Abstract
Purpose
To compare two commonly used methods of temporary hemiepiphysiodesis (staples and figure of eight plate) in the management of coronal plane deformities of the knee in skeletally immature children.
Methods
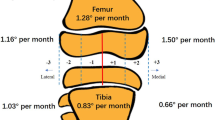
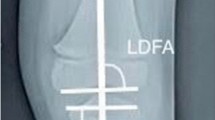
This prospective study was conducted between November 2012 and November 2015. A total of 40 patients with 67 affected knee joints, having at least 1 year of skeletal growth remaining, were included in the study. Angular correction was measured by recording the mechanical lateral distal femoral angle (mLDFA), mechanical medial proximal tibial angle (mMPTA), and anatomical tibio-femoral angle (TFA) (for the overall alignment of lower limbs). Implant removal was done after 5° of overcorrection was achieved. The rate of correction (° per month) and complications related to each technique were recorded.
Results
The most common diagnosis was idiopathic genu valgum. The overall rate of correction (TFA) was 1.2° for staples and 1.4° for eight plate (p = 0.70, not statistically significant). The correction in mLDFA was statistically better in the eight plate group, whereas an opposite trend was recorded in mMPTA. Implant-related complications were present in two cases of the staples group.
Conclusion
Although the overall correction rate was similar in both groups, implant-related complications were lower with figure of eight plate. In idiopathic genu valgum (the most common diagnosis), the correction was statistically better in the eight plate group. We recommend figure of eight plate over staples in managing these deformities.
Similar content being viewed by others
Introduction
Angular deformities around the knee joint are common in the pediatric population. Physiological deformities account for the majority of these cases [1]. While physiological deformities usually correct with growth, pathological deformities can cause functional impairment in the form of abnormal gait, painful joint, and a potential risk of developing osteoarthritis of the knee. Temporary hemiepiphysiodesis, timed permanent hemiepiphysiodesis, corrective osteotomy, and Ilizarov ring fixator application are the various surgical modalities for the correction of angular deformities around the knee joint [2–7]. Corrective osteotomies provide desired correction immediately but are associated with complications like increased blood loss, risk of compartment syndrome, neurovascular injury, and growth disturbance if the growth plate is damaged [2–4]. Prolonged period of immobilization following corrective osteotomy may also cause joint stiffness. Permanent hemiepiphysiodesis has unpredictable results, as the timing of the procedure is never precise. Overcorrection and undercorrection are common complications [7]. Limb length discrepancy can also occur, which may later require correction [7]. Staples, percutaneous screws, or figure of eight plate (tension band plate) can be used for temporary hemiepiphysiodesis [8–10]. It is a less invasive technique compared to osteotomy. The results are more predictable and the process is reversible. The implants can be removed after the desired correction is achieved. Figure of eight plates and epiphyseal staples are both widely used methods of temporary hemiepiphysiodesis [8, 9]. Complications related to the use of staples include breakage, extrusion, and permanent physeal damage [9, 11, 12]. Eight plates have been shown to have fewer complications [9, 13]. Although costlier, figure of eight plates are considered a better alternative to staples because of the fewer complications in comparative studies [14–16]. In this study, we have shared our experience with use of figure of eight plates (Orthofix) and staples (locally manufactured stainless steel staples) for the correction of coronal plane deformities around the knee joint.
Materials and methods
This prospective study was conducted between November 2012 and November 2015. The included patients had coronal plane angular knee deformities (genu varum and valgum) with at least 1 year of skeletal growth remaining. The following cases were excluded: physiological deformities, deformities due to metabolic disorders that improved with medical management, deformities as a result of infection or neoplasm, post-traumatic deformities, dynamic deformities as in neuromuscular disorders and contractures, non-ambulatory patients.
