Abstract
This study aims to provide a new method for treatment of severely comminuted fractures without bone loss using the well-known technique of bone transport. Sixteen patients suffering from severely comminuted fractures with closed soft tissue injury were prospectively treated using bone transport by Ilizarov circular fixator. There were 14 male and 2 female patients. The mean age was 36.5 years (27–45). There were 13 proximal tibial metaphyseal fractures, one tibial diaphyseal fracture and two femoral distal metaphyseal fractures. All patients had closed soft tissue. The mean length of the comminution gap was 50.3 mm (40–64). Fracture healing occurred in 15 patients. The mean healing time was 23.4 weeks (14–30). No bone stimulating procedures were needed for either the fracture or distraction site. Using the IOWA knee and ankle score for assessment of the 15 patients who completed treatment: the functional outcome for the knee was excellent in 11 patients, good in three and fair in one. The ankle score was excellent in 12 patients, good in two and fair in one. According to Paley and Maar’s, bone results were excellent in 14 patients, good in one patient and poor in the patient who had failure of the procedure. The results achieved in this work are encouraging to keep on applying this technique to treat fractures that meet the following criteria: metaphyseal, with total circumferential comminution involving more than 4 cm of the bone length.
Similar content being viewed by others
Introduction
Bone transport for the management of traumatic bone loss is a well-known technique [1–4]. Bone loss may occur from extrusion of fragments at the time of injury or during debridement of an open fracture when devitalized segments of bone are removed. This creates a segmental defect or gap between the remaining bone ends.
A severely comminuted fracture with intact soft tissue envelope, having circumferentially widely separated fragments that involve more than 2 cm of the bone length, should be considered as a fracture with “contained defect” or “internal bone loss.” Open fractures with segmental defects more than 2 cm are unlikely to heal spontaneously following bone stabilization alone. Fractures with 50 % or more of circumferential bone loss require bone graft to restore normal volume and strength [5–8].
Comminuted fractures with contained bone defects present difficulties in management because of the high potential of reduced fragments’ viability, soft tissue compromise and problems with stabilization. Various surgical methods have been proposed for treating such complex fractures including: internal fixation by plates and screws, intramedullary nailing and external fixation [5, 9, 10].
Circular external fixator provides multilevel stabilization of the fractured limb segments with minimal disruption of the soft tissue envelope. It is particularly useful where bone gaps need reconstruction by distraction osteogenesis.
This is a report of using bone transport technique to manage closed comminuted fractures with “contained bone defects” to bridge the gap and achieve healing in a reasonable time.
Patients and methods
Between June 2005 and January 2011, 16 patients suffering from severely comminuted fractures with closed soft tissue injury were treated using bone transport by Ilizarov circular fixator.
There were 14 males and 2 females. The mean age was 36.5 years (range 27–45). There were 14 tibial fractures (13 proximal metaphyseal and one diaphyseal), and two femoral distal metaphyseal fractures. According to AO/OTA system [11], ten fractures were classified as 41.A3, three as 41.C2, one as 42.C3, one as 33.A3.3 and one fracture as 33.C2.3.
All patients had closed soft tissue injuries that were graded according to Tscherene and Gotsen method [12]. Eight were grade I, five were grade II and three were grade III. Nine patients had their fractures as isolated injury while seven had other fractures (Table 1). The mechanism of injury was road traffic accident in 11 patients, trauma from a heavy object in three patients and falls from a height in two patients.
The length of the segmental comminution gap was measured between two points of circumferentially intact bone at the proximal and distal main bone segments (Fig. 1). The mean length of this gap was 50.3 mm (range 40–64).
Four patients had their fracture initially immobilized with a mono-lateral spanning external fixator. Twelve patients had their fractures immobilized in plaster back slab until definitive stabilization. The mean time to definitive surgery was 8.8 days (range 1–28). The operative delay in some patients was due to late referral from primary centers.
Four patients (three type 41-C2 proximal tibia and one type 33-C2.3 distal femur) had their articular fragments reduced and fixed percutaneously with one or two cannulated 6.5 screws and washers. Tibial fractures were stabilized with an Ilizarov frame; each segment of bone was fixed either by two rings or a single ring with a drop wire or half pin on either side. Each ring was fixed by at least two tensioned 1.8-mm wires and a 6-mm predrilled half pin. The femoral frames comprised two femoral arches proximally and two distal rings. Three or four 6-mm half pins fixed each arch. Two tensioned wires and half pins were fixed to the rings.
The two femoral fractures and the tibial diaphyseal fracture had proximal to distal bone transport. The 13 proximal tibial fractures had distal to proximal bone transport. Corticotomies were done using predrilling technique.
