Abstract
Background
Preoperative antibiotic prophylaxis remains one of the most important strategies for prevention of postoperative infection. In patients with penicillin allergy, alternative medications such as vancomycin are often used despite reduced antimicrobial coverage and recent literature questioning the efficacy of vancomycin monotherapy.
Questions/purposes
(1) Are patients who receive vancomycin alone for penicillin allergy at greater odds of developing surgical site infection (SSI) as compared with patients who receive cefazolin for prophylaxis before total joint arthroplasty (TJA) without a patient-reported allergy? (2) What organism profile is associated with vancomycin monotherapy?
Methods
We performed a retrospective study of 10,391 primary TJAs performed between 2005 and 2014 at two institutions with a minimum of 1-year followup. Patients reporting penicillin or cephalosporin allergy were electronically queried from the anesthesia note. The odds of deep SSI and causative organisms were compared using multivariate analysis between β-lactam-allergic patients receiving vancomycin and nonallergic patients receiving cefazolin.
Results
After controlling for potential confounders, including comorbidities, we found that vancomycin alone did not affect the odds of deep SSI development (adjusted odds ratio [OR], 0.98; 95% confidence interval [CI], 0.67–1.43; p = 0.907). Although the overall odds of deep SSI were not different for patients receiving vancomycin versus cefazolin, we found that vancomycin was associated with a reduced risk of infection with Gram-positive organisms (adjusted OR, 0.25 [CI, 0.10–0.62]; p = 0.003) and antibiotic-resistant organisms (adjusted OR, 0.10 [CI, 0.01–0.88]; p = 0.038). Vancomycin also demonstrated an increased risk of Gram-negative infection in bivariate analysis (OR, 2.42 [CI, 1.01–5.82]; p = 0.049) compared to cefazolin.
Conclusions
With the numbers available, vancomycin alone during elective primary TJA does not seem to result in a higher rate of subsequent deep SSI. However, patients who received vancomycin alone demonstrated reduced odds of Gram-positive organisms and methicillin-resistant Staphylococcus aureus. Vancomycin monotherapy can be used without increasing the risk of deep SSI; however, it should only be used in patients who require vancomycin, eg, anaphylactic reactions to penicillin resulting from the potential for the emergence of organism resistance and nephrotoxicity. Future studies are needed that use registry and large database studies to refute or confirm the preliminary findings of this study and determine if vancomycin monotherapy influences the risk of periprosthetic joint infection.
Level of Evidence
Level III, therapeutic study.
Similar content being viewed by others
Introduction
Current guidelines recommend that a first- or second-generation cephalosporin (cefazolin or cefuroxime) be primarily used because commensal Gram-positive bacteria remain the most likely infecting organisms [1, 4, 9]. However, when patients have a penicillin or β-lactam allergy, first- and second-generation cephalosporins often are avoided because of fears of crossreactivity. Instead, vancomycin and clindamycin are recommended alternatives, especially in patients with severe allergy or true anaphylaxis. However, clindamycin alone is only bacteriostatic, and vancomycin alone has reduced Gram-negative coverage and may thus be associated with increased infection rates.
Although many studies have compared the efficacy of vancomycin with cefazolin for preventing periprosthetic joint infection (PJI), the results have been mixed with some studies achieving excellent results with vancomycin alone [11–13, 16], but a recent large study suggested that vancomycin monotherapy is associated with increased risk of infection compared with cefazolin [11].
We therefore asked: (1) Are patients who receive vancomycin alone for penicillin allergy at greater odds of developing deep surgical site infection (SSI) as compared with nonallergic patients who receive cefazolin for prophylaxis before total joint arthroplasty (TJA)? (2) What organism profile is associated with vancomycin monotherapy?
