Abstract
Introduction
Geographical variation in rates of emergency inpatient admission for chronic disease may be due to variation in health need. However, it may also reflect differences in the provision of services which reduce the risk of inpatient admission for chronic disease, such as primary care.
Aims
The aim of this paper was to examine the effect of primary care provision [general practitioner (GP) supply] and deprivation on county-specific rates of emergency admission to hospital for diabetes complications and chronic obstructive pulmonary disease (COPD) in Ireland.
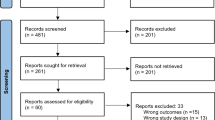
Methods
Data on emergency inpatient discharges were obtained from the hospital inpatient enquiry (HIPE) system. Secondary data on GP supply were obtained from a recently published study, while secondary data on deprivation were obtained from the Small Area Health Research Unit. The effect of county-level GP supply and deprivation on age-standardised rates of discharge for diabetes complications and COPD were examined, adjusting for population density and the proportion of the population who were eligible for free primary care.
Results
Greater deprivation and lower GP supply are associated with increased rates of discharge from hospital for COPD and diabetes complications. However, these associations are stronger in counties where a lower proportion of the population are eligible for free primary care.
Conclusion
Geographical variation in rates of admission to hospital for chronic disease is associated with both population need and health system factors. These findings suggest that primary care resourcing must be a key consideration in any efforts to tackle acute hospital capacity problems.






Similar content being viewed by others
References
Page A, Ambrose S, Glover J, Hetzel D (2007) Atlas of avoidable hospitalisations in Australia: ambulatory care-sensitive conditions. PHIDU, Adelaide
Department of Health (UK) (2013) The NHS outcomes framework 2014/15. https://www.gov.uk/government/publications/nhs-outcomes-framework-2014-to-2015. Accessed 18 Sept 2015
Department of Health (Ireland) (2015) National healthcare quality reporting system. http://health.gov.ie/blog/publications/national-healthcare-quality-reporting-system/. Accessed 18 Sept 2015
Van Loenen T, van den Berg MJ, Westert GP, Faber MJ (2014) Organizational aspects of primary care related to avoidable hospitalization: a systematic review. Fam Pract 31:502–516. doi:10.1093/fampra/cmu053
Gibson OR, Segal L, McDermott RA (2013) A systematic review of evidence on the association between hospitalisation for chronic disease related ambulatory care sensitive conditions and primary health care resourcing. BMC Health Serv Res 13:336. doi:10.1186/1472-6963-13-336
Blunt I (2013) Focus on preventable admissions: trends in emergency admissions for ambulatory care sensitive conditions, 2001 to 2013. http://www.health.org.uk/publication/qualitywatch-focus-preventable-admissions. Accessed 18 Sept 2015
Sheridan A, Howell F, Bedford D (2012) Hospitalisations and costs relating to ambulatory care sensitive conditions in Ireland. Ir J Med Sci 181:527–533. doi:10.1007/s11845-012-0810-0
Economic and Social Research Institute (2013) Activity in acute public hospitals in Ireland annual report 2012. Dublin
Teljeur C, Tyrrell E, Kelly A et al (2014) Getting a handle on the general practice workforce in Ireland. Ir J Med Sci 183:207–213. doi:10.1007/s11845-013-0991-1
Kelly A, Teljeur C (2013) The National deprivation index for health and health services research, Update 2013. Dublin
Cohen J (1992) A Power Primer. Psychol Bull 112:155–159
Teljeur C, O’Dowd T, Thomas S, Kelly A (2010) The distribution of GPs in Ireland in relation to deprivation. Heal Place 16:1077–1083. doi:10.1016/j.healthplace.2010.06.011
Eggli Y, Desquins B, Seker E, Halfon P (2014) Comparing potentially avoidable hospitalization rates related to ambulatory care sensitive conditions in Switzerland: the need to refine the definition of health conditions and to adjust for population health status. BMC Health Serv Res 14:25. doi:10.1186/1472-6963-14-25
Acknowledgments
This research would not have been possible without the data collected through the HIPE system, which is managed by the Healthcare Pricing Office (HPO). Access to the system was facilitated by Health Atlas Ireland. The research was also supported by the Royal College of Surgeons in Ireland (RCSI) and the RCSI Hospitals Group. The manuscript was finalised while one of the authors was employed by The Irish Longitudinal Study on Ageing (TILDA) at Trinity College Dublin.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Sexton, E., Bedford, D. GP supply, deprivation and emergency admission to hospital for COPD and diabetes complications in counties across Ireland: an exploratory analysis. Ir J Med Sci 185, 453–461 (2016). https://doi.org/10.1007/s11845-015-1359-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-015-1359-5