Abstract
Background
Musculoskeletal injury is the most common reason that soldiers are medically not ready to deploy. Understanding intrinsic risk factors that may place an elite soldier at risk of musculoskeletal injury may be beneficial in preventing musculoskeletal injury and maintaining operational military readiness. Findings from this population may also be useful as hypothesis-generating work for particular civilian settings such as law enforcement officers (SWAT teams), firefighters (smoke jumpers), or others in physically demanding professions.
Questions/purposes
The purposes of this study were (1) to examine whether using baseline measures of self-report and physical performance can identify musculoskeletal injury risk; and (2) to determine whether a combination of predictors would enhance the accuracy for determining future musculoskeletal injury risk in US Army Rangers.
Methods
Our study was a planned secondary analysis from a prospective cohort examining how baseline factors predict musculoskeletal injury. Baseline predictors associated with musculoskeletal injury were collected using surveys and physical performance measures. Survey data included demographic variables, injury history, and biopsychosocial questions. Physical performance measures included ankle dorsiflexion, Functional Movement Screen, lower and upper quarter Y-balance test, hop testing, pain provocation, and the Army Physical Fitness Test (consisting of a 2-mile run and 2 minutes of sit-ups and push-ups). A total of 320 Rangers were invited to enroll and 211 participated (66%). Occurrence of musculoskeletal injury was tracked for 1 year using monthly injury surveillance surveys, medical record reviews, and a query of the Department of Defense healthcare utilization database. Injury surveillance data were available on 100% of the subjects. Receiver operator characteristic curves and accuracy statistics were calculated to identify predictors of interest. A logistic regression equation was then calculated to find the most pertinent set of predictors. Of the 188 Rangers (age, 23.3 ± 3.7 years; body mass index, 26.0 ± 2.4 kg/m2) remaining in the cohort, 85 (45.2%) sustained a musculoskeletal injury of interest.
Results
Smoking, prior surgery, recurrent prior musculoskeletal injury, limited-duty days in the prior year for musculoskeletal injury, asymmetrical ankle dorsiflexion, pain with Functional Movement Screen clearing tests, and decreased performance on the 2-mile run and 2-minute sit-up test were associated with increased injury risk. Presenting with one or fewer predictors resulted in a sensitivity of 0.90 (95% confidence interval [CI], 0.83–0.95), and having three or more predictors resulted in a specificity of 0.98 (95% CI, 0.93–0.99). The combined factors that contribute to the final multivariable logistic regression equation yielded an odds ratio of 4.3 (95% CI, 2.0–9.2), relative risk of 1.9 (95% CI, 1.4–2.6), and an area under the curve of 0.64.
Conclusions
Multiple factors (musculoskeletal injury history, smoking, pain provocation, movement tests, and lower scores on physical performance measures) were associated with individuals at risk for musculoskeletal injury. The summation of the number of risk factors produced a highly sensitive (one or less factor) and specific (three or more factors) model that could potentially be used to effectively identify and intervene in those persons with elevated risk for musculoskeletal injury. Future research should establish if screening and intervening can improve musculoskeletal health and if our findings among US Army Rangers translate to other occupations or athletes.
Level of Evidence
Level II, prognostic study.
Similar content being viewed by others
Introduction
Musculoskeletal injury is the leading reason soldiers are medically not ready for combat deployment and the leading cause of disability in military service members [24, 34]. These injuries are one of the most significant threats to military readiness. They also account for approximately 2.4 million medical visits and USD 548 million in direct patient care costs [12, 31]. This translates into over 25 million limited-duty days and over 900,000 service members affected each year [12, 31]. In elite military units that that often deploy in small groups, consequences of musculoskeletal injury are amplified. A single musculoskeletal injury resulting in a soldier medically not ready to deploy can have a devastating effect on the integrity of the team.
The negative impact remains high during deployment in support of combat missions, where the majority of injuries are actually not combat-related trauma. In fact, nonbattle injuries (NBIs) are historically the most common reason (approximately 86.5%) for medical evacuations [10, 11]. More recent data indicate that between 2001 and 2012, evacuations from the Iraq/Afghanistan areas of operations for NBI accounted for 50.3% [3]. This was the second leading cause of medical evacuation. Of the total 23,719 evacuations in this date range, one in seven (14.3%) were for musculoskeletal disorders, and the majority of these were for back and knee injuries [3]. Early in the conflict, the majority of NBIs requiring evacuation were musculoskeletal and related to preexisting conditions [11]. Injury incidence rates for those who are specifically infantry or special forces units are even higher at approximately 10 to 12 injuries per 100 soldier-months [15]. It is proposed that a portion of the musculoskeletal injuries may be prevented [27], and preliminary work in civilian populations supports this concept [1, 32, 35].
