Abstract
Background
In the postpartum patient, sudden depression of consciousness may be caused by a number of etiologies and can result in serious consequences. Rapid, accurate diagnosis allows for specific treatments that optimize outcome, but diagnosis can be challenging in this population. We present a case of postpartum herniation due to intracranial hypotension in a patient with eclampsia, posterior reversible encephalopathy syndrome (PRES), and intracerebral hemorrhage (ICH).
Methods
Case report.
Results
A 26-year-old woman developed headache on postpartum day (PD) 1 after cesarean section with epidural anesthesia. Over the next 3 days, she developed progressively worsening headache and hypertension. On PD 5, she had a generalized seizure, leading to endotracheal intubation, propofol infusion, and transfer to our institution. By PD 6, she opened her eyes to voice, followed commands, moved all extremities, and had briskly reactive 4 mm pupils. MRI showed L parasagittal ICH with minimal mass effect, edema consistent with PRES, and brain descent with obliteration of the basal cisterns and tonsillar herniation. Later on PD 6, after diuresis for pulmonary edema, she became unresponsive with a dilated and nonreactive left pupil. She was laid flat for transport to CT, with improvement in arousal and pupil reactivity within 5 min. Intravascular volume was repleted with normal saline and albumin, and she was placed in the Trendelenburg position. Over the subsequent 8 h, she developed a dilated and nonreactive left pupil whenever her head was raised to horizontal. Her head position was gradually successfully raised over 48 h without need for a lumbar epidural blood patch. She was discharged home on PD 13 with only mild left arm dysmetria.
Conclusions
Intracranial hypotension may coexist with other potential causes of cerebral herniation in the postpartum period. Establishing this diagnosis is crucial because its treatment is opposite that of other causes of herniation.
Similar content being viewed by others
Introduction
Neurologic dysfunction, especially depressed consciousness, is common in critically ill obstetric patients and is associated with significant associated morbidity and mortality [1]. The wide diversity and unusual nature of the conditions associated with acutely depressed consciousness in the obstetric patient and the premium on rapid accurate diagnosis make this a challenging condition for neurologists in the intensive care unit (ICU). We present a case of postpartum cerebral herniation due to intracranial hypotension in a patient who had at the same time eclampsia, intracerebral hemorrhage (ICH), and posterior reversible encephalopathy syndrome (PRES). The unusual co-occurrence of these conditions in the same patient makes this case instructive for the clinical approach to this difficult problem.
Report of Case
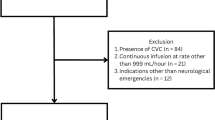
On postpartum day (PD) 6, we evaluated a 26-year-old woman without a significant past medical history who was transferred to our neurocritical care service from a community hospital ICU with intraparenchymal hemorrhage and seizure. The pregnancy was complicated by pre-eclampsia. She underwent cesarean section delivery for breach presentation with epidural anesthesia without significant complication. On PD 1, she developed the gradual onset of head and neck pain. Over the next 3 days, she developed a progressively worsening headache, but was otherwise neurologically intact and stable. On PD 4, she was noted to have severe hypertension with systolic blood pressures (SBP) in the 180 s mmHg. She was admitted to the community hospital ICU where a labetalol infusion was used to keep her SBP 140–160 mmHg. Late in the evening on PD 5, she had a brief generalized convulsive seizure with postictal depression of consciousness that lead to endotracheal intubation and sedation with propofol infusion. Emergent head CT showed a 3.2 × 2.2 × 2.5 cm (9.6 mL) ICH in the left parietal parafalcine region with perihematomal edema, but no associated tissue shifts. She was transferred to our institution a few hours later.
