Abstract
Background
Primary health care system plays a central role in caring for persons with diabetes. Thai National Health Examination Survey (NHES) reports that only 40% of patients with type 2 diabetes mellitus (T2DM) achieve optimal glycemic control. We sought to evaluate the quality of diabetic care (QOC), prevalence of microvascular complications, and associated risk factors among T2DM patients treated at primary care units in urban areas in Thailand.
Methods
A population-based, cross-sectional study of 488 T2DM patients aged over 35 years from 25 primary care units in Samutsakhon, Thailand was conducted during February 2018 to March 2019. Clinical targets of care (TOC) and processes of care (POC) were measured to evaluate QOC. Multivariate logistic regression models were applied to explore the association between risk factors and glycemic control.
Results
41.2% of women and 44.4% of men achieved hemoglobin A1C (A1C) < 53 mmol/mol, while 31.3% of women and 29.7% of men had poor glycemic control (A1C > 63 mmol/mol). 39 participants (8%) achieved all TOC and 318 participants (65.2%) achieved all POC. Significant risk factors for poor glycemic control included diabetes duration > 6 years (AOR = 1.83, 95% CI = 1.20–2.79), being overweight (AOR = 2.54, 95% CI = 1.58–4.08), obesity (AOR = 1.71, 95% CI = 1.05–2.89), triglycerides > 1.7 mmol/l (AOR = 1.81, 95% CI = 1.25–2.78), low density lipoprotein-cholesterol (LDL-C) ≥ 2.6 mmol/l (AOR = 1.55, 95% CI = 1.04–2.28). On the other hand, participants aged > 65 years (AOR = 0.25, 95% CI = 0.14–0.55) or achieved TOC indicators (AOR = 0.69, 95% CI = 0.43–0.89) were significantly associated with glycemic control. Diabetic retinopathy was significantly related to obesity (AOR = 2.21, 95% CI = 1.00–4.86), over waist circumference (AOR = 2.23, 95% CI = 0.77–2.31), and diastolic blood pressure > 90 mmHg (AOR = 1.81, 95% CI = 1.48–1.96).
Conclusion
Access to essential diabetic screening in primary care units is crucial to determine status of disease control and guide disease management. Duration of T2DM, high body mass index, triglyceride and LDL-C were independently associated with poor glycemic control. Obesity was highly associated with diabetes retinopathy. Effort should be taken seriously toward monitoring these factors and providing effective care.
Similar content being viewed by others
Introduction
Type 2 diabetic mellitus (T2DM) is one of increasingly prevalent non-communicable diseases (NCDs) worldwide. According to Thai National Health Examination Surveys (NHES) during 2004–2014 [1,2,3] and the International Diabetes Federation [4], the prevalence of Thai T2DM increased from 7.7% in 2004 to 7.8% in 2009, then to 9.9% in 2014. Diabetes is the leading cause of chronic kidney disease and death worldwide [5]. Thanks to a national program in Thailand to promote access to assessment of people at an increased risk for NCDs, the proportion of Thai persons with undiagnosed diabetes declined from 65.2% to 51.2% in men and from 48.5% to 41.3% in women between 2004 and 2014 [1,2,3]. The proportion of well-controlled glycemia improved from 15% in 2004 to 36% in 2012, and to 40% in 2014 [6]. Nearly half of the direct medical cost of diabetes is allocated to hospital care or the cost of managing complications, and only 14% to outpatient or community care [7].