The placement of implant in the distal femur, proximal tibia, or both was based on the location of the primary deformity as assessed by abnormality in the mechanical lateral distal femoral angle (mLDFA) and mechanical medial proximal tibial angle (mMPTA). One staple was placed on each side of the midsagittal plane in a submuscular position, with care taken to preserve the periosteum. Intraoperative imaging was used to verify satisfactory hardware placement in both the anteroposterior and lateral planes. Similarly, one eight plate was placed in the midsagittal plane (or slightly posterior to it to avoid future recurvatum deformity), with one screw proximal and one distal to the physis. The entire procedure was extraperiosteal, and care was taken to avoid damage to the physis. Figure 1 depicts intraoperative clinical and radiographic photos. Knee range of motion and full weight-bearing were allowed from the first post-operative day. Crutches or a walker were used to assist in walking in the initial few days. Unassisted weight-bearing was begun as pain subsided. Early return to daily activities was encouraged. The implants were removed after 5° of overcorrection was achieved.
Standing orthoroentgenograms were used to measure the angles. This view allowed assessment of the overall mechanical alignment, mLDFA, mMPTA, and anatomical tibio-femoral angle (TFA). Documentation of these radiological parameters was done at 4-monthly intervals in order to avoid crowding of insignificant observations.
All patients were observed for complications, including wound-related complications, failure to document any improvement after 4 months, implant breakage, implant extrusion, overcorrection (more than 5° in the opposite direction), and physeal penetration. Persistence of deformity 2 years post-surgery was considered as a failure and indication for an alternative procedure in the form of corrective osteotomy.
The end point of correction (time of implant removal) was planned taking into account the “rebound phenomenon”. TFA, mLDFA, and mMPTA were measured, as they are more accurate than clinical examination findings. Aiming for 5° of overcorrection in order to compensate for rebound growth, we kept our end point at 92 ± 3° for mLDFA and 82 ± 3° for mMPTA for valgus deformity correction and 82 ± 3° of mLDFA and 92 ± 3° of mMPTA for varus deformity correction. All patients approaching correction were closely followed every 2 weeks to prevent more than the desired overcorrection. After implant removal, all patients included in the study were closely followed every 2 months to document any recurrence.
SPSS version 20.0 was used for calculation of the mean and standard deviation within the two groups. An independent samples t test was used for the comparison of means. A p-value of less than 0.05 was considered to be statistically significant.
The institutional review board and ethics committee approved the study. Ethical standards according to the Helsinki declaration of 1964 (and its later amendments) were conformed to. Informed consent was obtained from all patients.
Results
Forty patients with 67 affected knee joints were included in the study. Three patients were lost to follow-up. Thirty-seven patients (63 knee joints) with a minimum follow-up of 2 years were available for final assessment. Thirty-one knee joints were included the figure of eight plate group (19 patients), while 32 were included in the epiphyseal staples group (18 patients). Figure 2 shows radiological correction in a case managed with staples and Fig. 3 shows a case managed with eight plate.
A total of 75 hemiepiphysiodeses were performed on 37 patients (63 in the distal femur, 12 in the proximal tibia). The age and sex distribution, laterality, and number of varus and valgus deformities were similar in both groups (Table 1). The mean age was 7.3 years (range: 3.5–12 years) in the staple group and 7.8 years (range: 4–12.0 years) in eight plate group. The male:female ratio was 8:10 in the staple group and 8:11 in the eight plate group. Idiopathic genu valgum followed by post-rachitic deformity were the most common underlying etiologies. One patient in the eight plate group had bilateral genu valgum deformity after successful treatment of congenital knee dislocation. The mean rate of correction was 1.2° per month in the staples group and 1.4° per month in the eight plate group (Table 2). This difference was not statistically significant (p = 0.75). One female patient with bilateral genu valgum managed with staples developed an early complication (implant extrusion) at 4 months and was not considered for calculation of the correction rate. There were no wound-related complications in either group. None of the patients had more than the desired overcorrection at the time of implant removal. A total of four knee joints (two in each group) did not achieve correction by 2 years (Table 3; Fig. 4). The underlying etiology in all these patients was skeletal dysplasia. Thus, an additional procedure was needed in four knee joints (12.5 %) in the staple group (two with failure of correction, two with implant extrusion). Two knee joints (6.5 %) in the eight plate group required additional procedure because of failure of correction. Continuing staples for more than 2 years carries the risk of permanent physeal failure [9]. This complication has not been reported with figure of eight plate. Thus, we consider it wise to remove the implants if deformity persists for more than 2 years. All patients were screened for limb length discrepancy pre-operatively. Pre-operatively, no patient had discrepancy of more than 1 cm. Three patients in the staple group (two unilateral idiopathic genu valgum, one unilateral post rachitic genu valgum) developed shortening of the affected limb of more than 1 cm, while in the eight plate group, two patients with unilateral idiopathic genu valgum developed limb length discrepancy of more than 1 cm. However, this was statistically insignificant. These patients were given appropriate shoe raise and were advised to wait till skeletal maturity for appropriate intervention. A few patients/parents were concerned about implant prominence, and reassurance was all that was required. Staple extrusion occurred in two knees (Fig. 5), while the eight plate group did not show any implant-related complications.