Patients and Methods
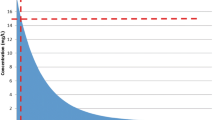
After institutional review board approval, a retrospective multiinstitutional study was performed on primary TJAs from January 2005 to November 2014 at two different institutions. During the period in question, we used vancomycin in patients with a reported allergy to penicillin or a cephalosporin of any severity and other patients received cephalosporins. Patients with unavailable antibiotic information, on multiple antibiotics or antibiotics other than cefazolin for nonallergic patients or vancomycin without a patient-reported penicillin or cephalosporin allergy, or who had less than 1 year of followup were excluded. Patients who developed SSI were included in the analysis regardless of whether the 1-year criteria were met (Table 1). Patients with any allergy to a cephalosporin or any penicillin-containing antibiotics who received vancomycin were placed in the allergic cohort. From a total of 13,003 primary TJAs, 1132 TJAs did not have the minimum of 1-year followup including 804 in the cefazolin cohort and 328 in the vancomycin cohort, and 1480 TJAs were excluded for other reasons. The final cohort thus consisted of 10,391 primary TJAs, including 7734 primary TJAs for which cefazolin was used in the nonallergic cohort and 2657 patients who received vancomycin in the penicillin- or cephalosporin-allergic cohort (Fig. 1). Patients who received simultaneous or staged bilateral were considered to have two TJAs. Of the 10,391 TJAs, 53.8% (n = 5589) were TKAs. The mean duration of followup was 39 months (range, 12–117 months) in the nonpenicillin-allergic group and 40 months (range, 12–118 months) in the penicillin-allergic cohort (p = 0.59).
Antibiotic Characteristics and Protocol
Collaboration of the two institutions involved in this study resulted from identical protocols for administering vancomycin in penicillin- and cephalosporin-allergic patients regardless of the severity of the allergic reaction. In patients without a contraindication to a cephalosporin or penicillin allergy, cefazolin was administered preoperatively at a dose of 1 to 2 g intravenously before skin incision based on the patient’s weight. In cases of renal disease, doses were renally adjusted. In contrast, 1 g vancomycin was administered to patients with an allergy to penicillin or cephalosporin over 1 to 2 hours of infusion, which was generally completed 1 hour before skin incision. Routine testing for penicillin allergy or administration of dual antibiotic coverage when using vancomycin was not performed. Antibiotic cement was used at both institutions for all TKAs, whereas all THAs were cementless.
Outcome Variables
The following variables were identified: perioperative antibiotic used, joint involvement, patient allergies, demographic information, and comorbidities, as assessed by the Charlson Comorbidity Index [7]. Deep SSI was initially assessed using International Classification of Diseases, 9th Revision (996.6, 996.66, and 996.67) followed by a manual review of the medical record to confirm that a deep SSI was suspected and to obtain the causative organism and date of infection. Deep SSI was defined as infection relating to the TJA operation that involves deep soft tissues (eg, fascial and muscle layers) of the incision. All organism information was obtained from intraoperative fluid and representative tissue culture results. Organisms were subsequently categorized into the following categories: Gram-positive, Gram-negative, resistant organisms, and culture-negative organisms, which is defined as an inability to isolate the infecting organism. Resistant organisms were defined as methicillin-resistant Staphylococcus aureus (MRSA) and vancomycin-resistant Enterococcus (VRE).
Statistical Analysis
Multiple logistic regression analysis was used to determine the independent contribution of the antibiotic group on the development of SSI. The multivariate analysis controlled for the following factors: age, body mass index, institutional site, gender, joint, year of surgery, and Charlson Comorbidity Index. The predictive models were pruned using the Akaike Information Criterion so that only variables associated with the outcome remained. A Fisher’s exact test was also used to evaluate differences in the SSI risk. All statistical analyses were performed using R 2.15.1 (R Foundation for Statistical Computing, Vienna, Austria) using the RMS (regression modeling strategies) package for logistic regression. An alpha level of 0.05 was used to evaluate significance. Using a priori power analysis with the observed proportions in this study and a power of 0.8, a sample size of 164,432 (82,216 in each group) would be needed.
Results
After controlling for potential confounders, including comorbidities, we found that the use of vancomycin alone did not affect the odds of deep SSI development (adjusted odds ratio [OR], 0.98; 95% confidence interval [CI], 0.67–1.43; p = 0.907; Table 2). In addition, when separated by year intervals of surgery, there was no difference between the two groups (Table 3).
