Abstract
Background
We aimed to investigate the feasibility, preliminary safety, and efficacy of prolonged low-dose intravenous thrombolysis in posterior circulation stroke patients with a thrombus lodged in the basilar artery who were ineligible for standard rtPA administration.
Methods
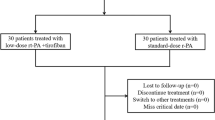
We retrospectively analyzed consecutively collected patients in our stroke database who suffered from a basilar artery thrombosis and were treated with prolonged (>1 h), intravenous, low-dose (≤20 mg) rtPA between 01/2005 and 11/2012.
Results
Patients included in this study (n = 14) were 68.5 years (IQR 55.5; 72.75) of age and presented with a median NIHSS of 2 (1; 5.25). Median time from symptom onset to treatment was 63 h (33; 141). A median dose of 5.21 μg/kg h (4.46; 6.25) rtPA was administered over 24 h (min 10; max 48). No patient experienced symptomatic intracerebral hemorrhage, one patient developed a spinal epidural hematoma, and two elderly patients were switched to comfort care and died. In eight patients (57 %) a decrease in thrombus size or no thrombus at all was detected on control imaging. Nine patients (64 %) had a favorable outcome (mRS 0–2) at day 90.
Conclusions
Prolonged low-dose thrombolysis with rtPA may be considered as individual treatment option in selected high-risk patients with basilar artery thrombosis. Presented data may lay the groundwork to further investigate safety and efficacy in a prospective trial.

Similar content being viewed by others
References
Mattle HP, Arnold M, Lindsberg PJ, Schonewille WJ, Schroth G. Basilar artery occlusion. Lancet Neurol. 2011;10:1002–14.
Veltkamp R, Jacobi C, Kress B, Hacke W. Prolonged low-dose intravenous thrombolysis in a stroke patient with distal basilar thrombus. Stroke. 2006;37:e9–11.
von Elm E, Altman DG, Egger M, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370:1453–7.
Hacke W, Kaste M, Fieschi C, et al. Randomised double-blind placebo-controlled trial of thrombolytic therapy with intravenous alteplase in acute ischaemic stroke (ECASS II). Second European–Australasian Acute Stroke Study Investigators. Lancet. 1998;352:1245–51.
Sairanen T, Strbian D, Soinne L, et al. Intravenous thrombolysis of basilar artery occlusion: predictors of recanalization and outcome. Stroke. 2011;42:2175–9.
Vergouwen MD, Algra A, Pfefferkorn T, et al. Time is brain (stem) in basilar artery occlusion. Stroke. 2012;43:3003–6.
Strbian D, Sairanen T, Silvennoinen H, Salonen O, Kaste M, Lindsberg PJ. Thrombolysis of basilar artery occlusion: impact of baseline ischemia and time. Ann Neurol. 2013;73(6):688–94.
Conflict of interest
CH, LK, SN, and RV report no conflicts and have nothing to disclose. WH and PR received speaker honoraria and travel expenses from Boehringer Ingelheim (manufacturer of Alteplase®).
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Hametner, C., Kellert, L., Veltkamp, R. et al. Prolonged Low-Dose Thrombolysis in Posterior Circulation Stroke. Neurocrit Care 21, 114–118 (2014). https://doi.org/10.1007/s12028-013-9891-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-013-9891-5