Diabetic persons with complications require 2.3–18.5 times more resources, and suffer poorer quality of life [7]. Growing inequalities in healthcare for people who live in rural and urban communities are observed generally [8]. Recent data in Thailand have shown that individuals with T2DM treated at regional hospitals had a better glycemic control than that of individuals from local hospitals. This implies that more comprehensive care provided by a medical team in regional hospitals and more urbanized patients may produce better clinical outcomes or high rates of awareness of diabetes than in rural patients [9]. In addition, education and behavioral support are especially crucial for individuals attempting for improvement of T2DM and prevention of early complications. Since 2002, concerted efforts have been made to institute comprehensive care to most diabetic individuals through the primary health care system, and particularly to those living in communities under the universal health care scheme (UHC). This provides free health care at the point of service in order to guarantee access to essential health care at primary care units (PCUs) [10]. Moreover, a resilient health system and management support team are a fundamental tenet of the diabetes care model linked to improved outcomes of diabetes control [11]. Services include health promotion, education, and screening for risk factors that lead to diabetes complications driven by interdisciplinary collaboration, proactive policies, and holistic care approaches [10, 12, 13]. This concept is also aligned with the guidelines of team-based care outlined by the Institute of Medicine (IOM) and the American Association of Colleges of Nursing (AACN), which recognize the patient as the center of the care team and must be aligned with cost containment mechanisms of a UHC to ensure long-term governmental financial sustainability [11].
To improve diabetes outcomes and actively prevent complications, it is useful to assess and monitor the quality of care (QOC), access to processes of care (POC) and achievement of clinical targets of care (TOC) [14, 15]. These metrics are associated with reduction and delayed onset of microvascular and macrovascular complications [15,16,17,18,19]. For instance, maintenance of blood pressure below 140/90 mmHg is recognized to reduce cardiovascular events and microvascular complications such as stroke, albuminuria, retinopathy, and chronic kidney disease (CKD), leading to overall benefits for populations at risk [14, 20,21,22,23]. Subgroup analysis of diabetic participants and large meta-analyses demonstrated a significant reduction in all-cause deaths for every 1.01 mmol/l reduction in low density lipoprotein-cholesterol (LDL-C) [24] and the protective benefits of statin, thereby reducing fatal and non-fatal cardiovascular outcomes [25, 26]. Diabetic nephropathy (DN) and diabetic retinopathy (DR) are clearly associated with poor glycosylated A1C and prolonged duration of diabetes [15, 19]. Optimal glycemic and blood pressure control can attenuate the progression of CKD and vision-threatening DR [27]. Interestingly, the most common barriers to glycemic control include improper psychological/support, low socioeconomic status, and insufficient access to essential care [28].
Therefore, we aimed to evaluate the results of T2DM care and determine the association between quality of glycemic control and the care system through accessibility of diabetic complication screening, and successful achievement of outcome goals in urban areas of Samutsakhon province, Thailand.
Materials and methods
Study population
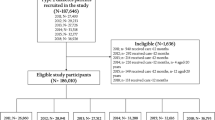
Baseline data were collected from 25 primary care units in 18 urban communities, in Samutsakhon province, Thailand. Among 13,256 patients, 6,871 had been diagnosed with T2DM whose care was provided by collaborative primary care providers (PCP) including family physicians, general practitioners, pharmacists and nurses, and the average wait time to visit a PCP was 2–3 months. Approximately 97% of these patients were all-insured, indicating there was no significant discrepancy in quality of diabetes care. Complication screening and complete blood measurement were set up during the annual checkup campaign of each PCU. All primary care units operated under a standard protocol that included guidelines of diabetic treatments according to the American Diabetes Association (ADA)’s recommendations [29] and the Thai clinical practice guideline for diabetes [30], standard anti-diabetic drugs, clinical investigations, and referral system. Participants were recruited in routinely scheduled visits during February 2018 to March 2019. Written informed consent was obtained from all participants. All procedures were approved by the Siriraj Institutional Review Board (095/2560 (EC1)). Participants were eligible for inclusion if they had received care and treatment for T2DM at least for 12 months. Pregnant participants and those with gestational diabetes or at their postpartum stage were excluded. Data were collected through face-to-face interviews and a case record form was completed by research coordinators using standardized questionnaires.
