Abstract
Background and Purpose
Patients with severe stroke who require mechanical ventilation and neurointensive care unit (NICU) management often require a tracheostomy (TT). The optimal time point for TT remains unclear and a controversy in everyday NICU life. Here, we prospectively evaluated a score for prediction of TT need in NICU patients with cerebrovascular disease.
Methods
Seventy-five consecutively ventilated stroke patients were prospectively included in the study and assessed by the stroke-related early tracheostomy score (SETscore) within the first 24 h of admission. Endpoints were TT need, NICU-length of stay (NICU-LOS), and ventilation time (VT). We examined the correlation of these variables with the SETscore using regression analysis and determined a cut-off by receiver operating characteristic (ROC) analysis.
Results
Twenty-six patients had to be tracheostomized. The mean VT was 8.7 ±8 days and the mean NICU-LOS was 11.6 ± 8 days. The SETscore predicted NICU-LOS with a positive predictive value of 0.748 (p < 0.001) and VT with a positive predictive value of 0.799 (p < 0.001). The ROC analysis demonstrated a SETscore value of 8 to be the optimal cut-off to predict prolonged NICU-LOS, VT, and TT need with a sensitivity of 64 % and a specificity of 86 %.
Conclusions
Based on this monocentric study, the SETscore seems to be a valid tool to indicate prolonged NICU-LOS and VT, as well as TT need in cerebrovascular NICU patients. Confirmation of these results in larger cohorts with various settings may help to develop the SETscore as a decisive tool on primary TT early in time to avoid extubation failure.
Similar content being viewed by others
Introduction
The prognosis of patients with severe ischemic or hemorrhagic stroke requiring NICU management and mechanical ventilation is generally poor with reported mortality rates ranging between 40 and 80 % [1–3]. Early weaning from the ventilator and extubation would be desirable in these patients, as extubation delay increases morbidity and mortality [4, 5]. However, it is particularly difficult to judge whether extubation is safe in brain-injured patients, because traditional extubation criteria, which are mostly based on the setting of the general ICU and are respiration-dominated, did not prove reliable in the prediction of extubation success or failure in this particular patient population [5, 6]. An alternative to potentially compromising extubation trials is primary tracheostomy (TT).
In critical care, it is common to do a TT if ventilated patients cannot be weaned off the respirator quickly but require long-term ventilation. Acknowledged advantages of a short tracheal tube compared to a long orotracheal one are reduction of ventilatory dead space and thus work of breathing, avoidance of oropharyngeal lesions, and facilitation of nursing care, as well as a higher patient comfort with less demand of analgesics or sedatives [7, 8]. Percutaneous dilatational tracheostomy (PDT) can be performed by neurointensivists at the bed-side quickly, at low cost and with very low complication rates [9–13]. The optimal time point for a TT is still unclear, but it is widespread critical care practice to perform the procedure after 2–3 weeks from intubation. Some previous studies in very different populations of critical care patients have suggested additional advantages of early TT, such as reduction in ventilation-associated pneumonias, analgesia and sedation, ventilation duration, ICU stay, and—in one study—even lower mortality [14–16]. The largest project in this regard, the UK TracMan Trial in more than 1000 mixed ICU patients demonstrated no benefit of early TT within 4 days of critical care admission in 30-day mortality or other important secondary outcomes [17]. Very recently, the time point of TT in mixed ICU populations was addressed in a systemic review and meta-analysis by Siempos et al suggesting that early TT is not associated with lower mortality, but might be associated with a lower rate of VAP [18]. These results may suggest that the question of early TT should rather be addressed in special ICU subpopulations than in large mixed groups.
In neurocritical care patients, a number of retrospective studies have suggested that ICU-LOS, duration of ventilation, and mortality might be potential benefits of early TT [19]. The only prospective randomized trial on potential benefits of early TT in ventilated stroke patients to date is the monocentric pilot trial stroke-related early tracheostomy vs. prolonged orotracheal intubation in neurocritical care trial (SETPOINT) [20]. The SETPOINT trial showed a significant reduction of sedatives, as well as a reduction of the ICU-mortality in the early TT group, although it should be noted that these were secondary endpoints and this pilot trial was not designed to focus on this question [19].