Although the overall odds of deep SSI were not different for patients receiving vancomycin versus cefazolin, multivariate analysis controlling for relevant confounding variables demonstrated that vancomycin was associated with a reduced risk of infection with Gram-positive organisms (adjusted OR, 0.25 [CI, 0.10–0.62]; p = 0.003) and antibiotic-resistant organisms (adjusted OR, 0.10 [CI, 0.01–0.88]; p = 0.038 (Table 4). There were no cases of VRE in either cohort. Interestingly, the rate of culture-negative deep SSI was not affected by the preoperative antibiotic administered (adjusted OR, 1.27; 95% CI, 0.41–3.91; p = 0.681). Although vancomycin did not demonstrate an increased risk of Gram-negative infection in the multivariate analysis (adjusted OR, 2.48; 95% CI, 0.82–7.55; p = 0.108), the bivariate analysis demonstrated an increased risk (OR, 2.42; 95% CI, 1.01–5.82; p = 0.049; Table 4).
Discussion
Currently, the American Academy of Orthopaedic Surgeons recommends vancomycin as antibiotic prophylaxis for patients with a β-lactam allergy or known colonization with MRSA, at facilities with recent MRSA outbreaks, or a MRSA prevalence of 10% to 20% [1]. β-lactam allergy is very common, and vancomycin or clindamycin is frequently substituted for cefazolin in these patients. However, there have been increasing concerns that the use of vancomycin as the sole agent may not be as effective as currently approved cephalosporins as a result of its narrower coverage [11, 16]. Thus, we aimed to better elucidate differences in the risk of deep SSI and the organism profile of penicillin- or cephalosporin-allergic patients receiving vancomycin compared with nonallergic patients who received cefazolin.
This study had a number of limitations. First, the lack of difference in the present study is likely the result of the fact that we were underpowered, because the power analysis demonstrated that a sample size of 164,432 TJAs was needed to demonstrate a difference in risk of deep SSI between the two antibiotic groups. Second, deep SSI was evaluated in this study as a surrogate for PJI, although PJI has a more impactful endpoint. However, because deep SSI was used rather than superficial SSI, superficial infections such as cellulitis were excluded. Future studies with larger sample sizes such as registry and database studies are needed to refute or confirm the preliminary findings of this study with respect to PJI rather than deep SSI. Third, differences in the organism profile may be reflective of different hospital antibiograms. Fourth, vancomycin was administered to any patient with a β-lactam allergy regardless of the severity of the reaction, which may represent a different population and result in different outcomes from institutions that administer vancomycin exclusively to patients with true anaphylaxis. Fifth, the dose and timing of the antibiotic could not be obtained for the cohort. This is especially important because 1 g vancomycin is frequently given rather than adjusting the dose by weight (15 mg/kg) [5]. Many patients may thus have been underdosed, which unfortunately could not be assessed. Sixth, as a result of the retrospective nature, it was difficult to determine which patients received vancomycin as a result of a history of MRSA or nasal colonization. However, we tried to exclude these patients by excluding non-β-lactam-allergic patients who received vancomycin. Seventh, of the two institutions involve in the study, one used a MRSA screening and decolonization protocol that may have influenced the results of the study. In addition, the rate of MRSA SSI was different between the two institutions (11% versus 23%). These institutional differences were, at least in part, controlled for in the multivariate analysis as we controlled for institutional site. Eighth, like with any study on perioperative antibiotics, attributing the perioperative antibiotic prophylaxis to the development of deep SSI is difficult given the multifactorial nature of deep SSI, and potential confounders may exist despite our best efforts to control for them. Lastly, deep SSI was the only endpoint studied and mortality and other outcomes such as salvage procedures, although interesting, were not explored.
Administering vancomycin alone was not associated with a higher proportion of patients developing deep SSI. Many prior studies have compared vancomycin with cephalosporins and have demonstrated conflicting results [11–13, 16]. These studies are rarely focused on the β-lactam-allergic population and frequently represent the outcomes of universally administering vancomycin. In a series of 5,036 primary TJAs, Smith et al. [13] found that transitioning from cefazolin to vancomycin resulted in a significant reduction of PJI from 1% to 0.5% [13]. Tyllianakis et al. [16] demonstrated no difference (six of 188 versus six of 120) in the SSI or PJI rate between those receiving cefuroxime and vancomycin in a prospective randomized trial in nonpenicillin-allergic patients. Sewick et al. [12] evaluated the use of dual antibiotics (vancomycin and cefazolin) with cefazolin monotherapy and found no difference in the infection rate (1.1% versus 1.4%; p = 0.64). In contrast, Ponce et al. [11] revealed that vancomycin (2.3%) demonstrated an approximately two times higher rate of 30-day SSI than cefazolin (1.3%, adjusted OR 1.73) and clindamycin (1.1%). Additionally, a subanalysis of patients with penicillin allergy found that the SSI rate was 2% in vancomycin alone compared with 1% in penicillin-allergic patients receiving clindamycin (p = 0.18) and 1.3% in cefazolin patients. Unlike Ponce et al.’s study, we could not demonstrate any difference in the risk of penicillin-allergic patients despite controlling for comorbidities and potential confounders.