Data collection
Standardized questionnaires comprised demographic data and self-reported comorbidities such as hypertension, dyslipidemia, gout, chronic kidney disease, and a family history of NCDs. Anthropometric information was retrieved from an electronic medical record. Date of diagnosis, behavioral risk factors, and lifestyle (physical activities, smoking and alcohol consumption) were also collected. The recent use of antidiabetic agents, antihypertensive agents, lipid lowering agents and antiplatelet therapies were retrieved from the medical record. Physical activities or exercise were classified into three categories: (1) less than once a week or seldom, (2) once a week, (3) at least 2–3 times a week. Smoking was classified into three categories: (1) never, (2) quit smoking, and (3) current smoking. Alcohol consumption was classified into two categories: (1) yes or drinking and (2) no or never drinking. Body mass index (BMI) was classified as (1) underweight < 18.5 kg/m2, (2) normal 18.5–22.9 kg/m2, (3) overweight 23.0–24.9 kg/m2, (4) obese I 25.0- 29.9 kg/m2, and (5) obese II ≥ 30.0 kg/m2. Waist circumference (WC) was classified as (1) normal (< 90 cm in men and < 80 cm in women) and (2) over. Optimal blood pressure (BP) was defined by systolic blood pressure (SBP) < 140 mmHg and diastolic blood pressure (DBP) < 90 mmHg as defined the American College of Cardiology/American Heart Association Task Force and the American Diabetes Association [14, 31].
Measurements
Laboratory data including fasting blood glucose (FBG), A1C, total cholesterol (TC), triglycerides (TG), high-density lipoprotein (HDL-C) were retrieved from the medical record within the preceding 9 months. LDL-C was estimated based on the Friedewald formula [32]. Plasma uric acid levels, liver functions (aspartate transaminase; AST, and alanine aminotransferase; ALT) and electrolytes (sodium; Na+ and potassium; K+) were determined by a Cobas 6000 clinical chemistry analyzer (Roche Diagnostics, Basel, Switzerland).
Quality of Care (QOC) assessment
QOC [6, 15] comprised TOC and POC. TOC included the ABC indicators of diabetes: A-A1C, B-BP, and C-LDL-C. POC was the receipt of essential diabetes examinations, including the FACE indicators of diabetes: F-Foot exam, A-A1C exam, C-LDL-C exam, and E-eye exam. In addition, aggregates of the QOC measures were generated for TOC (AllABC), POC (AllFACE), and all QOC indicators (a combination of TOC and POC). AllABC represented all three of the treatment goals achieved. AllFACE represented an indicator variable for cases where all four POC were conducted. All7Q represented an indicator variable of whether all seven of the clinical indicators were achieved, including AllABC and AllFACE. Finally, the count variable Num7Q represented the number of TOC and POC outcomes achieved (0, 1, 2, 3, 4, 5, 6 or 7). Participants were considered as satisfactory for achievement of clinical targets if A-A1C ≤ 53 mmol/mol, B-BP ≤ 130/80 mmHg, and C-LDL-C < 2.6 mmol/l. Participants were considered to have satisfactorily met the examination target if they were examined once in the previous 12 months for A1C, cholesterol, feet and eyes. Moreover, all QOC was also compared the effectiveness with previous studies.