Here, we investigate prospectively a score to predict the need of TT in ventilated cerebrovascular NICU patients. The Stroke-related Early Tracheostomy score (SETscore) was previously used by the authors in the pilot trial SETPOINT as a screening tool for trial inclusion and it appeared to be useful. Now we have applied the score outside the trial to a new independent subgroup of 75 patients on their day of admission and analyzed its predictive value systematically.
Methods
Score
The SETscore was initially developed as an in-house screening tool based on tracheostomy predictors identified in several retrospective studies [21–23]. These were combined under the categories (1) neurological function, (2) neurological lesion, and (3) general organ function/procedure and weighed by allocation of certain point values that were based partially on relevance suggested in the retrospective studies and partially on clinical estimation. The detailed score is given in Table 1. All items were assessed within the first 24 h after admission to hospital. For each physiological variable, the worst value in the first 24 h after admission was used to achieve an estimation as early as possible (explanations for further details see reference [19]). Dysphagia has either to be reported from a transferring neurological department or be observed by clinical signs on admission, e.g., by a non-successful swallowing test, impaired saliva handling, or loss/reduction of gag reflex. If the patient is already intubated on admission, the item dysphagia is scored with “0,” (Neuro)surgical intervention constitutes a relevant operation, such as decompressive surgery, hematoma removal, or non-cranial major surgery, but not EVD or probe placement, thrombectomy, angioplasty for vasospasm or coiling. Diffuse lesion is defined as a multilocular or widespread affection of the brain such as in subarachnoid hemorrhage (SAH), brain edema, multiple infarcts, or hematomas. The definition of hydrocephalus is the distension of ventricles requiring EVD placement. Sepsis is assessed according to the current guidelines of the surviving sepsis campaign [24]. Any combination of selected components of categories 1 and 3 is possible, while some components in category 2 exclude themselves, which results in a total sum ranging between 3 and 37. The early assessment of the SETscore within the first 24 h after admission and a score of >10 (the cut-off having been an estimate based on a smaller pre-trial cohort), combined with the judgement (and possibly veto) of two experienced neurointensivists, were previously used to screen patients for eligibility to be included in the pilot trial SETPOINT. This trial on potential benefits in cerebrovascular NICU patients randomized 60 patients either for early TT (within 3 days after intubation) or to standard regime (ongoing intubation followed by weaning and extubation trials and late TT between day 7 and 14 from intubation if extubation failed) [20]. In the standard group, in which extubation was strived for by application of strict protocols, none of these patients could be successfully extubated, suggesting that the score and the selected cut-off might indeed be useful to predict TT need [19].
Patients and Data Acquisition
Data for this study were prospectively collected as a part of our study campaign to assess long-term functional outcome and life quality in ventilated neurocritical care patients. Approval for purely observational data acquisition was granted by the Heidelberg ethical committee (S-193/2011), and informed consent was obtained from the patients´ legal proxies. Over 11 months, all intubated and consecutively ventilated patients admitted to our NICU were screened for this prospective observational cohort study. Patients could be included if they were admitted for either acute ischemic infarction (AIS) or spontaneous intracerebral hemorrhage (ICH) or aneurysmal subarachnoid hemorrhage (SAH) and if they stayed intubated for at least 24 h. They were excluded if life expectancy was very low and withdrawal of care was very likely on admission. Patients were routinely intubated at a GCS score <8, when there were any signs of respiratory insufficiency (arterial pO2 < 60 mmHg and/or pCO2 > 48 mmHg), reduced swallowing or coughing reflexes, or when the airway was compromised. Intubation and ventilation was based on our institution’s standard operating procedures (SOP), and patients were weaned as soon as possible. If extubation failed or was not feasible, a TT was performed after day 10 of intubation. Analgesia and sedation were routinely applied for pain, agitation, and anxiety, and to improve the comfort of the patients. The mode of analgesia and sedation depended on the estimated time for need of sedation and was performed according to standard local practices. Locally customary agents were routinely utilized to assure patient comfort, and titrated to sedation scales such as the Sedation and Agitation Scale (SAS) of 3–4 [25, 26] or a Richmond Agitation-Sedation Scale at −2 to 4 [27, 28].