Although the consequences differ, professional athletes–the civilian analogue, perhaps, of the military’s elite units–are also at substantial risk for musculoskeletal injury, which analogously impacts organizational readiness. The financial implications injuries have on the professional sports sector has made proper identification and treatment of these injuries a research priority. Therefore, transitioning this focus over to assess military populations is the next logical step. Initial research on the use of a combination of physical performance and functional movement screens to identify intrinsic risk factors for future injury has been successful [24]. However, whether this approach is feasible and will prove helpful in terms of predicting injuries in soldiers is yet to be answered. If modifiable intrinsic risk factors for injury can be identified early, then targeted interventions can be implemented and may reduce future injury rates.
Therefore, the objectives of this study were to: (1) examine whether musculoskeletal injury risk can be determined using self-report and physical performance/movement-based examination items; and (2) to determine if a combination of items would enhance the accuracy for determining future musculoskeletal injury risk in US Army Rangers.
Materials and Methods
Study Design
The study was a planned secondary analysis from a large prospective cohort of 1477 soldiers that tracked injuries over the course of a year. The study was completed across a variety of military specialties (Rangers, Combat, Combat Service, and Combat Service Support military units) chosen to perform a battery of tests that included dorsiflexion ROM measurement, the Functional Movement Screen, the Y-balance test lower and upper quarter, and the triple crossover hop for distance between July and August 2011. The analyzed cohort in this study consisted of US Army Rangers recruited through group briefings established to inform soldiers about the relationship between physical performance and injuries. Of 320 Rangers briefed about our study, 211 were eligible, interested in participating, and completed baseline data collection (Fig. 1). Throughout the 1-year followup period, three (1.0%) participants requested to be withdrawn from the study. Medical records review revealed that one (0.3%) participant had been previously injured and was seeking medical care at the time of enrollment and was therefore removed from the analysis, resulting in a sample of 207 at 1-year followup. An additional 19 (9.2%) participants self-reported an injury that either (1) did not result in medical care; or (2) sought care for an injury that was not comprehensive or overuse in nature. These 19 subjects were removed from the final analyses because our focus was on comprehensive or overuse injuries, which have a stronger potential for risk mitigation strategies. Of the 188 participants analyzed (age, 23.3 ± 3.7 years; body mass index, 26.0 ± 2.4 kg/m2; Fig. 1), 103 (55%) remained uninjured and 85 (45%) had a comprehensive or overuse injury. Time in military service ranged from less than 1 year (n = 30 [16%]), between 1 and 3 years (n = 62 [33%]), between 3 and 5 years (n = 69 [37%]), between 5 and 10 years (n = 23 [12%]), to more than 10 years (n = 4 [2%]). Rangers are a specialized subset of soldiers in the US Army that conducts special operations missions, traditionally airborne or air assault, to seize key terrain such as airfields and other strategic facilities. Their selection process is rigorous and their training is some of the most physically and mentally demanding in the military.
All subjects were fluent in written and verbal English and between the ages of 18 and 45 years. Participants were excluded if they were on limited-duty status during the past 30 days as a result of physical limitations; were unable to participate in routine physical training; had cardiac, pulmonary, balance or visual impairments; neurological disorders; or had plans to leave the military in the next 12 months. The institutional review board at Madigan Army Medical Center, Fort Lewis, WA, USA, granted approval for the study.
Baseline Data Collection
After obtaining participant informed consent, data were collected during a single session that involved the completion of multiple tests at a series of stations. This included subjective self-report surveys examining individual lifestyle and history of injury followed by the series of physical performance and functional movement tests. These tests included the closed chain dorsiflexion ROM measurement, the Functional Movement Screen, the Y-balance test lower and upper quarter, and the triple crossover hop for distance. In addition to these measures, results from the most recent Army Physical Fitness Test was collected. Further description of these tests is outlined subsequently and has been reported previously [33, 39, 40].
The closed chain ankle dorsiflexion ROM assessed distal lower extremity mobility. Measurements were taken with the subject half kneeling based on the position of tibial advancement while the heel maintains contact with the ground. Previous research on the measurement of ankle dorsiflexion has reported good interrater (intraclass correlation coefficient [ICC] = 0.82) and intrarater reliability (ICC = 0.89–0.97) [20, 21].