Complication data collection
Data were collected on complications including cerebrovascular accident, cerebral infarction, ischemic stroke, hemorrhagic stroke, DR, DN, renal insufficiency, and neuropathy. Retinal photography during the year prior to enrollment was retrieved from the medical record. If this had not been performed, subjects were scheduled for retinal screening using a non-mydriatic seven-field stereoscopic retinal photography (KOWA nonmyd 8S, Kowa, Tokyo, Japan) by a trained technical specialist. Results were verified by an ophthalmologist. DR was defined as the presence of at least one microaneurysm, hemorrhage, or evidence of proliferative retinopathy. DR was reported into three categories: (1) normal or no-DR, (2) non-proliferative diabetic retinopathy (NPDR; mild, moderate or severe), and (3) proliferative diabetic retinopathy (PDR). Techniques and standards [33, 34] for diagnosing retinopathy did not change over the period of the study. To assess renal insufficiency, spot morning urine collected at the clinics was sent to the main lab facility, and stored at 4 °C until processing. To determine albuminuria, spot morning urine albumin was measured by an immunoturbimetric assay and creatinine using the enzymatic colorimetric method. Then, the urine albumin-to-creatinine ratio (ACR) was calculated. Staging of DN was categorized according to the Kidney Disease Improving Global Outcomes (KDIGO) 2012 guidelines [35, 36]: microalbuminuria and macroalbuminuria as well as serum creatinine (Cr), estimated glomerular filtration rate (eGFR). The presence of neurological problems of the feet was evaluated using monofilament (10 ng). Skin and nail characteristics, the presence of foot deformities, and the risk of foot ulcers were evaluated by well-trained nurses in all participants. Briefly, nurses inspected for visible abnormalities, peripheral pulse palpation and monofilament testing [37].
Statistical analyses
Continuous variables were described using means, and standard error of mean (SEM), whereas categorical variables were summarized using counts and percentages. Comparisons between groups were analyzed by independent t-test or Chi-square test, when appropriate. Logistic regression was used to estimate odds ratio (OR) and 95% confidence interval (95% CI) for predictive factors associated with glycemic control. All risk factors were analyzed first in univariate logistic analyses and included in the initial multivariate model if an association existed (p-value < 0.2). Variables were eliminated in the final model, if they were not associated with glycemic control (p-value < 0.05). Confounders were identified if they altered the remaining coefficients by greater than 20% after their removal from the model. If a variable was identified as a confounder, it was forced into the final model. Our results indicate that age and HDL were confounding factors of glycemic control. Therefore, we have addressed the confounding variables appropriately. Statistical analyses were performed using STATA version 15.0 (Stata Corporation, College Station, TX, USA).
Results
General characteristics of the study participants
Four hundred and eighty-eighth participants were enrolled with the average age of 64.3 ± 0.61 years in women and 63.4 ± 1.07 years in men (Table 1). The average duration of diabetes in women was greater than in men (7.4 ± 0.28 years vs. 5.4 ± 0.34 years, p = 0.002). Based on BMI and WC, approximately two-third of participants were obese. No differences between genders were observed in SBP and self-reported underlying diseases. Men were more likely to consume alcohol and to be current smokers than women (p < 0.001).
Clinical characteristics
41.2% of women and 44.4% of men achieved optimal glycemic control as defined by A1C < 53 mmol/mol. One third of both genders had poor glycemic control (A1C > 63 mmol/mol). Women had significantly higher HDL-C levels than men (1.32 ± 0.17 vs. 1.23 ± 0.03 mmol/l, p = 0.009). 279 participants (61.4% in men and 60.2% in women) had an LDL-C level of < 2.6 mmol/l and 354 participants (71.4% in men and 76.2% in women) had an eGFR > 59 ml/min/1.73m2 (Table 2).
QOC
Nearly 40% of participants achieved glycemic and blood pressure targets (Table 3). Only 39 participants (8.0%) achieved AllABC goals and 28 participants (5.7%) achieved all7Q goals, while 318 participants (65.2%) achieved AllFACE. DR and risk of foot ulcers were found in 47 (13.6%) and 40 (8.9%) participants, respectively (Table 4). Albuminuria was tested in only 12 participants (data not shown); therefore,the prevalence of DN was not estimated.