Acute kidney injury (AKI) was defined as the loss of kidney function, resulting in the retention of urea and other nitrogenous waste products and usually implying the need for renal replacement therapy [29].
The SETscore was assessed within the first 24 h by an observer independent from the treating physicians who were blinded to the SETscore result. In addition, demographic, baseline, and clinical data, among the latter particularly NICU-length of stay (NICU-LOS), ventilation time, extubation trials, re-intubations, tracheostomy, and mortality were prospectively recorded. The cut-off-day for “prolonged” NICU-LOS and VT was defined at day 10, because this was considered a common “standard” of care, based on several trials and the results from an analysis of tracheostomy practices in the US National Inpatient Sample [13, 19, 30–32], demonstrating it to be customary to tracheotomize around that time if extubation failed or was not feasible.
Statistical Analysis
Data collection was made by the use of electronic case report forms in Excel® (Microsoft Office 2011®, Microsoft®), and all statistical analyses were performed using R (version 3.2.2) [33] in combination with the packages “ROCR” (version 1.0-7) [34], “gplots” (version 2.17.0) [35], and “xtable” (version 1.7-4) [36]. In the first step, descriptive statistics for baseline variables are provided. For categorical data, absolute and relative frequencies are presented, while for continuous variables, means and standard deviations are given. Furthermore, we provide a comparison of the baseline variables between patients who required a TT and patients who did not, as well as between patients with a SETscore ≥10 and patients with a SETscore <10, since this cut-off had been applied in a clinical study before. Patient characteristics are additionally displayed in dichotomization according to the optimal cut-off derived from our analysis. Differences between the groups were assessed using the Chi square test or the t test for categorical or continuous variables, respectively. To answer our first two research questions, whether the SETscore is correlated with NICU-LOS and the ventilation time, we calculated Pearson correlation coefficients and estimated linear regression models, where the SETscore was included as a predictor variable. Since the distribution of NICU-LOS and the ventilation time was skewed, we did not use the original values but the values on a log scale. We provide the estimated coefficients (β) with 95 % confidence intervals (95 % CI), as well as back-transformed values (according to the log-transformation of NICU-LOS and ventilation time), respectively. We also used linear regression models combined with a step-wise variable selection to examine whether the single (binary) components of the SETscore are predictive of NICU-LOS and ventilation time. We applied a combination of a backward and a forward selection using p-values as the selection criteria (0.05 in the backward step and 0.049 in the forward step). Since the distribution of some items was strongly skewed, they were only included if the frequency in each category of the considered item was not less than 5. To answer the third research question, whether the SETscore is correlated with TT need, we compared the SETscore between the groups with and without TT need by a t test. Furthermore, a logistic regression model was applied to provide an odds ratio. Significance was considered at a two-sided p value of <0.05. As this was an exploratory study, we did not adjust for multiple testing.
Additionally, we derived cut-off values of the SETscore for the three outcome values using ROC analyses. For this purpose, the NICU-LOS and the ventilation time were dichotomized using cut-off values of 10 or 5 days, respectively (see the “Results” section for a justification of these values). The best cut-off values of the SETscore for each of the outcome variables were determined by maximizing the Youden-Index accordingly.
Results
Patient Characteristics
Seventy-five consecutive stroke patients who fulfilled the eligibility criteria were included in this study. The baseline and clinical characteristics are shown in Table 2. Illness severity was reflected by an average admission Glasgow coma scale (GCS) of 9.5 and an average admission National Institute of Stroke Scale (NHISS) score of 15.4. In all patients, sufficient data collection throughout the NICU stay was possible, and nine patients died during the course. 54.7 % of patients had AIS, while 45.3 % had hemorrhagic stroke, i.e., either ICH or SAH. Of the recorded comorbidities, hypertension (70.7 %), atrial fibrillation (29.3 %), hyperlipidemia (21.3 %), and diabetes mellitus (18.7 %) were the most frequent ones.