The Functional Movement Screen screens for major movement limitations and asymmetry and is broken down into several movement tests. These were performed at multiple stations by trained raters. The individual tests included the deep squat, in-line lunge, hurdle step, shoulder mobility, active straight leg raise, trunk stability push up, and rotary stability. Performance was scored using the checklist scoring method for improved reliability [7]. The standard 0 to 3 score on the Functional Movement Screen was used for testing where a 0 indicates pain during the test, a 1 indicates complete inability to perform the test, a 2 indicates ability to perform the test with compensation, and a 3 indicates the ability to perform the test in the most challenging fashion without any movement deviations. The Functional Movement Screen has good interrater (ICC = 0.74) and intrarater (ICC = 0.76) reliability with trained raters in military populations [40]. Joint clearing tests are part of this screen and were performed to determine if end range pain was present in the lower extremity, trunk, or shoulder complex.
The lower quarter Y-balance requires dynamic lower extremity balance and is used to identify deficits related to risk of injury and motor control changes that occur after injury [10]. This balance test examines how far an individual can reach with the lower limb in three independent directions (anterior, posteromedial, and posterolateral) while maintaining a unilateral stance. The test is performed on each limb and the overall reach is normalized to the limb length of the subject (inferior anterosuperior iliac spine to inferomedial malleolus) measured while lying down. Each subject was provided six practice trials followed by three actual performance trials. The maximum score for each limb and reach direction was used for analysis. The lower quarter Y-balance test has shown high interday reliability (ICC = 0.80–0.85) in military populations [33].
The upper quarter Y-balance test requires upper quadrant mobility and stability that has been shown to correlate to shoulder stability and core strength measures in military subjects [44]. Similar to the lower quarter test, the upper quarter test examines how far an individual can reach while maintaining balance. However, with this test the subject is required to maintain balance while in a three-point plank position (one arm, two legs) while reaching with the unweighted upper extremity. The reach directions are in the medial, superolateral, and inferolateral directions. The maximum reach in each direction is normalized to the upper quarter limb length (spinous process of C7 to tip of the longest finger measured in 90° of abduction while standing). Each subject performed two practice trials to become familiar with the test. The practice trials were followed by three recorded performance trials. The maximum reach for each limb and direction was used for analysis. The upper quarter Y-balance has high between-day reliability among active adults (ICC = 0.88–0.99) and military populations (ICC = 0.91–0.92) [9, 44].
Triple hop requires lower extremity strength, power, and agility. Each subject performed three sequential hops without a pause while alternating across a 15.24-cm-wide line for each hop with the goal of hopping as far forward as possible without making contact with the line. Three trials were performed on each limb and the total distance hopped during each trial was recorded. The maximum best score on the test was used for analysis. Good reliability of the triple hop tests (ICC = 0.78–0.93) has been found when used in military populations [36].
The Army Physical Fitness Test is the standard assessment of fitness for soldiers in the US Army [13]. This test consists of three events: sit-ups, push-ups, and 2-mile run time. The scores are normalized to gender and age to establish performance standards. The most current test score was used for analysis. A minimum score of 60 on each test is a US Army standard requirement to pass the test [13] with the maximum score on each test being 100. Rangers have a minimum benchmark not normalized to age and gender that is required before they are even eligible to attend Ranger school (49 push-ups in 2 minutes; 59 sit-ups in 2 minutes; and 2-mile run in 15:12 minutes), which translates to a minimum score of 70 for a male that is in the 22- to 26-year age range. However, the truth is that these soldiers are expected to score at least 300 points (80 push-ups in 2 minutes; 80 sit-ups in 2 minutes; and a 2-mile run in under 13 minutes) after completing Ranger school and becoming a member of the Ranger Regiment.
Musculoskeletal Injury Surveillance
After baseline data collection, each participant was followed for 1 year to track the incidence of musculoskeletal injuries. Each subject was emailed monthly to query as to whether they had sustained a musculoskeletal injury over the past month. At the end of the year, injury data were extracted from healthcare records and from the Military Health System Management and Reporting Tool healthcare database using an established process [18, 19]. The Comprehensive Injury Index captures International Classification of Diseases, 9th Revision (ICD-9) codes related to both traumatic and overuse injuries that are associated with the musculoskeletal system. The Overuse Injury Index captures ICD-9 codes related to overuse-type musculoskeletal injury (eg, stress fractures, stress reactions, tendonitis, bursitis, fasciitis, arthralgias, neuropathies, radiculopathies, shin splints, synovitis, and strains). A healthcare provider reviewed all injury cases to determine that the origin of the injury was overuse in nature. These injury indices have been defined and used in other work [17]. Individuals without a self-reported or medical visit for a musculoskeletal injury were categorized as noninjured.