Logistic regression models
The association between variables and glycemic control was analyzed by multivariate logistic regression (Table 5). Risk factors independently related to the quality of glycemic control (referred by A1C < 53.0 vs. ≥ 53.0 mmol/mol) including age, overweight and obesity, diabetes duration, TG, LDL-C, and TOC achievement. Older patients (age > 65 years) achieved better glycemic control than younger patients. Glycemic control was negatively associated with being overweight (AOR = 2.54, 95% CI = 1.58–4.08, p < 0.001), obese (AOR = 1.71, 95% CI = 1.05–2.89, p = 0.045), diabetes duration > 6 years (AOR = 1.83, 95% CI = 1.20–2.79, p = 0.005), TG ≥ 1.7 mmol/l (AOR = 1.81, 95% CI = 1.25–2.78, p = 0.019) and LDL-C ≥ 2.6 mmol/l (AOR = 1.55, 95% CI = 1.04–2.28, p = 0.039). Moreover, participants who achieved TOC-target indicators significantly had better glycemic control (AOR = 0.69, 95% CI = 0.43–0.89, p = 0.034).
Risk factors significantly associated with DR included obese (I, II) based on BMI, increased DBP and WC (Table 6). Obese participants (AOR = 2.21, 95% CI = 1.00–4.86, p = 0.046) and large WC (AOR = 2.23, 95% CI = 0.77–2.31, p = 0.021) were strongly correlated with DR. Additionally, participants with higher DBP level were 1.81 times more likely to have DR complication (AOR = 1.81, 95% CI = 1.48–1.96, p = 0.049). Therefore, these anthropometric indicators should be closely monitored to prevent and reduce risk of microvascular complications in T2DM patients. Unfortunately, our study did not find any association between DR complication, A1C levels, and the QOC indicators.
Discussion
Attainment of good glycemic control and regular screening for comorbidities are essential aspects of T2DM management. These goals help prevent or delay microvascular, macrovascular complications, organ damage, and death [38,39,40]. Risk factor modification, combined with therapeutic care, improves overall outcomes and well-being. Our study demonstrated that access to critical tests managed by primary care professionals generally reaches acceptable targets (POC and AllFACE). The concept of "process of care" in this study was mainly referred to as the receipt of essential diabetes examinations, i.e., the FACE indicators. However, from a health services research perspective, the process of care is also a reflection of the physician–patient encounters in the primary care setting which takes into account patients’ healthcare needs and minimize treatment burden. Existing evidence suggests that the sustainability of long-term improvements of glycemic control remains a major challenge in the prevention and control of diabetes and its complications [41, 42]. A recent multi-site evaluation from patients' perspectives demonstrated that an improvement in primary care patients' experiences was significantly associated with reduced treatment burden [43]. Efforts to improve the process of care that takes into account a wider context of service delivery would help in strengthening patients' long-term adherence to diabetic care [44]. Moreover, strengthening the capacity building of primary care physicians and multidisciplinary teams are also important to achieve a more holistic approach towards an optimised delivery of primary care. Interestingly, most patients in this study could access to LDL-C examination and achieve LDL-C target. However, an LDL-C 2.6 mmol/l or lower can be achieved by pharmacological treatment rather than behavioral modification alone in this setting. This is likely because adherence to a healthy lifestyle is challenging especially on maintenance of body weight and healthy dietary consumption [45]. Moreover, optimal glycemic and BP control are more challenging since these two are subject to family and social encouragement and socioeconomic changing, and require multidisciplinary collaboration and patient compliance [46, 47].
A multi-center cross-sectional study in 26,869 Thai patients from 595 hospitals showed that larger hospitals and hospitals having a specialized diabetes clinic outperformed general medical clinics regarding accessibility, effectiveness, and quality of diabetes care. For example, they showed that achievement of essential process of care and quality of care (AllFACE and AllABC) were reported to be 19.3–29.6% and 8.4–10.5%, respectively [6]. De Berardis et al., showed in a prospective study of 3,437 Italian patients treated by different specialties in 125 diabetes clinics and 103 general practice clinics that care supervised in diabetes clinics related with better clinical outcome goals than general clinics [48]. However, we found that in our getting, achievement of these indicators was 65% and 8%, respectively, especially in the achievement of LDL-C clinical target. This large discrepancy between a proportion of patients who met the POC and TOC may due to the nature of diabetes, financial burden, work and environment related factors. Recent statement from the American College of Lifestyle Medicine suggested that an ability of diabetes control or even diabetes remission is related to its intensity of preventive interventions [11]. Therefore, it is explainable that this result will help us drive the healthcare system that we then need to use our data to implement more intense interventions with patients to improve TOC indicators.