When the group was dichotomized according to whether they were tracheostomized or not at any given time from admission, male gender and renal impairment were considerably more frequent in the TT group. On the contrary, patients with ischemic stroke type as opposed to hemorrhagic at higher age were more frequently extubated (Table 3).
SETscore and NICU-Length of Stay
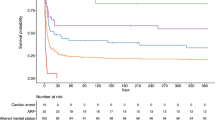
The correlation coefficient of the SETscore and NICU-LOS (on a log scale) was equal to 0.477 (Fig. 1a). The regression coefficient of the SETscore in a regression model for NICU-LOS on the log scale was 0.10 (95 % CI [0.05; 0.14], p < 0.001). For a better interpretation, a back-transformation to the original scale was performed leading to a value of exp(β) = 1.10 (95 % CI [1.06; 1.15]). This means that the expectation of NICU-LOS has to be multiplied by 1.10 when the SETscore is increased by 1 unit, i.e., the higher the SETscore the higher is the NICU-LOS value.
a Correlation between SETscore and NICU length of stay (on a log scale). The bars represent the mean of the NICU length stay (on a log scale) per SETscore value. Additionally, the estimated regression line is plotted. b Correlation between SETscore and ventilation time (on a log scale). The bars represent the mean ventilation time (on a log scale) per SETscore value. Additionally, the estimated regression line is plotted
When testing the single components of the SETscore for the prediction of NICU-LOS, we obtained the following significant predictors (expressed as exp(β) with 95 % CI): ICH volume >25 ml (1.46 [1.04; 2.04]), diffuse lesion (2.30 [1.28; 4.13]), and hydrocephalus (1.90 [1.35; 2.66]).
Of note, the score components on oxygenation failure, acute physiology disturbances, lung injury, and sepsis (score category 3) were not selected for further statistical analysis, since their distribution was extremely skewed.
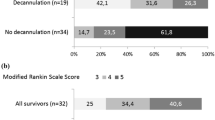
The discriminative power of the SETscore for predicting ICU stay more than 10 days (our current in-unit average length of stay) was examined using a ROC analysis. This analysis led to an area under the ROC curve (AUC) value of 0.748 which is relatively high meaning that the SETscore seems to be a useful tool to distinguish between short and prolonged ICU stays (Fig. 2). A value of 8 turned out to be the optimal cut-off, where the SETscore had a moderate sensitivity (59.5 %) and a relatively high specificity (78.9 %).
SETscore and Ventilation Time
The correlation coefficient of SETscore and ventilation time was equal to 0.540 (Fig. 1b). Estimation of the linear regression model yielded coefficients of β = 0.15 (95 % CI [0.09; 0.20], p < 0.001) and, after back-transformation, exp(β) = 1.16 (95 % CI [1.10; 1.23]), respectively. This means that the higher the SETscore, the longer was the ventilation time.
While assessing the predictive value of different components of the SETscore for the prediction of ventilation time, we obtained the following significant coefficients (expressed as exp(β) with 95 % CIs): ICH volume >25 ml (2.51 [1.66; 3.80]), diffuse lesion (3.87 [1.89; 7.95]), and hydrocephalus (1.16 [0.70; 1.61]).
The discriminative power of the SETscore for predicting ventilation time for more than 5 days (cut-off resulting in a change in our in-house sedation regime) was examined using the ROC approach. This analysis confirmed that the SETscore had a good discriminative power for predicting prolonged ventilation with an AUC of 0.799. The optimal cut-off was equal to 8 where the SETscore had a moderate sensitivity (64.1 %) and a relatively high specificity (86.1 %).
The SETscore and Prediction of Tracheostomy
Patients who were tracheostomized in their course had a significantly higher score than the others (9.73 ± 3.18 versus 6.86 ± 3.68, p = 0.001) (Table 3). When patients were dichotomized according to a SETscore above or below a sum of 10 (cut-off previously used to screen for eligibility for a past tracheostomy trial [20]), patients with a score <10 were more likely to be successfully extubated, with an odds ratio of 2.16 (95 % CI [0.77; 6.09]) (Table 4) with a re-intubation rate of 14.7 %.