Data Analysis
Two different statistical techniques were used to assess a set of predictors associated with injury risk. Prognostic accuracy of a multivariate model was assessed to describe how a combination of variables could describe an individual’s personal injury risk. Logistic regression equations were developed to identify the most accurate set of predictors associated with injury. The initial step for both approaches was to narrow the number of predictors of interest. Dichotomous predictors that exhibited a point estimate of the odds ratio equal to or greater than 2.0 were retained for further exploration. We calculated t-tests for continuous variables. Continuous variables with p value < 0.20 were retained for further analysis [37, 38]. The more liberal cutoff values were used to preferentially protect against Type II error at this early state of analysis. Once variables with high multicolinearity were removed, prognostic accuracy profiles were calculated for the following common set of variables for CII and OII: smoking status, prior history of surgery, history of recurrent injury, limited duty in the prior year, pain on one of the FMS clearing tests, asymmetry in dorsiflexion range of motion, run time, and sit-up performance for both CII and OII (Tables 1, 2).
After identifying variables of interest, those with high colinearity were removed. The remaining predictors were assessed to determine their prognostic accuracy for both comprehensive and overuse injuries. A more robust set of predictors was analyzed to provide a better understanding of the association with future injury risk. Receiver operator characteristic (ROC) curves identified the meaningful cutpoints in the data set. From these cutpoints, all of the data points were dichotomized and accuracy statistics were calculated.
A backward stepwise logistic regression was used to help identify the most accurate set of predictors associated with injury risk. Variables entered the equation if the probability value was < 0.05 and were removed if > 0.10. Predictors retained from stepwise procedures were then entered into the logistic regression model to maximize sample size for each model. Using the final multivariable logistic regression equation model, logits were calculated for each soldier and then transformed to predicted probabilities (predicted probability = ez/[1 + ez ]; Z = logit). Factors that exhibited an odds ratio point estimate greater than or equal to 2.0 or a t-test p value < 0.20 were identified for inclusion in the logistical multivariable regression equation. The predicted probabilities were compared with the observed occurrence of injury and noninjury using ROC curves and prognostic accuracy statistics.
Results
Single Factors that Predict Overuse Injuries in Army Rangers
The findings of the current study suggest that a common set of self-report, physical performance, and movement-based factors can predict comprehensive and overuse injuries in a US Army Ranger cohort. The specific list of factors include smoking status, history of previous surgery, history of recurrent injury, limited duty in the preceding year, pain on one of the Functional Movement Screen clearing tests, asymmetry in dorsiflexion ROM, run time, and sit-up performance. Prior surgery here referred to bone, joint, muscle, or nerve surgery, and this was reflected in the language of the questionnaire.
Using Multiple Predictors Improves the Model’s Predictive Value
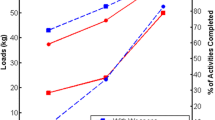
For comprehensive injuries, the specificity of the model was maximized (1.0) when six of the eight predictors were present for a given soldier (Table 3; Fig. 2). When two or more predictors were present in the model, the risk of injury increased (odds ratio [OR], 1.9; 95% confidence interval [CI], 1.0−3.5; p < 0.05). The increased risk of injury (OR, 6.7; 95% CI, 1.4–21.6) was maximized when four or more predictors were present. For overuse injuries, a maximum specificity (0.99) was achieved when five of the eight predictors were present (Table 3). Similar to the comprehensive injury model, the risk of injury increased when two or more predictors were present in the model (OR, 2.3; 95% CI, 1.1–4.8; p < 0.05). However, the risk was much greater (OR, 5.9; 95% CI, 1.1–31.5; p < 0.05) when four or more predictors were present.
From the results, our approach using multiple risk factors to identify athletes at increased risk of injury appears to be feasible in a population of elite soldiers. Our results also indicated that smoking, prior surgery, recurrent prior injury, limited-duty days in the preceding year because of injury, asymmetrical ankle dorsiflexion, pain with movement screen clearing tests, and decreased performance on the 2-mile run and 2-minute sit-up test were associated with increased injury risk (Table 4).
For comprehensive injuries, four predictors were retained in the model including current smoking status, injury recurrence, pain provocation during the Functional Movement Screen clearing tests, and ankle dorsiflexion asymmetry. These predictors accurately identified 87% of the noninjured and 39% of the injured soldiers correctly (R2 = 0.09 [Cox]; 0.12 [Nagekerke]). Accuracy statistics used Youden’s Index cutoff values; the ROC curve analysis using this model revealed an area under the curve of 0.64 (95% CI, 0.55−0.72; p < 0.05; Table 5). To best identify overuse injuries, three predictors of interest were retained in the model including recurrence of a prior injury, current smoker, and asymmetry in dorsiflexion ROM. Using just the three variables combined, 96% of the noninjured soldiers and 31% of the injured soldiers were identified correctly (R2 = 0.13 [Cox]; 0.18 [Nagekerke]). Additional screening statistics of this model included an area under the curve of 0.68 (95% CI, 0.58−0.78; p < 0.05; Table 5).
