ABSTRACT
BACKGROUND
Although others have reported national disparities in the quality of diabetes care between the Veterans Affairs (VA) and private health care delivery systems, it is not known whether these differences persist among internal medicine resident providers in academic settings.
OBJECTIVE
We compared the quality of diabetes primary care delivered by resident physicians in either a private academic health care system (AHS) or its affiliated VA health care system.
DESIGN
Cross-sectional observational study
PARTICIPANTS
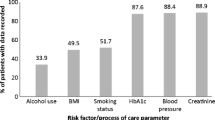
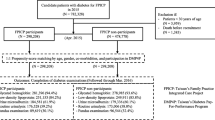
We included patients who: had a diagnosis of diabetes, had >2 primary care visits with the same resident provider during 2005, and were not separately managed by an attending physician or endocrinologist. A total of 640 patients met our criteria and were included in the analysis.
MEASUREMENTS AND RESULTS
Compared to the VA, patients in the AHS were more likely to be younger, female, have fewer medications, and be treated with insulin, but had less comorbidity. Patients in the VA were more likely to be referred for an annual eye exam (94% vs. 78%), receive lipid screening (88% vs. 74%), receive proteinuria screening (63% vs. 34%), and receive a complete foot exam (85% vs. 32%) in analyses adjusted for patient demographics and comorbidities (p-value <0.001 for all comparisons). In adjusted analyses, there were no significant differences in HbA1c, blood pressure, or LDL cholesterol control.
CONCLUSIONS
In spite of similar resident providers and practice models, there were substantial differences in the diabetes quality of care delivered in the VA and AHS. Understanding how these factors influence subsequent practice patterns is an important area for study.

Similar content being viewed by others
References
Holmboe ES, Bowen JL, Green M, et al. Reforming internal medicine residency training. A report from the Society of General Internal Medicine’s task force for residency reform. J Gen Intern Med. 2005;20(12):1165–72.
Fitzgibbons JP, Bordley DR, Berkowitz LR, Miller BW, Henderson MC. Redesigning residency education in internal medicine: a position paper from the Association of Program Directors in Internal Medicine. Ann Intern Med. 2006;144(12):920–6.
Weinberger SE, Smith LG, Collier VU. Redesigning training for internal medicine. Ann Intern Med. 2006;144(12):927–32.
Education ACfGM. ACGME Outcome Project: the general competencies. www.acgme.org. Accessed May 2009.
Bernard AM, Anderson L, Cook CB, Phillips LS. What do internal medicine residents need to enhance their diabetes care? Diabetes Care. 1999;22(5):661–6.
Miller CD, Ziemer DC, Doyle JP, et al. Diabetes management by residents in training in a municipal hospital primary care site (IPCAAD 2). Ethn Dis. 2005;15(4):649–55.
Ziemer DC, Doyle JP, Barnes CS, et al. An intervention to overcome clinical inertia and improve diabetes mellitus control in a primary care setting: improving primary care of African Americans with Diabetes (IPCAAD) 8. Arch Intern Med. 2006;166(5):507–13.
Mladenovic J, Shea JA, Duffy FD, Lynn LA, Holmboe ES, Lipner RS. Variation in internal medicine residency clinic practices: assessing practice environments and quality of care. J Gen Intern Med. 2008;23(7):914–20.
McGlynn EA, Asch SM, Adams J, et al. The quality of health care delivered to adults in the United States. N Engl J Med. 2003;348(26):2635–45.
Saaddine JB, Engelgau MM, Beckles GL, Gregg EW, Thompson TJ, Narayan KM. A diabetes report card for the United States: quality of care in the 1990s. Ann Intern Med. 2002;136(8):565–74.
Berlowitz DR, Ash AS, Hickey EC, et al. Inadequate management of blood pressure in a hypertensive population. N Engl J Med. 1998;339(27):1957–63.
Berlowitz DR, Ash AS, Hickey EC, Glickman M, Friedman R, Kader B. Hypertension management in patients with diabetes: the need for more aggressive therapy. Diabetes Care. 2003;26(2):355–9.
el-Kebbi IM, Ziemer DC, Musey VC, Gallina DL, Bernard AM, Phillips LS. Diabetes in urban African-Americans. IX. Provider adherence to management protocols. Diabetes Care. 1997;20(5):698–703.