Discussion
Blount (1948) introduced staples as a means to achieve temporary hemiepiphysiodesis [4]. Although widely used and considered safe, several reports have documented the occurrence of complications with the use of staples [9, 11, 12]. Eight plate was introduced by Stevens as a means to avoid these complications [9]. Hemiepiphysiodesis is based on the Hueter–Volkmann principle, which states that compression and tension forces at the physis can cause physeal growth inhibition and acceleration, respectively [17]. Contrary to staples, which make a rigid construct providing compression to the physis throughout its length, eight plates act as a dynamic construct with scope for mobility at the screw–plate interface. This is the reason for staples having a higher risk of breakage and extrusion. In eight plate, maximum compression acts on the peripheral part of the physis at the screw plate junction, where it is actually required. Temporary hemiepiphysiodesis is applicable to skeletally immature children with open physes and having at least 1 year of growth remaining. Past studies had included a wide range of age groups, from as young as 2 years to those approaching skeletal maturity. In our study also, we had maintained this wide range (3.5–12 years in the staples group and 4–12 years in the eight plate group). To the best of our knowledge, only three previous studies have compared the results of staples with eight plate [14–16]. These are summarized in Table 4. In a retrospective study by Jelinek et al., during the period 1999–2008, a total of 33 knee angular deformities were treated with figure of eight plate and 32 with staples [14]. The rate of correction was similar in both treatment groups. They reported overcorrection in four cases of eight plate, which we avoided by close follow-up after correction was achieved. This is an avoidable complication. Migration of staples occurred in two cases, which is similar to our series.
In a retrospective study by Wiemann et al. [15], among 38 patients (24 extremities treated with eight plate and 39 with Blount staple temporary hemiepiphysiodesis), the rate of correction was higher in the eight plate group, but the difference was not statistically significant. Notably, they reported one case of eight plate screw breakage. The deformity correction rates in our study were comparable to past studies. The tibio-femoral angle (TFA) is a simple and reproducible measurable parameter on standing orthoroentgenogram. The overall correction rate of TFA in our study was 1.2° per month for the staple group and 1.4° per month for the eight plate group, the difference being statistically insignificant. The improvement in mMPTA was significantly lower in the eight plate group. This could be due to the small number of cases with deformity involving the proximal tibia. In skeletal dysplasia patients with abnormal physes, the correction rate was low in both groups. In idiopathic genu valgum, the correction rate was significantly lower in the staple group.
There were two knee joints with abnormal physis (skeletal dysplasia) in each group. Complications were similar to previous studies. The complication rate was slightly higher in the staple group, but this was statistically insignificant. There was no implant breakage in our series. Implant extrusion was seen in two joints in the staple group. Two failures (persistence of deformity at 2 years) were seen in both groups. Limb length discrepancy of more than 1 cm was seen in three cases in the staple group and two cases in the eight plate group. This has not been described in previous studies [14–16]. There was no case of sagittal plane deformity (flexion deformity or recurvatum deformity) in either group.
Early physiotherapy was recommended to ensure rapid return to daily activities and limit absence from school [18, 19].
Our study was not without limitations. There was an unequal distribution of varus and valgus knees, with valgus knees outnumbering varus knees in both groups. In our study, the minimum follow-up period was 2 years. Long-term follow-up studies for outcomes of eight plate are still needed. The patients with abnormal mMPTA were fewer than those with abnormal mLDFA. A larger number of the former could have helped in the better analysis of correction of mMPTA.
Conclusion
Both staples and eight plates have similar potential for the correction of angular deformity around the knee in skeletally immature children. However, eight plates have a significantly higher rate of correction in idiopathic deformities. Allowing some overcorrection before implant removal (5° in our study) can prevent rebound deformity. Unlike eight plates, staples carry a risk of migration and extrusion. Abnormal physes as in skeletal dysplasias can lead to inferior outcomes in both groups.