Differences in the causative organisms between vancomycin and cefazolin have been well documented. Smith et al. [13] found that vancomycin alone was associated with reduced PJI with coagulase-negative Staphylococcus (0.07% versus 0.54%, p = 0.001) and MRSA (0.07% versus 0.23%, p = 0.14) compared with cefazolin alone Similarly, Sewick et al. [12] revealed that the rate of MRSA SSI was 10-fold more likely to occur in patients treated with cefazolin alone compared with vancomycin and cefazolin. Additionally, in a study of 885 patients undergoing cardiac surgery, patients receiving vancomycin were more likely to be infected with methicillin-sensitive S aureus, whereas patients receiving cefazolin developed increased infection with MRSA [8]. Although several studies, including the present study, have demonstrated that MRSA is reduced in patients with vancomycin, no studies to our knowledge have observed a reduced rate of Gram-positive organism. This finding can likely be explained by the narrower coverage of vancomycin compared with cefazolin and is important because infection with organisms other than Gram-positives such as atypical organisms and Gram-negative infection has been associated with poor treatment outcomes [10, 17]. Because of the potential for narrower coverage, another antibiotic can be added such as cefazolin or teicoplanin, which is commonly done in Europe, or monotherapy with antibiotics of broader coverage such as aztreonam, levofloxacin, or clindamycin. Despite the reduction in the rate of MRSA and the lack of VRE observed in this study, vancomycin should be used with caution in penicillin-allergic patients as a result of the potential for the emergence of organism resistance, most notably VRE and vancomycin-resistant S aureus [6], and its potential for nephrotoxicity. Thus, we encourage that vancomycin be reserved for patients that require vancomycin such as those with true anaphylaxis because the relative risk of anaphylaxis to a cephalosporin is rare in patient with a penicillin allergy history, ranging from one in 1000 to one in 1,000,000 [2]. In addition, skin testing can be a useful tool in distinguishing allergy and guiding antibiotic selection. Although skin testing penicillin-allergic patients cannot reliably predict an allergic response to cephalosporins with dissimilar side chains such as cefazolin, it can help identify whether a true allergy to penicillin exists in patients with a reported hypersensitivity, because a negative test result can reliably predict who can receive the antibiotic [3, 9, 14, 15].
In summary, the administration of perioperative prophylactic vancomycin alone during elective primary TJA does not seem to result in a higher rate of subsequent deep SSI with the numbers available. However, patients who received vancomycin alone demonstrated reduced odds of Gram-positive organisms and MRSA. Vancomycin monotherapy can be used without increasing the risk of SSI; however, it should only be used in patients who require vancomycin, eg, anaphylactic reactions to penicillin, or MRSA carriers resulting from the potential for nephrotoxicity and the emergence of organism resistance. Future studies are needed that use registry and large database studies to refute or confirm the preliminary findings of this study and determine if vancomycin monotherapy influences the actual PJI risk.
References
American Academy of Orthopaedic Surgeons. Recommendations for the use of intravenous antibiotic prophylaxis information statement. Available at: http://www.aaos.org/about/papers/advistmt/1027.asp. Accessed September 12, 2015.
Apter AJ, Kinman JL, Bilker WB, Herlim M, Margolis DJ, Lautenbach E, Hennessy S, Strom BL. Is there cross-reactivity between penicillins and cephalosporins? Am. J. Med. 2006;119:354.e11–19.
Audicana M, Bernaola G, Urrutia I, Echechipia S, Gastaminza G, Muñoz D, Fernández E, Fernández de Corres L. Allergic reactions to betalactams: studies in a group of patients allergic to penicillin and evaluation of cross-reactivity with cephalosporin. Allergy. 1994;49:108–113.