Stevens DP, Wagner EH. Transform residency training in chronic illness care – now. Acad Med. 2006;81(8):685–7.
Jha AK, Perlin JB, Kizer KW, Dudley RA. Effect of the transformation of the Veterans Affairs Health Care System on the quality of care. N Engl J Med. 2003;348(22):2218–27.
Asch SM, McGlynn EA, Hogan MM, et al. Comparison of quality of care for patients in the Veterans Health Administration and patients in a national sample. Ann Intern Med. 2004;141(12):938–45.
Ross JS, Keyhani S, Keenan PS, et al. Use of recommended ambulatory care services: is the Veterans Affairs quality gap narrowing? Arch Intern Med. 2008;168(9):950–8.
Kerr EA, Gerzoff RB, Krein SL, et al. Diabetes care quality in the Veterans Affairs Health Care System and commercial managed care: the TRIAD study. Ann Intern Med. 2004;141(4):272–81.
DesRoches CM, Campbell EG, Rao SR, et al. Electronic health records in ambulatory care–a national survey of physicians. N Engl J Med. 2008;359(1):50–60.
Perkins AJ, Kroenke K, Unutzer J, et al. Common comorbidity scales were similar in their ability to predict health care costs and mortality. J Clin Epidemiol. 2004;57(10):1040–8.
Murcia AM, Hennekens CH, Lamas GA, et al. Impact of diabetes on mortality in patients with myocardial infarction and left ventricular dysfunction. Arch Intern Med. 2004;164(20):2273–9.
Fleming BB, Greenfield S, Engelgau MM, Pogach LM, Clauser SB, Parrott MA. The Diabetes Quality Improvement Project: moving science into health policy to gain an edge on the diabetes epidemic. Diabetes Care. 2001;24(10):1815–20.
Saaddine JB, Cadwell B, Gregg EW, et al. Improvements in diabetes processes of care and intermediate outcomes: United States, 1988–2002. Ann Intern Med. 2006;144(7):465–74.
Suwattee P, Lynch JC, Pendergrass ML. Quality of care for diabetic patients in a large urban public hospital. Diabetes Care. 2003;26(3):563–8.
Bozkurt B, Agoston I, Knowlton AA. Complications of inappropriate use of spironolactone in heart failure: when an old medicine spirals out of new guidelines. J Am Coll Cardiol. 2003;41(2):211–4.
Lied TR, Kazandjian VA. A Hawthorne strategy: implications for performance measurement and improvement. Clin Perform Qual Health Care. 1998;6(4):201–4.
Demakis JG, Beauchamp C, Cull WL, et al. Improving residents’ compliance with standards of ambulatory care: results from the VA Cooperative Study on Computerized Reminders. JAMA. 2000;284(11):1411–6.
Higashi T, Shekelle PG, Adams JL, et al. Quality of care is associated with survival in vulnerable older patients. Ann Intern Med. 2005;143(4):274–81.
Dunlay SM, Alexander KP, Melloni C, et al. Medical records and quality of care in acute coronary syndromes: results from CRUSADE. Arch Intern Med. 2008;168(15):1692–8.
Acknowledgements
This research was supported by the The Joseph C. Greenfield, Jr. Scholars Endowment. The first author (BJP) was supported by a KL2 career development award through Duke University and the NIH (KL2 RR024127). This research was presented as a poster at the VA HSR&D 2009 National Meeting in Baltimore, MD, on February 11, 2009. The authors would also like to acknowledge Beverly McCraw, Jennette Wood Crowley and Mike Harrelson for their assistance with data collection.
Conflicts of Interest
The authors have no conflicts of interest to report.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Powers, B.J., Grambow, S.C., Crowley, M.J. et al. Comparison of Medicine Resident Diabetes Care Between Veterans Affairs and Academic Health Care Systems. J GEN INTERN MED 24, 950–955 (2009). https://doi.org/10.1007/s11606-009-1048-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-009-1048-z