Discussion
Surveillance of injuries that led to increased medical care utilization and time loss from work has implications on national security as well as in civilian healthcare settings. Considering the staggering costs (USD 548 million per year) and impact on work loss (25 million days per year), it becomes apparent how such injuries can quickly compromise a military unit and reduce its ability to complete a mission. More importantly, the majority of these injuries are not directly related to combat and many can be prevented. However, the first step is a prospective understanding of the predictors that best identify soldiers with reduced function secondary to musculoskeletal injury. Identifying specific predictors associated with increased risk of injury is an important first step in developing effective risk mitigation strategies.
Like with any study, limitations were present. These results relate solely to an isolated population of Rangers and cannot be inferred to the US Army in general or other military populations. In fact, not all the Rangers whom we approached elected to participate; self-selection bias could have had an unquantifiable influence on our results. The primary limitation of our study was the single location at which the trial took place. Geographic- and cohort-specific factors (men only) along with training factors at the unit location may have predisposed the Ranger unit to a certain type of injury and associated risk factors. However, all Rangers undergo the same baseline training together at the same location, and while stationed in different places, they often travel to similar locations. Therefore, we do not believe location played an important role in our cohort. All the same, performing a similar task at multiple Ranger installations would not only increase the sample size of our study, but also have the potential to improve the external validity of our findings to account for possible geographic factors. Finally, the identification of injuries is primarily based on a combination of self-report and data taken from electronic medical records, which maintained the consistent limitations associated with self-report and medical recordkeeping. However, the steps taken to thoroughly identify occurrence of MSI from multiple resources (self-report, electronic medical records review, and the healthcare utilization database extraction) likely helped improve the identification of injuries.
When identifying individuals at risk for injury, often the problem does not come down to one single issue. Our study yielded a prediction model consisting of a combination of modifiable and nonmodifiable risk factors (smoking status, history of surgery, history of recurrent injury, limited duty in the prior year, pain on one of the Functional Movement Screen clearing tests, asymmetry in dorsiflexion ROM, run time, and sit-up performance). Although the results need further validation, we were able to identify subjects with three or more modifiable predictors that can be addressed with personalized education and training (Fig. 2). For those with one or fewer predictors, the hypothesis was that a non-modifiable risk factor may have contributed to the injury, and an intervention may be less relevant. The subjects with only two predictors fell into a “gray zone” of uncertainty (Fig. 2). The model provided less guidance as to what may be best for these individuals based on risk-mitigating courses of action. These findings support the initial hypothesis that a combination of predictors would yield a more robust prediction model compared with a single predictor variable alone. Furthermore, these findings corroborate other research in this field. Kazman and colleagues [16] found that a combination of Functional Movement Screen composite scores and running time provided a more robust prediction model that either item alone in Marine Corps officer candidates. The same was also found in a cohort of collegiate athletes albeit using a different set of predictors, Functional Movement Screen, lower quarter Y-balance, and injury history [23]. The findings from our study identify several modifiable predictors specific to Rangers, which can potentially be the focus for risk mitigation strategies (smoking status, pain on movement screen clearing tests, asymmetry in dorsiflexion ROM, run time, and sit-up performance). Future efforts should evaluate the impact of providing behavioral (smoking status), medical (pain on movement screen clearing tests), and fitness (asymmetry in dorsiflexion ROM, run time, and sit-up performance)-based interventions in an attempt to reduce future injury incidence.
It is not surprising that smoking was associated with the highest risk of injury. Smoking is related to poorer functional outcomes, independent of the nature or severity of injury [22]. It is an independent risk factor across a variety of populations and conditions [5, 26, 30, 42], but specifically associated with delayed healing and recurrence of pain in shoulder [6], back [29], neck [14], and multiple other exercise-related injuries [2]. It has deleterious effects on peak bone mass [8], bone mineral density [43], bone healing [28], and wound healing [4, 25] as well as many other general complications [41]. However, the exact nature of this association still needs further investigation.
The unique analytic model used in our study supported a risk stratification process and possible tiered approach to injury prevention for Rangers. The application of this information could lead to a more holistic approach to injury prevention than focusing on any single factor. For instance, the final statistical model in the current study supports collaborative care models incorporating healthcare providers who target smoking cessation as well as those who provide care to improve joint mobility and reduce joint pain. Developing a specific checklist of important factors that are relevant to maintain soldier health allows for an efficient discussion with nonhealthcare providers. This efficient discussion can provide a larger network of individuals who can effectively reinforce the importance of soldier health as well as funneling soldiers to seek out the appropriate cost-effective resources before significant injury develops. Similar models are currently incorporated in some professional and collegiate athlete settings so that sports coaches, strength coaches, and healthcare providers have an efficient understanding of the health of the team. These models tend to incorporate factors beyond the scope of the current study such as sleep, physiologic readiness, general stress, dehydration, and other factors. Understanding how these additional factors affect soldier readiness, in addition to the factors discovered in the current study, is the next step in identifying what predominant factors assist in screening for soldiers at risk for developing musculoskeletal injuries. The study and inclusion of similar models in a civilian population will likely go a long way in reducing the extensive economic and functional burden that musculoskeletal injuries have on the general public. Developing a network that links the traditional health care and wellness models in the civilian population through the examination of relevant performance tests and measures will serve as a beneficial platform to improve community health metrics.