Postoperatively, patients were allowed partial weight bearing unless contraindicated by the presence of other injuries. Knee and ankle range of motion exercises started on the first postoperative day or as tolerated by the patient. Distraction started after a latent period of 7 days at a rate of 0.25 mm/6 h. This continued till the comminuted fragments resisted transport. Thus, the amount of distraction was not necessarily equal to the preoperative measured length of contained defect (Fig. 2).
Pin site care included daily removal of crusts with normal saline and application of compressive dressing. Alcoholic chlorhexidine antiseptic solution was used only if pin site inflammation occurs.
Patients were followed up weekly during the distraction period and then every 2 weeks till frame removal. All frames were dynamized 2 weeks before removal.
Healing was determined radiologically and clinically: radiologically, callus bridging the fracture site and the appearance of three cortices bridging the distraction corticotomy on antero-posterior and lateral radiographs indicated healing. Clinical fracture healing was determined when the patient was able to bear weight freely without supporting aids after frame dynamization.
The final follow-up was done after 12 months using the IOWA [13] knee and ankle functional score and Paley and Maar’s bone results [4].
Results
Fifteen fractures healed uneventfully (Fig. 3). The mean healing time was 23.4 weeks (range 14–30). The mean consolidation time for the distraction site was 19 weeks (range 10–24). No bone healing stimulating procedures were needed for either the fracture or distraction site (Table 2). The mean length gained (the transported distance) was 39.4 (range 20–50) mm.
Pin site infection was the most common problem encountered in almost all patients and treated with oral antibiotics. None progressed to deep infection or required exchange of wires or half pins.
One patient (with 42-C3 diaphyseal fracture) was not able to tolerate the procedure; the frame was removed prematurely. A back slab was applied temporarily for 4 weeks until consolidation of the distraction gap. Revision of fixation was performed with an unreamed interlocking nail and iliac crest bone graft used. This patient was excluded from the final functional assessment and was rated as a poor bony result due to failure of the bone transport procedure alone to achieve healing.
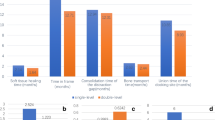
The IOWA knee and ankle score was used for assessment of the 15 patients who completed treatment. The functional outcome for the knee was excellent in 11 patients, good in three and fair in one. The ankle score was excellent in 12 patients, good in two and fair in one. The patient who did not complete treatment with bone transport was not included in this final functional assessment and was considered as a failure of the procedure.
According to Paley and Maar’s scoring system, bone results for all 16 patients were excellent in 14 patients, good in one patient and poor in the patient who had failure of the procedure.
Discussion
High-energy fractures have soft tissue compromise and a potentially reduced viability of bone ends which can alter the normal healing process with considerable delay in union expected. The method chosen for treatment of these fractures has a substantial effect on the local mechanical and biological environment. The treatment strategy for these fractures focuses on fixation stability while respecting the biological reserve.
Restoration of limb length and alignment together with preservation of function are the main goals in treatment of these injuries. Severely comminuted metaphyseal fractures challenge the ability of standard implants to provide adequate stability. Fixation by plates and screws pose an additional surgical injury to an already compromised soft tissue envelope, even with minimally invasive plate designs. Furthermore, the presence of a segmental gap or defect will compromise the stability of plate fixation; when prolonged bone healing time is expected, failure may occur by cantilever loading [5, 14].
The use of intramedullary nails in comminuted fractures with contained metaphyseal defects is not suitable. Short metaphyseal proximal tibial or distal femoral segments are difficult to control and malalignment can be difficult to avoid, even with the use of nails with multidirectional locking screws [5, 15].
The Ilizarov external fixator can be applied with minimal soft tissue disruption. Moreover, it offers the mechanical advantage of resisting all prevailing loads except the axial ones that are beneficial for osteogenesis. The multidirectional fixation can adequately stabilize short metaphyseal segments allowing early weight bearing and rehabilitation; additionally, it has the versatility for correcting any residual postreduction deformities.
A severely comminuted fracture forms a “contained defect” comprised of fracture fragments with reduced viability. In this series, the bone transport technique was used knowing corticotomy increases blood flow to the limb [16] and the transported bone segment is able to bridge the area of the contained defect and avoid need for bone graft.
Pin site infections encountered in all patients were successfully controlled with oral antibiotics. This is considered a problem of external fixation used in limb reconstruction as opposed to an obstacle or true complication as described by Paley [17]. The only true complication was the non-union encountered with one patient with the diaphyseal fracture who did not tolerate the procedure.