References
Saini UC, Bali K, Sheth B, Gahlot N, Gahlot A (2010) Normal development of the knee angle in healthy Indian children: a clinical study of 215 children. J Child Orthop 4(6):579–586
Rang M (1966) Anthology of orthopaedics. E & S Livingstone Ltd., Edinburgh
Gariepy R (1964) Genu varum treated by high tibial osteotomy. J Bone Joint Surg Br 46:783–784
Blount WP, Clarke GR (1949) Control of bone growth by epiphyseal stapling; a preliminary report. J Bone Joint Surg Am 31A(3):464–478
Macewen W (1880) Osteotomy with an inquiry into the aetiology and pathology of knock-knee, bow-leg, and other osseous deformities of the lower limbs. Churchill, London
Smith JO, Wilson AJ, Thomas NP (2013) Osteotomy around the knee: evolution, principles and results. Knee Surg Sports Traumatol Arthrosc 21(1):3–22
Stevens PM (2006) Guided growth: 1933 to the present. Strateg Trauma Limb Reconstr 1(1):29–35
Raab P, Wild A, Seller K, Krauspe R (2001) Correction of length discrepancies and angular deformities of the leg by Blount’s epiphyseal stapling. Eur J Pediatr 160(11):668–674
Stevens PM (2007) Guided growth for angular correction: a preliminary series using a tension band plate. J Pediatr Orthop 27:253–259
Métaizeau J-P, Wong-Chung J, Bertrand H, Pasquier P (1998) Percutaneous epiphysiodesis using transphyseal screws (PETS). J Pediatr Orthop 18(3):363–369
Fraser RK, Dickens DRV, Cole WG (1995) Medial physeal stapling for primary and secondary genu valgum in late childhood and adolescence. J Bone Joint Surg Br 77(5):733–735
Mielke CH, Stevens PM (1996) Hemiepiphyseal stapling for knee deformities in children younger than 10 years: a preliminary report. J Pediatr Orthop 16(4):423–429
Stevens PM, Klatt JB (2008) Guided growth for pathological physes: radiographic improvement during realignment. J Pediatr Orthop 28(6):632–639
Jelinek EM, Bittersohl B, Martiny F, Scharfstädt A, Krauspe R, Westhoff B (2012) The 8-plate versus physeal stapling for temporary hemiepiphyseodesis correcting genu valgum and genu varum: a retrospective analysis of thirty five patients. Int Orthop 36(3):599–605
Wiemann JM 4th, Tryon C, Szalay EA (2009) Physeal stapling versus 8-plate hemiepiphysiodesis for guided correction of angular deformity about the knee. J Pediatr Orthop 29(5):481–485
Gottliebsen M, Rahbek O, Hvid I, Davidsen M, Hellfritzsch MB, Møller-Madsen B (2013) Hemiepiphysiodesis: similar treatment time for tension-band plating and for stapling: a randomized clinical trial on guided growth for idiopathic genu valgum. Acta Orthop 84(2):202–206
Stokes IAF (2002) Mechanical effects on skeletal growth. J Musculoskelet Neuronal Interact 2(3):277–280
Fillingham YA, Kroin E, Frank RM, Erickson B, Hellman M, Kogan M (2014) Post-operative delay in return of function following guided growth tension plating and use of corrective physical therapy. J Child Orthop 8(3):265–271
Fillingham YA, Luthringer T, Erickson BJ, Kogan M (2015) Does physical therapy prevent post-operative delay in return of function following tension-band plating? J Child Orthop 9(6):483–487
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
None.
Conflict of interest
None. No author has any financial conflict of interest with the implant, implant manufacturer, or implant distributor.
Ethical approval
All procedures performed in this study were in accordance with the ethical standards of the institution and with the 1964 Helsinki declaration and its later amendments.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Kumar, A., Gaba, S., Sud, A. et al. Comparative study between staples and eight plate in the management of coronal plane deformities of the knee in skeletally immature children. J Child Orthop 10, 429–437 (2016). https://doi.org/10.1007/s11832-016-0758-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11832-016-0758-0