Upon our initial evaluation at 7 am on PD 6, she was afebrile, and the blood pressure was 127/84 mmHg. She was intubated and mechanically ventilated on the assist control mode, fraction of inspired oxygen (FiO2) of 50 % and positive end-expiratory pressure (PEEP) of 5 cm H2O with an oxygen saturation (SpO2) of 98 %. The medications included infusions of propofol (30 mcg/kg/min) and magnesium (2 g/h). The serum sodium concentration was 143 mEq/L. On neurologic examination, she was alert, opening her eyes and orienting to the examiner immediately to voice. She was able to consistently follow two-step commands and answered simple yes/no questions accurately by nodding or shaking her head. The cranial nerve examination was notable for conjugate left gaze preference, full visual fields, and 4 mm briskly reactive pupils. She moved all limbs normally. The muscle stretch reflexes were 3+ throughout and the toes were extensor bilaterally. The general medical examination was unremarkable. MRI of the brain, performed at 10 am on PD 6, showed that the hemorrhage was unchanged compared to the earlier CT (Fig. 1a, b). It also demonstrated bilaterally symmetric edema at the cortical-subcortical junction consistent with PRES (Fig. 2). There were no microhemorrhages on susceptibility-weighted sequences. MR angiography and venography were normal.
After the MRI, levetiracetam and a nicardipine infusion (target blood pressure 100–140/<90 mmHg) were started. At 1 pm on PD 6, we began to wean ventilatory support in anticipation of extubation. Within minutes of being changed to the pressure support (PS) mode with PEEP 5 cm H2O and PS 5 cm H2O, the SpO2 dropped to 90 % and the patient became tachypneic. An X-ray of the chest showed severe bilateral pulmonary edema. For this reason, she was placed back on her previous ventilator settings, the head of her bed was elevated to about 45°, and furosemide 20 mg was administered intravenously. Her oxygenation improved immediately, and within 1 h, she made 1,250 mL of urine.
Two hours later, she was noted to be unarousable by her nurse. On neurologic exam, she was somnolent, arousable only to sternal rub, not following commands. Her left pupil was dilated to 8 mm and nonreactive; the right pupil was 4 mm and reactive. She was moving all extremities semi-purposefully spontaneously. She was laid flat for transport to obtain emergent head CT. Within 5 min, her neurologic examination improved. She became alert, followed simple commands, her left pupil was 4.5 mm and reactive, right pupil 4 mm and reactive, and she was moving all extremities normally. The serum sodium concentration at this time was 136 mEq/L. Her head CT showed stable size of the intraparenchymal hemorrhage, stable effacement of bilateral perimesencephalic cisterns and the quadrigeminal plate cistern (Fig. 3a), and crowding of the structures at the foramen magnum (Fig. 3b). On review of her MRI from PD 6, features of intracranial hypotension were noted to already be present on T1 sagittal and FLAIR axial images as well (Fig. 4a, b). At this point, based on the radiographic findings and the favorable response to being transported with the head of the bed flat, we posited that her clinical herniation syndrome was due to intracranial hypotension and was not related to the ICH. To replete her intravascular volume, she was given a 500 mL bolus of 0.9 % sodium chloride solution and 50 mL of 25 % of albumin and the head of her bed was laid flat. Two hours after the initial decline in her exam, she was arousable, but somnolent, her left pupil was 6 mm and sluggishly reactive, and her right pupil remained at 4 mm and reactive. She was placed in the Trendelenburg position and within 5–10 min, her level of arousal improved and the left pupil became 4.5 mm and briskly reactive.
T1 weighted sagittal MRI demonstrating brain sagging in the setting of intracranial hypotension with compression of midbrain (thin arrows), obliteration of the prepontine cistern (thick arrow), and low lying cerebellar tonsils (dotted arrow) (a). FLAIR axial MRI through the region of the midbrain showing compression and elongation of the midbrain (arrows; b)
She was kept in the Trendelenburg position for the next 24 h, and her neurologic function remained stable despite a decline in the serum sodium concentration to its nadir at 134 mEq/L. Because her pulmonary status remained tenuous due to the inability to raise the head of the bed or diurese, a lumbar epidural blood patch was considered to facilitate extubation. This was delayed by the development of a fever and leukocytosis on PD 7. She was started on vancomycin and piperacillin/tazobactam and cultures were sent of blood, urine, and sputum. Oxygenation began to improve spontaneously over the course of that day. Beginning on PD 8, her head position was raised slowly, such that by PD 9, it was at 45° for many hours without any decline in neurologic function. She was successfully weaned from mechanical ventilation and extubated on PD 9. The neurologic examination after extubation was normal with the exception of brisk muscle stretch reflexes at 3+ throughout and mild dysmetria of the left limbs. Her toes were now flexor bilaterally. She was transferred out of the ICU on PD 9 and was discharged home on PD 13 with only mild left arm dysmetria and persistence of brisk muscle stretch reflexes throughout.