A multifactorial approach (history of injury, smoking, pain provocation, movement tests, and performance measures) was associated with identifying Rangers at risk for injury. The summation of the number of risk factors produced a highly sensitive (one or less factor) and specific (three or more factors) model, which can potentially be used to effectively identify and intervene in those with elevated risk for musculoskeletal injury. Future research should establish whether screening and intervention can improve musculoskeletal health and if application of our findings translates to other military and civilian populations or sporting activities. A better understanding of characteristics associated with future injury risk can provide a foundation for both military and civilian prevention programs. Validated models could help reduce medical cost and lost duty days as well as improve the overall health and readiness of elite military units.
References
Alentorn-Geli E, Mendiguchia J, Samuelsson K, Musahl V, Karlsson J, Cugat R, Myer GD. Prevention of non-contact anterior cruciate ligament injuries in sports. Part II: systematic review of the effectiveness of prevention programmes in male athletes. Knee Surg Sports Traumatol Arthrosc. 2014;22:16–25.
Altarac M, Gardner JW, Popovich RM, Potter R, Knapik JJ, Jones BH. Cigarette smoking and exercise-related injuries among young men and women. Am J Prev Med. 2000;18:96–102.
Armed Forces Health Surveillance Center. Medical Evacuations from Afghanistan during Operation Enduring Freedom, Active and Reserve Components, US Armed Forces, 7 October 2001–31 December 2012. Medical Surveillance Monthly Report (MSMR). 2013;20:2–8.
Bartsch RH, Weiss G, Kastenbauer T, Patocka K, Deutinger M, Krapohl BD, Benditte-Klepetko HC. Crucial aspects of smoking in wound healing after breast reduction surgery. J Plast Reconstr Aesthetic Surg. 2007;60:1045–1049.
Behrend C, Prasarn M, Coyne E, Horodyski M, Wright J, Rechtine GR. Smoking cessation related to improved patient-reported pain scores following spinal care. J Bone Joint Surg Am. 2012;94:2161–2166.
Bishop JY, Santiago-Torres JE, Rimmke N, Flanigan DC. Smoking predisposes to rotator cuff pathology and shoulder dysfunction: a systematic review. Arthroscopy. 2015.
Butler R, Plisky P, Kiesel K. Interrater reliability of videotaped performance on the functional movement screen using the 100-point scoring scale. Athletic Training and Sports Health Care. 2012;4:103–109.
Callreus M, McGuigan F, Akesson K. Adverse effects of smoking on peak bone mass may be attenuated by higher body mass index in young female smokers. Calcif Tissue Int. 2013;93:517–525.
Gorman PP, Butler RJ, Plisky PJ, Kiesel KB. Upper quarter Y balance test: reliability and performance comparison between genders in active adults. J Strength Cond Res. 2012;26:3043–3048.
Gribble PA, Hertel J, Plisky P. Using the Star Excursion Balance Test to assess dynamic postural-control deficits and outcomes in lower extremity injury: a literature and systematic review. J Athl Train. 2012;47:339–357.
Harman DR, Hooper TI, Gackstetter GD. Aeromedical evacuations from Operation Iraqi Freedom: a descriptive study. Mil Med. 2005;170:521–527.
Hauret KG, Jones BH, Bullock SH, Canham-Chervak M, Canada S. Musculoskeletal injuries description of an under-recognized injury problem among military personnel. Am J Prev Med. 2010;38:S61–70.
Headquarters Department of the Army. Field Manual 21–20 Physical Fitness Training. Washington, DC, USA: Headquarters Department of the Army; 1998.
Hogg-Johnson S, van der Velde G, Carroll LJ, Holm LW, Cassidy JD, Guzman J, Cote P, Haldeman S, Ammendolia C, Carragee E, Hurwitz E, Nordin M, Peloso P; Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated Disorders. The burden and determinants of neck pain in the general population: results of the Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated Disorders. Spine (Phila Pa 1976). 2008;33:S39–51.
Jones BH, Perrotta DM, Canham-Chervak ML, Nee MA, Brundage JF. Injuries in the military: a review and commentary focused on prevention. Am J Prev Med. 2000;18:71–84.