ROC analysis of the SETscore for tracheostomy at any time during the course was also analyzed, which revealed that the SETscore had a good discriminative power for predicting tracheostomy with an AUC of 0.741 (Fig. 3). For a cut-off score sum of 10, the SETscore had a low sensitivity (38.5 %), but a high specificity (77.6 %) for discriminating TT (Fig. 2b). The optimal cut-off in our data was equal to 8 with a sensitivity of 65.4 % and a specificity of 73.5 %. Since a cut-off of 8 was found optimal in all three analyses, patient characteristics were dichotomized according to that cut-off and displayed in Table 5.
Discussion
Currently, it is unclear whether and when ventilated patients with ischemic or hemorrhagic stroke should obtain a TT, and to recognize the need to tracheostomize these patients is a daily dilemma. Retrospective subgroup analyses suggest that these patients could be particularly fast to wean off the ventilator after early TT because their main impairment is securing the upper airway and not breathing. Retrospectively, predictors of TT need both in the general [21, 22] and in the neurological ICU [23, 37, 38] population had been identified. For patients with supratentorial ICH, low GCS, presence of COPD, volume and thalamic location of the hematoma, midline shift, presence of intraventricular blood and hydrocephalus have been found as predictors of TT need [23, 38]. Some of these parameters have been combined to form the TRACH score for use in ICH patients with a reported positive predictive value of 95 % and a negative value of 83 % for tracheostomy need [38]. Although the airway pathophysiology of traumatic brain injury is probably similar to stroke, and several studies favored early over delayed TT [39–41], the question of early TT in non-traumatic brain diseases including stroke is presently unclear. A current review of potential benefits of early TT in ventilated stroke patients included advantages regarding ICU-LOS, VT, and mortality [20]. Furthermore, a recent analysis of the optimal point of time of TT in the National Inpatient Sample implied that a early TT before day 10 was associated with lower rate of VAP and shorter ICU stay compared with later TT [42]. However, all these studies have been retrospective so far and their results have not been prospectively validated.
Our study aimed at prospectively confirming the utility of a tracheostomy prediction score in the cerebrovascular NICU population. The SETscore, assessed within the first 24 h after admission, correlated well with both ventilation time and NICU-LOS and predicted eventual TT in our setting. More precisely, at a cut-off score sum of 8, it discriminated TT need with a sensitivity of 65.4 % and a specificity of 73.5 %. We regard the specificity as more important, because we consider an unnecessary TT is more problematic than a delayed one. With regard to the individual components of the SETscore, some components well correlated with ventilation time and NICU-LOS, supporting the respective findings in the retrospective studies. Interestingly, the component “ischemic infarct > 2/3 MCA territory” turned out to be negatively associated with NICU-LOS, and patients with ischemic stroke were less likely to be tracheostomized than with hemorrhagic stroke. This might hint to an increased chance of extubation success (i.e., reduced TT need), particularly after decompressive hemicraniectomy that most of the patients with such large infarcts received at our center, and an overall shorter NICU course in patients with ischemia compared to patients with hemorrhagic stroke in this population, but the study design does not allow for more than speculation thereof. Of note, the systemic parameters of the SETscore, i.e., those in category 3 (PaO2/FiO2 > 150, APS (of APACHEII) > 20 [43], LIS > 1 [44], and sepsis) were almost never selected by the scorer and thus are probably negligible. Of note, the SETscore has been originally developed for use within 3 days from intubation in a previous study [20] but has been tested in the current study for day 1 only. So early in time, most ventilated stroke patients are most probably unlikely to have developed pulmonary, circulatory, infectious complications or a sepsis yet, or these might not have been detected. It should therefore be interesting to investigate prospectively a reduced and modified version of the SETscore that only contains cerebral components. Another important aspect for further studies could be a larger time frame or later time point for the assessment of the SETscore (e.g., after 48 or 72 h), as complications, e.g., a progression of the cerebral lesion or cardiopulmonary compromise, may rather develop within the first days and not directly on or after admission, but may have an important impact on the clinical course and airway management decisions. Based on our findings, it would be therefore interesting to initiate a further larger prospective study with the optimal cut-off value of the SETscore of 8 and maybe with different assessment intervals (such as within the first 24, 48, and 72 h) and thus possibly come up with a shorter, simpler but for neurocritical care patients more specific version of the score, should it turn out that systemic items of the scale remain uninfluential.