Discussion
Dysfunction of the nervous system has been described in up to 50 % of critically ill obstetric patients, the most common manifestation of which is altered consciousness. The range of potential underlying etiologies is broad, and rapid diagnosis and treatment are necessary to minimize the substantial morbidity and mortality associated with the development of a depressed level of consciousness in this generally young and healthy population [1]. The present case is instructive because it illustrates the presence of a number of these disorders (intracranial hypotension, seizure, ICH, PRES) simultaneously in the same patient as well as the diagnostic approach that allowed the most clinically relevant etiology to be identified and effectively treated.
The first neurologic disorder manifested by our patient was seizure, which was the result of eclampsia and PRES. An association between eclampsia and PRES has been described in the literature, but has yet to be well defined [2]. A recent study at the Mayo Clinic found that in all seven patients with a diagnosis of eclampsia between 2001 and 2008, there were imaging changes consistent with a diagnosis of PRES [3]. Notably, the risk for developing eclampsia or PRES persists following delivery, and delayed onset of eclamptic seizures may occur up to 6 weeks after delivery [4].
Intracerebral hemorrhage is an uncommon, but devastating complication of pregnancy. A recent study which used the Nationwide Inpatient Sample to review obstetric patients between 1993 and 2002 yielded 6,969,553 deliveries and found an incidence of ICH of 7.1/100,000 at-risk person per year. Independent risk factors included age greater than 35, African-American race, hypertension, coagulopathy, and tobacco or cocaine abuse. Over 50 % of these hemorrhages occurred in the postpartum period, 30 % were related to pre-eclampsia or eclampsia [5]. Of significance, approximately 60 % of ICHs related to pre-eclampsia or eclampsia occurred in the postpartum period [6]. Despite a relatively young population, outcomes were poor. Twenty percent of patients died prior to discharge, 30 % were discharged to a medical facility, and only 50 % were discharged directly home [5]. Fortunately for our patient, the hemorrhage itself seemed to cause relatively few problems.
Despite the presence of a mass lesion in the form of the ICH and the fact that the headache could have been due to this lesion or the eclampsia/PRES, we believe that intracranial hypotension was responsible for the herniation syndrome exhibited by our patient. First, she recently had epidural anesthesia. Second, the onset of herniation was in the midst of a brisk diuresis and significant head elevation, and it resolved nearly completely with no treatment other than lying the head flat and repleting the intravascular volume. Third, it is unlikely that the 9.6 mL parietal ICH, from which there was no associated local mass effect, caused herniation. Fourth, there are characteristic features of “brain sag” such as midbrain elongation, effacement of the prepontine cisterns, and low lying cerebellar tonsils as seen on the sagittal view of the admission MRI [7, 8]. Finally, this clinical picture has been well described to be caused by intracranial hypotension [9].
Our patient had epidural anesthesia 6 days prior to transfer to our institution with likely unrecognized accidental dural puncture. Accidental dural punctures (ADP) can go unrecognized at the time of epidural catheter insertion. In a 23-year survey in a district general hospital by Sprigge and Harper, ADP occurred in 0.91 % of cases [10]. In up to 36 % of cases, the anesthetist was unaware of the ADP at the time of insertion. This is similar to findings in other studies [11]. ADP resulted in postdural puncture headache (PDPH) in 88 % of the patients [10]. Other complications of ADP are not well reported in the literature and, to our knowledge, there are no reported cases of coma associated with ADP and intracranial hypotension.
Altered consciousness and coma as a result of intracranial hypotension from other causes, particularly spontaneous intracranial hypotension (SIH), have been reported [7]. SIH is typically characterized by a positional-type headache that improves when supine, but can lead to more severe complications. Imaging findings can help support the diagnosis. The findings on MRI can include meningeal enhancement, subdural fluid collections, small ventricles, and findings consistent with brain sagging such as midbrain elongation [7, 8]. Our patient had small ventricles and obliteration of the basal cisterns with midbrain elongation and downward displacement of the cerebellar tonsils.