Kazman JB, Galecki JM, Lisman P, Deuster PA, O’Connor FG. Factor structure of the functional movement screen in marine officer candidates. J Strength Cond Res. 2014;28:672–678.
Knapik J, Darakjy S, Scott SJ, Hauret KG, Canada S, Marin R, Rieger W, Jones BH. Evaluation of a standardized physical training program for basic combat training. J Strength Cond Res. 2005;19:246–253.
Knapik JJ, McCollam R, Canham-Chervak M, Hoedebecke E, Arnold S, Craig S, Barko W. Injuries and injury prevention among senior military officers at the Army War College. Mil Med. 2002;167:593–599.
Knapik JJ, Sharp MA, Canham-Chervak M, Hauret K, Patton JF, Jones BH. Risk factors for training-related injuries among men and women in basic combat training. Med Sci Sports Exerc. 2001;33:946–954.
Konor MM, Morton S, Eckerson JM, Grindstaff TL. Reliability of three measures of ankle dorsiflexion range of motion. Int J Sports Phys Ther. 2012;7:279–287.
Krause DA, Cloud BA, Forster LA, Schrank JA, Hollman JH. Measurement of ankle dorsiflexion: a comparison of active and passive techniques in multiple positions. J Sport Rehabil. 2011;20:333–344.
Langley J, Davie G, Wilson S, Lilley R, Ameratunga S, Wyeth E, Derrett S. Difficulties in functioning 1 year after injury: the role of preinjury sociodemographic and health characteristics, health care and injury-related factors. Arch Phys Med Rehabil. 2013;94:1277–1286.
Lehr ME, Plisky PJ, Butler RJ, Fink ML, Kiesel KB, Underwood FB. Field-expedient screening and injury risk algorithm categories as predictors of noncontact lower extremity injury. Scand J Med Sci Sports. 2013;23:e225–e232.
Lincoln AE, Smith GS, Amoroso PJ, Bell NS. The natural history and risk factors of musculoskeletal conditions resulting in disability among US Army personnel. Work. 2002;18:99–113.
Manassa EH, Hertl CH, Olbrisch RR. Wound healing problems in smokers and nonsmokers after 132 abdominoplasties. Plastic Reconstr Surg. 2003;111:2082–2087; discussion 2088–2089.
Mikkonen P, Leino-Arjas P, Remes J, Zitting P, Taimela S, Karppinen J. Is smoking a risk factor for low back pain in adolescents? A prospective cohort study. Spine (Phila Pa 1976). 2008;33:527–532.
Nindl BC, Williams TJ, Deuster PA, Butler NL, Jones BH. Strategies for optimizing military physical readiness and preventing musculoskeletal injuries in the 21st century. US Army Medical Department Journal. 2013:5–23.
Patel RA, Wilson RF, Patel PA, Palmer RM. The effect of smoking on bone healing: a systematic review. Bone Joint Res. 2013;2:102–111.
Petre B, Torbey S, Griffith JW, De Oliveira G, Herrmann K, Mansour A, Baria AT, Baliki MN, Schnitzer TJ, Apkarian AV. Smoking increases risk of pain chronification through shared corticostriatal circuitry. Hum Brain Mapp. 2015;36:683–694.
Prasarn ML, Horodyski MB, Behrend C, Wright J, Rechtine GR. Negative effects of smoking, workers’ compensation, and litigation on pain/disability scores for spine patients. Surg Neurol Int. 2012;3:S366–369.
Ruscio BA, Jones BH, Bullock SH, Burnham BR, Canham-Chervak M, Rennix CP, Wells TS, Smith JW. A process to identify military injury prevention priorities based on injury type and limited duty days. Am J Prev Med. 2010;38:S19–33.
Schiftan GS, Ross LA, Hahne AJ. The effectiveness of proprioceptive training in preventing ankle sprains in sporting populations: a systematic review and meta-analysis. J Sci Med Sport. 2015;18:238–244.
Shaffer SW, Teyhen DS, Lorenson CL, Warren RL, Koreerat CM, Straseske CA, Childs JD. Y-balance test: a reliability study involving multiple raters. Mil Med. 2013;178:1264–1270.
Songer TJ, LaPorte RE. Disabilities due to injury in the military. Am J Prev Med. 2000;18:33–40.
Sugimoto D, Myer GD, Bush HM, Klugman MF, Medina McKeon JM, Hewett TE. Compliance with neuromuscular training and anterior cruciate ligament injury risk reduction in female athletes: a meta-analysis. J Athl Train. 2012;47:714–723.
Teyhen D, Shaffer S, Lorenson C, Wood S, Rogers S, Dugan J, Walker M, Childs J. Reliability of lower quarter physical performance measures in healthy service members. US Army Medical Department Journal. 2011;July-September:37–49.