Our study has a number of limitations. Above all, it is a monocentric observational study looking at customs of airway management in our own NICU. As such, prediction of “tracheostomy need” cannot be derived directly from our findings, as all we have analyzed is the correlation of the admission SETscore with the eventual clinical decision to do a tracheostomy taken by the physicians in charge who were blinded to the score result. However, this decision might not necessarily reflect ultimate need to tracheostomize according to the customs in other places. Furthermore, although the treating clinicians were unaware of the admission SETscore, components of the score had been used on our NICU in the past to guide decisions on sedation, ventilation, and airway management, so we cannot exclude a certain amount of self-fulfilling despite blinding. The true value of the score will therefore only become clear, if it is tested and confirmed in NICU settings other than our own. The score itself, especially the weighting of its components, was originally not the product of a comprehensive systematic retrospective statistical analysis, but the result of combining reported retrospective findings with subjective judgment to form an in-house screening tool and thus was to a great extent empirical and intuitive. In this validation study, the score was determined by a single investigator and thus assessment quality and precision depended completely on the judgment of the clinical and radiological situation by this single observer and nothing can be said on the interrater-reliability of the score. Also, the study population was small and heterogeneous with regard to the included brain pathologies. The latter was accepted as it is our impression that for compromise of airway protection and breathing, the relevant cause is rather the extension and location of the vascular brain lesion and not so much the specific pathological nature. However, it might still be rewarding to investigate specific scores (or reduced partial SETscore versions) in more homogeneous NICU subpopulations. Finally, due to the exploratory nature of the analysis, we applied a number of statistical tests without multiplicity adjustment and thus cannot completely exclude false positive findings.
Still, we took great efforts to collect all relevant clinical data to display a realistic NICU situation and to detect confounders as well as all possible courses the patients could take with regard to airway management. Furthermore, we are not aware of any other comparable score being investigated prospectively in this patient population.
Conclusion
In our NICU setting of 75 cerebrovascular ventilated patients, assessment of the SETscore within the first 24 h allowed for estimation of NICU-LOS, ventilation time, and likelihood of TT with agreeable certainty. It may be a useful tool to guide airway management in ventilated patients with non-traumatic ischemic or hemorrhagic brain lesions allowing for earlier TT in the respective cases. Clearly, the SETscore needs prospective confirmation in other NICU settings and larger patient populations before its true validity, reliability, and predictive potential can be judged.
References
Bushnell CD, Phillips-Bute BG, Laskowitz DT, Lynch JR, Chilukuri V, Borel CO. Survival and outcome after endotracheal intubation for acute stroke. Neurology. 1999;52:1374–81.
Gujjar AR, Deibert E, Manno EM, Duff S, Diringer MN. Mechanical ventilation for ischemic stroke and intracerebral hemorrhage: indications, timing, and outcome. Neurology. 1998;51:447–51.
Steiner T, Mendoza G, De Georgia M, Schellinger P, Holle R, Hacke W. Prognosis of stroke patients requiring mechanical ventilation in a neurological critical care unit. Stroke. 1997;28:711–5.
Chevron V, Menard JF, Richard JC, Girault C, Leroy J, Bonmarchand G. Unplanned extubation: risk factors of development and predictive criteria for reintubation. Crit Care Med. 1998;26:1049–53.
Coplin WM, Pierson DJ, Cooley KD, Newell DW, Rubenfeld GD. Implications of extubation delay in brain-injured patients meeting standard weaning criteria. Am J Respir Crit Care Med. 2000;161:1530–6.
Ko R, Ramos L, Chalela JA. Conventional weaning parameters do not predict extubation failure in neurocritical care patients. Neurocrit Care. 2009;10:269–73.