Bratzler DW, Houck PM, Surgical Infection Prevention Guideline Writers Workgroup. Antimicrobial prophylaxis for surgery: an advisory statement from the National Surgical Infection Prevention Project. Am J Surg. 2005;189:395–404.
Catanzano A, Phillips M, Dubrovskaya Y, Hutzler L, Bosco J. The standard one gram dose of vancomycin is not adequate prophylaxis for MRSA. Iowa Orthop J. 2014;34:111–117.
Centers for Disease Control and Prevention. CDC–VISA/VRSA in Healthcare Settings–HAI. Available at: http://www.cdc.gov/HAI/organisms/visa_vrsa/visa_vrsa.html. Accessed September 12, 2015.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383.
Finkelstein R, Rabino G, Mashiah T, Bar-El Y, Adler Z, Kertzman V, Cohen O, Milo S. Vancomycin versus cefazolin prophylaxis for cardiac surgery in the setting of a high prevalence of methicillin-resistant staphylococcal infections. J Thorac Cardiovasc Surg. 2002;123:326–332.
Hansen E, Belden K, Silibovsky R, Vogt M, Arnold W, Bicanic G, Bini S, Catani F, Chen J, Ghazavi M, Godefroy KM, Holham P, Hosseinzadeh H, Kim KII, Kirketerp-Møller K, Lidgren L, Lin JH, Lonner JH, Moore CC, Papagelopoulos P, Poultsides L, Randall RL, Roslund B, Saleh K, Salmon JV, Schwarz E, Stuyck J, Dahl AW, Yamada K. Perioperative antibiotics. J Orthop Res. 2014;32(Suppl 1):S31–59.
Hsieh P-H, Lee MS, Hsu K-Y, Chang Y-H, Shih H-N, Ueng SW. Gram-negative prosthetic joint infections: risk factors and outcome of treatment. Clin Infect Dis. 2009;49:1036–1043.
Ponce B, Raines BT, Reed RD, Vick C, Richman J, Hawn M. Surgical site infection after arthroplasty: comparative effectiveness of prophylactic antibiotics: do surgical care improvement project guidelines need to be updated? J Bone Joint Surg Am. 2014;96:970–977.
Sewick A, Makani A, Wu C, O’Donnell J, Baldwin KD, Lee G-C. Does dual antibiotic prophylaxis better prevent surgical site infections in total joint arthroplasty? Clin Orthop Relat Res. 2012;470:2702–2707.
Smith EB, Wynne R, Joshi A, Liu H, Good RP. Is it time to include vancomycin for routine perioperative antibiotic prophylaxis in total joint arthroplasty patients? J Arthroplasty. 2012;27:55–60.
Solensky R, Earl HS, Gruchalla RS. Penicillin allergy: prevalence of vague history in skin test-positive patients. Ann Allergy Asthma Immunol. 2000;85:195–199.
Solensky R, Earl HS, Gruchalla RS. Lack of penicillin resensitization in patients with a history of penicillin allergy after receiving repeated penicillin courses. Arch Intern Med. 2002;162:822–826.
Tyllianakis ME, Karageorgos AC, Marangos MN, Saridis AG, Lambiris EE. Antibiotic prophylaxis in primary hip and knee arthroplasty: comparison between cefuroxime and two specific antistaphylococcal agents. J Arthroplasty. 2010;25:1078–1082.
Zmistowski B, Fedorka CJ, Sheehan E, Deirmengian G, Austin MS, Parvizi J. Prosthetic Joint Infection Caused by Gram-Negative Organisms. J Arthroplasty. 2011;26:104–108.
Acknowledgments
We thank Bryce Van Doren MPA, MPH, and Susan Odum PhD, of OrthoCarolina Research Institute and Mitchell Maltenfort PhD, of Rothman Institute for their extensive efforts in making this study possible.
Author information
Authors and Affiliations
Corresponding author
Additional information
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at Rothman Institute at Thomas Jefferson University, Philadelphia, PA, USA, and OrthoCarolina, Charlotte, NC, USA.
About this article
Cite this article
Tan, T.L., Springer, B.D., Ruder, J.A. et al. Is Vancomycin-only Prophylaxis for Patients With Penicillin Allergy Associated With Increased Risk of Infection After Arthroplasty?. Clin Orthop Relat Res 474, 1601–1606 (2016). https://doi.org/10.1007/s11999-015-4672-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-015-4672-4