Teyhen DS, Flynn TW, Childs JD, Abraham LD. Arthrokinematics in a subgroup of patients likely to benefit from a lumbar stabilization exercise program. Phys Ther. 2007;87:313–325.
Teyhen DS, Flynn TW, Childs JD, Kuklo TR, Rosner MK, Polly DW, Abraham LD. Fluoroscopic video to identify aberrant lumbar motion. Spine (Phila Pa 1976). 2007;32:E220–229.
Teyhen DS, Shaffer SW, Lorenson CL, Greenberg MD, Rogers SM, Koreerat CM, Villena SL, Zosel KL, Walker MJ, Childs JC. Clinical measures associated with dynamic balance and functional movement. J Strength Cond Res. 2014;28:1272–1283.
Teyhen DS, Shaffer SW, Lorenson CL, Halfpap JP, Donofry MJ, Dugan JL, Childs JD. The functional movement screen: a reliability study. J Orthop Sports Phys Ther. 2012;42:530–540.
Truntzer J, Vopat B, Feldstein M, Matityahu A. Smoking cessation and bone healing: optimal cessation timing. Eur J Orthop Surg Traumatol. 2015;25:211–215.
Van Middelkoop M, Kolkman J, Van Ochten J, Bierma-Zeinstra SM, Koes BW. Risk factors for lower extremity injuries among male marathon runners. Scand J Med Sci Sports. 2008;18:691–697.
Ward KD, Klesges RC. A meta-analysis of the effects of cigarette smoking on bone mineral density. Calcif Tissue Int. 2001;68:259–270.
Westrick RB, Miller JM, Carow SD, Gerber JP. Exploration of the y-balance test for assessment of upper quarter closed kinetic chain performance. Int J Sports Phys Ther. 2012;7:139–147.
Acknowledgments
This study was conducted in collaboration with physical therapy research and administrative assistants from US Army-Baylor University, US Army Medical Department Center and School, San Antonio, TX, USA; the University of Evansville, Evansville, IN, USA; Duke University, Durham, NC; and University of Puget Sound, Tacoma, WA, USA. We thank Ann-Maree Williams PT, DPT, COMT, and Jennifer C. Prye MEd, ATC, for their assistance with data collection, analysis, and manuscript preparation. We acknowledge the following staff for their administrative and technical support: Mr Josh Miller, Ms Julie Koepp, Ms Nadine Shewell, Mr Norman Gardner, Ms Liz Reilly-Hess, Ms Celestina Wildman, Miyoko D. Sasakura MSPH, Gail Baudendistel PT, CPA, MS, MAFM, Tom Kurtz PT, and Mr Jeff Wilson. Technology support included Bob Humphrey, Dalene Becka, Jack Brower, and Jaret Willard. Additional data logistical support provided by Ms Theresa Leatherwood, MAJ Carrie Hoppes, SFC Sean Stephens, SFC Ryan Murphy, SSG Christopher Villarreal, CPO Ferdinand Ajel, Paul Gorman ATC, PTA, CSCS, Luck Chanthabandith, Phil Borja, Matthew Buchanan, and Valeria DeAngelis.
Author information
Authors and Affiliations
Corresponding author
Additional information
Research support was provided by Joint Base Lewis McChord’s Physical Therapy Clinic, Madigan Army Medical Center, Tacoma, WA, USA; and the 2/75th Ranger Regiment, Joint Base Lewis McChord, WA, USA. This project was financially supported by the Army Medical Department Advanced Medical Technology Initiative (AAMTI, Principal Investigator [PI]: DST), Telemedicine and Advanced Technology Research Center (TATRC, PI: DST), and the Defense Medical Research and Development Program, Military Operation Medicine Research Program (PI: DST) from the US Army Medical Research and Materiel Command, Fort Detrick, MD, USA. One or more of the authors (KBK, PJP) own equity in Move2Perform LLC and have developed the Move2Perform software that was used to collect data as part of this study. One of the authors (PJP) developed the Y Balance Test™, which was also used in this study.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
The views expressed are those of the authors and do not reflect the official policy of Madigan Army Medical Center, Brooke Army Medical Center, the Department of the Army, the Department of Defense, or the US Government.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This study was performed at Madigan Army Medical Center, Fort Lewis, WA, USA.
About this article
Cite this article
Teyhen, D.S., Shaffer, S.W., Butler, R.J. et al. What Risk Factors Are Associated With Musculoskeletal Injury in US Army Rangers? A Prospective Prognostic Study. Clin Orthop Relat Res 473, 2948–2958 (2015). https://doi.org/10.1007/s11999-015-4342-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-015-4342-6