MacIntyre N. Discontinuing mechanical ventilatory support. Chest. 2007;132:1049–56.
MacIntyre NR, Cook DJ, Ely EW Jr, et al. Evidence-based guidelines for weaning and discontinuing ventilatory support: a collective task force facilitated by the American College of Chest Physicians; the American Association for Respiratory Care; and the American College of Critical Care Medicine. Chest. 2001;120:375S–95S.
Mallick A, Bodenham AR. Tracheostomy in critically ill patients. Eur J Anaesthesiol. 2010;27:676–82.
Seder DB, Lee K, Rahman C, et al. Safety and feasibility of percutaneous tracheostomy performed by neurointensivists. Neurocrit Care. 2009;10:264–8.
Delaney A, Bagshaw SM, Nalos M. Percutaneous dilatational tracheostomy versus surgical tracheostomy in critically ill patients: a systematic review and meta-analysis. Crit Care. 2006;10:R55.
Hoekema D. Percutaneous tracheostomy coming of age for the neurointensivist? Neurocrit Care. 2009;10:261–3.
Villwock JA, Jones K. Outcomes of early versus late tracheostomy: 2008–2010. Laryngoscope. 2014;124:1801–6.
Rumbak MJ, Newton M, Truncale T, Schwartz SW, Adams JW, Hazard PB. A prospective, randomized, study comparing early percutaneous dilational tracheotomy to prolonged translaryngeal intubation (delayed tracheotomy) in critically ill medical patients. Crit Care Med. 2004;32:1689–94.
Nieszkowska A, Combes A, Luyt CE, et al. Impact of tracheotomy on sedative administration, sedation level, and comfort of mechanically ventilated intensive care unit patients. Crit Care Med. 2005;33:2527–33.
Griffiths J, Barber VS, Morgan L, Young JD. Systematic review and meta-analysis of studies of the timing of tracheostomy in adult patients undergoing artificial ventilation. BMJ. 2005;330:1243.
Young D, Harrison DA, Cuthbertson BH, Rowan K, TracMan C. Effect of early vs late tracheostomy placement on survival in patients receiving mechanical ventilation: the TracMan randomized trial. JAMA. 2013;309:2121–9.
Siempos II, Ntaidou TK, Filippidis FT, Choi AM. Effect of early versus late or no tracheostomy on mortality and pneumonia of critically ill patients receiving mechanical ventilation: a systematic review and meta-analysis. Lancet Respir Med. 2015;3:150–8.
Bösel J, Schiller P, Hook Y, et al. Stroke-related early tracheostomy versus prolonged orotracheal intubation in neurocritical care trial (SETPOINT): a randomized pilot trial. Stroke. 2013;44:21–8.
Bösel J, Schiller P, Hacke W, Steiner T. Benefits of early tracheostomy in ventilated stroke patients? Current evidence and study protocol of the randomized pilot trial SETPOINT (stroke-related early tracheostomy vs. prolonged orotracheal intubation in neurocritical care trial). Int J Stroke. 2012;7:173–82.
Kollef MH, Ahrens TS, Shannon W. Clinical predictors and outcomes for patients requiring tracheostomy in the intensive care unit. Crit Care Med. 1999;27:1714–20.
Seneff MG, Zimmerman JE, Knaus WA, Wagner DP, Draper EA. Predicting the duration of mechanical ventilation. The importance of disease and patient characteristics. Chest. 1996;110:469–79.
Huttner HB, Kohrmann M, Berger C, Georgiadis D, Schwab S. Predictive factors for tracheostomy in neurocritical care patients with spontaneous supratentorial hemorrhage. Cerebrovasc Dis. 2006;21:159–65.
Dellinger RP, Levy MM, Rhodes A, et al. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock, 2012. Intensive Care Med. 2013;39:165–228.
Riker RR, Picard JT, Fraser GL. Prospective evaluation of the Sedation–Agitation scale for adult critically ill patients. Crit Care Med. 1999;27:1325–9.
