the same time as the onset of apnea arising from hypoxemia is equally not surprising. The purpose of this study therefore was to illustrate these expected results in clear juxtaposition and as a way to highlight the important clinical observation of apnea as an observable sign of the arrest of brain function in an analogous clinical setting of progressive hypoxemia.
The sequence of apnea, death, and pulselessness is certainly not the exclusive pathway involving death—even in the context of progressive hypoxemia. In the raised intracranial pressure scenario, death follows apnea, but pulselessness may be significantly delayed by hours, days, or even months when mechanical ventilation is provided. In sudden cardiac arrest or the sudden termination of supported circulation, such as cardiopulmonary resuscitation (CPR) or extracorporeal cardiopulmonary resuscitation, we observe sudden pulselessness, followed within seconds by neuroelectrophysiological standstill and apnea [6]. Following this, two parallel pathways proceed, unless they are interrupted. The first is the progression to irreversible loss of cardiac-generated circulation, and in parallel, the second is the progression to the irreversible (cannot be resuscitated by any means) loss of brain function. The timing of irreversible loss of cardiac-generated circulation has been studied and is described either by so-called CPR stopping rules [7]—which describe when cardiac resuscitation cannot be achieved—or by the documented experience of the absence of the phenomenon of autoresuscitation after a certain number of minutes [8]. The pathway to the physiological state where the brain cannot be resuscitated even with restored oxygenated circulation is less well studied in terms of timing. Determinants likely include pre-event conditions of the brain. If the term death is used as described above, then following sudden cessation of circulation, the sequence of events can include pulselessness, apnea, and then either death followed by irreversible loss of cardiac-generated circulation, or pulselessness, apnea, irreversible loss of cardiac-generated circulation followed by death. The time to death in this last scenario lacks outward clinical signs—other than time following pulselessness—that allow bracketing the timing or otherwise gaining much precision. It is possible, however, that death occurs at some not insignificant time after the arrival of the irreversible loss of cardiac-generated circulation, albeit inevitable death, in the absence of extracorporeal methods.
In this paper, we have used the state of ‘no spontaneous electrical or even stimulated electrical response in the hippocampus in the presence of a resuscitated and adequate blood pressure and oxygen tension’ as a proxy for ‘death’ and then used the term death in the summary of our observations and conclusions. This experimental endpoint, as a proxy for death, does not meet the standard for determining brain death. This includes the fact that the hippocampus may be more sensitive to hypoxia, that there was only a limited period of normalized blood pressure and oxygen tension, and that other brain structures were not functionally evaluated. We chose this proxy because: there is good experience with measuring hippocampal activity, lead placement would not injure the brainstem and an important readout was brainstem-related apnea, the hippocampus is a central deep structure with central importance to integrated brain function, and while the duration of normalized physiology was limited, this duration did demonstrate a time-dependent relationship of this proxy (return of stimulated activity was dependent (inversely) on the delay after apnea of resuscitation). Longer periods of normalized physiology may have increased the number of rats which demonstrated a return of hippocampal function, and changed the details of this time-dependent relationship. In summary, this study used the endpoint of the inability to demonstrate any stimulated electrical activity in the hippocampus after resuscitation following hypoxia-related apnea. This endpoint was a proxy for death determination and was used to highlight relevant physiological processes in greater temporal resolution during progressive hypoxia.
The use of ketamine as an anesthetic agent includes the possibility of influence of electrophysiological activity during the hypoxemia aspects of the protocol. Given ketamine’s numerous pharmacologic targets in the central nervous system including NMDA receptors, HCN1, L-type calcium channels, AMPA receptors among many others [9], it is reasonable to suspect that in a hypoxic environment modulation of these and other affected receptors and channels could influence outcome. However, the magnitude of that effect is currently unknown. From a respiratory perspective, it has been shown clinically to have little influence on respiratory mechanics, unless overdosed [10]. In this regard, ketamine likely had minimal influence on the rate of cardiopulmonary decline. Whether ketamine contributed to a faster decline in electrophysiological brain function or was protective in a hypoxemia state is not clear from our study.
In summary, in the context of describing three pathways to death, we have presented physiological data to illustrate one sequence consisting of progressive hypoxemia. Of course, it is possible that there are other pathways and certainly more than one at a time. For example, sudden cardiac arrest may occur during progressive hypoxia, and this might change the neurological significance of the clinical finding of apnea. Nevertheless, the observations presented here provide some conceptual reference for the clinician who is observing progressive hypoxemia and eventually making the inferential conclusion that death has occurred. The significance of noting apnea prior to pulselessness is highlighted by these observations.
References
Organ donation and transplantation in Canada: System Progress Report 2006–2015. Ottawa: Canadian Blood Services; 2016. https://blood.ca/sites/default/files/ODT_Report.pdf.
Shemie SD, Hornby L, Baker A, et al. International guideline development for the determination of death. Intensive Care Med. 2014;40:788–97.
Dhanani S, Hornby L, Ward R, et al. Vital signs after cardiac arrest following withdrawal of life-sustaining therapy: a multicenter prospective observational study. Crit Care Med. 2014;42:2358–69.
Soltesz I, Deschenes M. Low- and high-frequency membrane potential oscillations during theta activity in CA1 and CA3 pyramidal neurons of the rat hippocampus under ketamine-xylazine anesthesia. J Neurophysiol. 1993;70:97–116.
Sharma AV, Wolansky T, Dickson CT. A comparison of sleeplike slow oscillations in the hippocampus under ketamine and urethane anesthesia. J Neurophysiol. 2010;104:932–9.
Pana R, Hornby L, Shemie SD, Dhanani S, Teitelbaum J. Time to loss of brain function and activity during circulatory arrest. J Crit Care. 2016;34:77–83.
Torke AM, Bledsoe P, Wocial LD, Bosslet GT, Helft PR. CEASE: a guide for clinicians on how to stop resuscitation efforts. Ann Am Thorac Soc. 2015;12:440–5.
Hornby K, Hornby L, Shemie SD. A systematic review of autoresuscitation after cardiac arrest. Crit Care Med. 2010;38:1246–53.
Lodge D, Mercier MS. Ketamine and phencyclidine: the good, the bad and the unexpected. Br J Pharmacol. 2015;172:4254–76.
Tobias JD, Leder M. Procedural sedation: a review of sedative agents, monitoring, and management of complications. Saudi J Anaesth. 2011;5:395–410.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Park, E., Liu, E., Shemie, S.D. et al. Relating Clinical and Electrophysiological Parameters in Death Determination in a Laboratory Model of Progressive Hypoxemia. Neurocrit Care 28, 133–141 (2018). https://doi.org/10.1007/s12028-017-0382-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-017-0382-y