There are possible explanations why diabetes care at these PCUs could outperform larger scale hospital-based clinics in terms of T2DM care. First, primary care physicians and health care professionals in PCUs are familiar with patients with longer-term, doctor-patient relationships. Second, access to medical care in PCUs was limited in the past. Therefore, over the past 4 decades, Thailand has focused on considerable investment and implementation in strengthening its primary health care system, especially at PCUs.
Our findings demonstrated that high BMI, advanced age, duration of diabetes of 6 years or more, TG of 1.7 mmol/l or more, and LDL-C of 2.6 mmol/l or more, are significantly associated with poorer glycemic control. These parameters reflect key characteristics of the metabolic syndrome: poor glycemic control and central obesity [49]. It is well known that time since diagnosis (i.e. disease duration) increases the risk of mortality as well as chronic complications [12, 50,51,52,53]. Due to the long asymptomatic stage of diabetes, most diabetic patients fail to achieve a healthy metabolic lifestyle, leading to poor glycemic control and complications. Elevated BMI was associated with progressively higher risk for all T2DM complications, even more so for women than for men [53]. Although our study did not find any association between neck circumference and DM development, its relationship was reported in other studies. In 2021, a prospective multi-center study determined the association between neck circumference and the incidence of cardiovascular events in T2DM patients and were followed up for a 10-year period in Beijing communities. A higher neck circumference was associated with a higher risk of cardiovascular events by 40% in T2DM patients [54]. In 2019, meta-analysis of a cross-sectional design reported that neck circumference was positive correlated with glycemic indicators including fasting plasma glucose, serum fasting insulin level, and A1C [55]. Moreover, neck circumference was also positively correlated with fasting plasma glucose, A1C in patients with hypertension [56]. In 2015, neck circumference was also positive correlated with most factors related to obesity, glucose metabolism, and lipid parameters in both genders [57]. Therefore, neck circumference was easily measured for fat deposit, which might be a predictive risk factor for cardiovascular development and glycemic indicators.
The quality of lipid control was significantly related to glycemic control. It was reported that there was a significant positive correlation between A1C and lipid profile including TC, TG, and LDL-C [58]. Patients with A1C lower than 53.0 mmol/mol had significantly better values of TC, LDL-C, and LDL-C/HDL-C ratio, as compared with ones with A1C > 53.0 mmol/mol [59]. Therefore, the lipid profile could be used as a potential biomarker for predicting glycemic control and the early detection of elevated.
In our study, A1C (≥ 53.0 mmol/mol) was not statistically associated with DR but there were a moderate and a high risk of foot ulcers or wounds. A retrospective cohort study of diabetic patients at the Johns Hopkins Wound Center demonstrated that well-controlled A1C was significantly associated with faster wound-area healing rate [60]. The most common location of wounds was at the lower extremities including legs, ankles and feet. Besides, there may be a relationship between faster wound-healing rate and lower A1C levels [60]. Moreover, the study of T2DM in South Indian using retrospective observational design demonstrated that poor glycemic control was associated with neuropathy, DR and DN [61]. Patients with DN were prone to have higher A1C which was associated with 1.49 times of having DN [12].
Our study has limitations. First, our study was cross-sectional design; therefore, measuring clinical targets, POC, TOC and patients’ characteristic data can be subject to time of assessment which may not represent overall care for all primary care units. Second, at the time of assessment the rate of albuminuria monitoring was low; therefore, we could not determine prevalence of DN and its associated variable risk factors. Third, at PCUs paper-based records were used in parallel with some electronic patient records to support different tasks including anthropometric information and peripheral blood glucose data; therefore, we could not retrieve all data from electronic medical records for the analyses.