Simmons LE, Riker RR, Prato BS, Fraser GL. Assessing sedation during intensive care unit mechanical ventilation with the Bispectral Index and the Sedation–Agitation Scale. Crit Care Med. 1999;27:1499–504.
Sessler CN, Gosnell MS, Grap MJ, et al. The Richmond Agitation–Sedation Scale: validity and reliability in adult intensive care unit patients. Am J Respir Crit Care Med. 2002;166:1338–44.
Ely EW, Truman B, Shintani A, et al. Monitoring sedation status over time in ICU patients: reliability and validity of the Richmond Agitation–Sedation Scale (RASS). JAMA. 2003;289:2983–91.
Barry R, James MT. Guidelines for classification of acute kidney diseases and disorders. Nephron. 2015;131:221–6.
Walcott BP, Kamel H, Castro B, Kimberly WT, Sheth KN. Tracheostomy after severe ischemic stroke: a population-based study. J Stroke Cerebrovasc Dis. 2014;23:1024–9.
Pinheiro Bdo V, Tostes Rde O, Brum CI, Carvalho EV, Pinto SP, Oliveira JC. Early versus late tracheostomy in patients with acute severe brain injury. J Bras Pneumol. 2010;36:84–91.
Jüttler E, Unterberg A, Hacke W. Hemicraniectomy for middle-cerebral-artery stroke. N Engl J Med. 2014;370:2347–8.
R Core Team. R Foundation for Statistical Computing V, Austria. https://www.R-project.org/. R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. 2015. https://www.R-project.org/.
Sing T, Sander O, Beerenwinkel N, Lengauer T. ROCR: visualizing classifier performance in R. Bioinformatics. 2005;21:3940–1.
Warnes GR, Bolker B, Bonebakker L, Gentleman R, Huber W, Liaw A, Lumley T, Maechler M, Magnusson A, Moeller S, Schwartz M, Venables B. gplots: various R programming tools for plotting data. R package version 2.17.0. 2015. http://CRAN.R-project.org/package=gplots.
Dahl DB. xtable: export tables to LaTeX or HTML. R package version 1.7-4. 2014.
Qureshi AI, Suarez JI, Parekh PD, Bhardwaj A. Prediction and timing of tracheostomy in patients with infratentorial lesions requiring mechanical ventilatory support. Crit Care Med. 2000;28:1383–7.
Szeder V, Ortega-Gutierrez S, Ziai W, Torbey MT. The TRACH score: clinical and radiological predictors of tracheostomy in supratentorial spontaneous intracerebral hemorrhage. Neurocrit Care. 2010;13:40–6.
Rodriguez JL, Steinberg SM, Luchetti FA, Gibbons KJ, Taheri PA, Flint LM. Early tracheostomy for primary airway management in the surgical critical care setting. Surgery. 1990;108:655–9.
Bouderka MA, Fakhir B, Bouaggad A, Hmamouchi B, Hamoudi D, Harti A. Early tracheostomy versus prolonged endotracheal intubation in severe head injury. J Trauma. 2004;57:251–4.
Dunham CM, LaMonica C. Prolonged tracheal intubation in the trauma patient. J Trauma. 1984;24:120–4.
Rabinstein AA, Wijdicks EF. Outcome of survivors of acute stroke who require prolonged ventilatory assistance and tracheostomy. Cerebrovasc Dis. 2004;18:325–31.
Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13:818–29.
Murray JF, Matthay MA, Luce JM, Flick MR. An expanded definition of the adult respiratory distress syndrome. Am Rev Respir Dis. 1988;138:720–3.
Funding
This study was not funded.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Bösel received travel grants and speaker honoraria from Covidien and Sedana. Dr. Schönenberger, Dr. Al-Suwaidan, Dr. Kieser, and Mr. Uhlmann report no conflicts.
Rights and permissions
About this article
Cite this article
Schönenberger, S., Al-Suwaidan, F., Kieser, M. et al. The SETscore to Predict Tracheostomy Need in Cerebrovascular Neurocritical Care Patients. Neurocrit Care 25, 94–104 (2016). https://doi.org/10.1007/s12028-015-0235-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-015-0235-5