The functional outcome in this series indicates the limited knee and ankle range of motion that can be encountered in some patients treated by Ilizarov method is temporary and can be resolved after frame removal. Early postoperative knee and ankle range of motion exercises are imperative to avoid this problem.
The mean time to bone healing was 23.4 weeks which the authors consider as a reasonable time for such fractures. This is comparable to the healing time reported for complex and segmental fractures stabilized by circular fixators [9, 10, 18].
Conclusion
We describe a technique of bone transport to stimulate and overcome the comminution in high-energy fractures of the tibia and femur using the Ilizarov fixator as an alternative to other methods of stabilization with or without bone graft. The results presented confirm the suitability of the strategy for this cohort of patients who have metaphyseal fractures with total circumferential comminution involving more than 4 cm of the bone length.
References
Ilizarov GA, Ledyaev VI (1992) The replacement of long tubular bone defects by lengthening distraction osteotomy of one of the fragments. Clin Orthop Relat Res 280:7–10
Green SA, Jackson JM, Wall DM, Marinow H, Ishkanian J (1992) Management of segmental defects by the Ilizarov intercalary bone transport method. Clin Orthop Relat Res 280:136–142
Song HR, Cho SH, Koo KH, Jeong ST, Park YJ, Ko JH (1998) Tibial bone defects treated by internal bone transport using the Ilizarov method. Int Orthop 22(5):293–297
Paley D, Maar DC (2000) Ilizarov bone transport treatment for tibial defects. J Orthop Trauma 14(2):76–85
Keating JF, Simpson AH, Robinson CM (2005) The management of fractures with bone loss. J Bone Joint Surg Br 87(2):142–150
Blick SS, Brumback RJ, Lakatos R, Poka A, Burgess AR (1989) Early prophylactic bone grafting of high-energy tibial fractures. Clin Orthop Relat Res 240:21–41
Court-Brown CM, McQueen MM, Quaba AA, Christie J (1991) Locked intramedullary nailing of open tibial fractures. J Bone Joint Surg Br 73(6):959–964
Sledge SL, Johnson KD, Henley MB, Watson JT (1989) Intramedullary nailing with reaming to treat non-union of the tibia. J Bone Joint Surg Am 71(7):1004–1019
Giotakis N, Panchani SK, Narayan B, Larkin JJ, Al Maskari S, Nayagam S (2010) Segmental fractures of the tibia treated by circular external fixation. J Bone Joint Surg Br 92(5):687–692
Foster PA, Barton SB, Jones SC, Morrison RJ, Britten S (2012) The treatment of complex tibial shaft fractures by the Ilizarov method. J Bone Joint Surg Br 94(12):1678–1683
Marsh JL, Slongo TF, Agel J, Broderick JS, Creevey W, DeCoster TA, Prokuski L, Sirkin MS, Ziran B, Henley B, Audigé L (2007) Fracture and dislocation compedium - 2007: orthopedic trauma association classification, database and outcomes committee. J Orthop Trauma 21(10 suppl):S1–S133
Tscherne H, Gotzen L (eds) (1984) Fractures with soft tissue injuries (German). Telger TC (trans). Springer, Berlin, pp 1–9
Merchant TC, Dietz FR (1989) Long-term follow-up after fractures of the tibial and fibular shafts. J Bone Joint Surg Am 71(4):599–606
Fulkerson E, Egol KA, Kubiak EN, Liporace F, Kummer FJ, Koval KJ (2006) Fixation of diaphyseal fractures with a segmental defect: a biomechanical comparison of locked and conventional plating techniques. J Trauma 60(4):830–835
Lindvall E, Sanders R, Dipasquale T, Herscovici D, Haidukewych G, Sagi C (2009) Intramedullary nailing versus percutaneous locked plating of extra-articular proximal tibial fractures: comparison of 56 cases. J Orthop Trauma 23(7):485–492
Aronson J (1994) Temporal and spatial increases in blood flow during distraction osteogenesis. Clin Orthop Relat Res 301:124–131
Paley D (1990) Problems, obstacles, and complications of limb lengthening by the Ilizarov technique. Clin Orthop Relat Res 250:81–104
Ozturkmen Y, Karamehmetoglu M, Karadeniz H, Azboy I, Caniklioglu M (2009) Acute treatment of segmental tibial fractures with the Ilizarov method. Injury 40(3):321–326
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Thakeb, M.F., Mahran, M.A. & El-Motassem, EH.M. Bone transport for the management of severely comminuted fractures without bone loss. Strat Traum Limb Recon 11, 19–24 (2016). https://doi.org/10.1007/s11751-016-0241-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11751-016-0241-y