Treatment of intracranial hypotension involves intravascular volume repletion, placing the patient in the recumbent position, and often requires an epidural blood patch. Other reported treatments in severe presentations of intracranial hypotension included use of intrathecal saline infusion and injection of glue [12, 13]. Use of an epidural blood patch was considered in our patient, but conservative management with placing the patient in the Trendelenburg position, hydration, and use of albumin to restore circulating volume was effective and a blood patch was not required. These treatments are very different, and in some ways opposite those that are used to treat herniation from the competing diagnoses of a mass-occupying ICH or diffuse cerebral edema from eclampsia and PRES. Cranial surgery with evacuation of the hematoma and/or craniectomy, for example, could exacerbate the downward herniation from intracranial hypotension [7]. Similarly, as one of the mainstays of intracranial hypotension treatment is intravascular volume repletion (with a theoretical goal of optimizing cerebrospinal fluid volume), treating cerebral edema from eclampsia and PRES with mannitol could possibly worsen intracranial hypotension by decreasing the cerebrospinal fluid volume.
In conclusion, this case illustrates many of the severe intracranial complications of pregnancy and delivery as well as the diagnostic and management challenges in postpartum patients with acute disorders of consciousness. It also demonstrates that intracranial hypotension may coexist with other potential causes of cerebral herniation in the postpartum period. Establishing this diagnosis is crucial because its treatment is opposite that of other causes of herniation.
References
Karnad DR, Guntupalli KK. Neurological disorders in pregnancy. Crit Care Med. 2005;33(10):S362–71.
Hinchey J, Chaves C, Appignani B, et al. A reversible posterior leukoencephalopathy syndrome. N Engl J Med. 1996;334(8):494–500.
Wagner SJ, Acquah LA, Lindell EP, et al. Posterior reversible encephalopathy syndrome and eclampsia: pressing the case for more aggressive blood pressure control. Mayo Clin Proc. 2011;86(9):851–6.
Al-Safi Z, Imudia AN, Filetti LC, et al. Delayed postpartum eclampsia and preeclampsia: demographics, clinical course and complications. Obstet Gynecol. 2011;118:1102–7.
Bateman BT, Schumacher HC, Bushnell CD, et al. Intracerebral hemorrhage in pregnancy: frequency, risk factors and outcome. Neurology. 2006;67:424–9.
Kittner SJ, Stern BJ, Feeser BR, et al. Pregnancy and the risk of stroke. N Engl J Med. 1996;335:768–74.
Komotar RJ, Mocco J, Ransom ER, et al. Herniation secondary to postcraniotomy cerebrospinal fluid hypovolemia. Neurosurgery. 2005;57:286–92.
Binder DK, Dillon WP, Fishman RA, Schmidt MJ. Intrathecal saline infusion in the treatment of obtundation associated with spontaneous intracranial hypotension: technical case report. Neurosurgery. 2002;51:830–7.
Dhillon AK, Rabinstein AA, Wijdicks EFM. Coma from worsening spontaneous intracranial hypotension after subdural hematoma evacuation. Neurocrit Care. 2010;12:390–4.
Sprigge JS, Harper SJ. Accidental dural puncture and post dural puncture headache in obstetric anaesthesia: presentation and management: a 23-year survey in a district general hospital. Anaesthesia. 2008;63:36–43.
Van de Velde M, Schepers R, Berends N, et al. Ten years of experience with accidental dural puncture and post-dural puncture headache in a tertiary obstetric anaesthesia department. Int J Obstet Anesth. 2009;17:329–35.
Spelle L, Boulin A, Tainturier C, et al. Neuroimaging features of spontaneous intracranial hypotension. Neuroradiology. 2001;43:622–7.
Schievink WI, Moser FG, Pikul BK. Reversal of coma with an injection of glue. Lancet. 2007;369:1402.
Conflict of interest
The authors report no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Orehek, E.K., Burns, J.D., Koyfman, F. et al. Postpartum Trifecta: Simultaneous Eclamptic Intracerebral Hemorrhage, PRES, and Herniation Due to Intracranial Hypotension. Neurocrit Care 17, 434–438 (2012). https://doi.org/10.1007/s12028-012-9742-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-012-9742-9