In conclusion, in terms of QOC in PCUs, most diabetic patients receive essential diabetes examination but still cannot achieve goals of diabetic control. Diabetic retinopathy is a major microvascular complication in an urban population. Associated risk factors include diabetes longer than 6 years, obesity with abnormal lipid profiles were significantly at risk for poor glycemic control and diabetic retinopathy. The relationship between glycemic levels and lipid levels can be an early warning indicator for the development of vascular complications in T2DM participants. Therefore, all diabetic patients should be aware of both essential screening and goals of treatment to reduce risk of complications in future.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- T2DM:
-
Type 2 diabetic mellitus
- NCDs:
-
Non-communicable diseases
- NHES:
-
Thai National Health Examination Survey
- QOC:
-
Quality of diabetic care
- TOC:
-
Clinical targets of care
- POC:
-
Processes of care
- AOR:
-
Adjust odd ratio
- PCUs:
-
Primary care units
- DN:
-
Diabetes nephropathy
- DR:
-
Diabetes retinopathy
- A1C:
-
Glycosylated hemoglobin A1C
- ADA:
-
American Diabetes Association
- BMI:
-
Body mass index
- SBP:
-
Systolic blood pressure
- DBP:
-
Diastolic blood pressure
- FBG:
-
Fasting blood glucose
- TC:
-
Total cholesterol
- TG:
-
Triglycerides
- HDL-C:
-
High-density lipoprotein cholesterol
- LDL-C:
-
Low-density lipoprotein cholesterol
- AST:
-
Aspartate transaminase
- ALT:
-
Alanine aminotransferase
- NPDR:
-
Non-proliferative diabetic retinopathy
- PDR:
-
Proliferative diabetic retinopathy
- ACR:
-
Albumin-to-creatinine ratio
- KDIGO:
-
Kidney Disease Improving Global Outcomes
- Cr:
-
Creatinine
- eGFR:
-
Estimated glomerular filtration rate
- BP:
-
Blood pressure
- SEM:
-
Standard error of mean
- OR:
-
Odds ratio; CI: confidence interval
- WC:
-
Waist circumference
- UHC:
-
The universal health care
- IOM:
-
The Institute of Medicine
- AACN:
-
The American Association of Colleges of Nursing
- PCP:
-
Primary care providers
References
Aekplakorn W, Abbott-Klafter J, Premgamone A, Dhanamun B, Chaikittiporn C, Chongsuvivatwong V, et al. Prevalence and management of diabetes and associated risk factors by regions of Thailand: Third National Health Examination Survey 2004. Diabetes Care. 2007;30(8):2007–12.
Aekplakorn W, Chariyalertsak S, Kessomboon P, Sangthong R, Inthawong R, Putwatana P, et al. Prevalence and management of diabetes and metabolic risk factors in Thai adults: the Thai National Health Examination Survey IV, 2009. Diabetes Care. 2011;34(9):1980–5.
Aekplakorn W, Chariyalertsak S, Kessomboon P, Assanangkornchai S, Taneepanichskul S, Putwatana P. Prevalence of diabetes and relationship with socioeconomic status in the Thai population: National Health Examination Survey, 2004–2014. J Diabetes Res. 2018;2018:1654530.
International Diabetes Federation. IDF Diabetes Atlas-9th Edition [Internet]. 2019 Available from: https://www.diabetesatlas.org/upload/resources/material/20200302_133351_IDFATLAS9e-final-web.pdf#page=68&zoom=auto.
Toyama T, Furuichi K, Ninomiya T, Shimizu M, Hara A, Iwata Y, et al. The impacts of albuminuria and low eGFR on the risk of cardiovascular death, all-cause mortality, and renal events in diabetic patients: Meta-analysis. PLoS ONE. 2013;8(8):e71810.
Sieng S, Hurst C. A combination of process of care and clinical target among type 2 diabetes mellitus patients in general medical clinics and specialist diabetes clinics at hospital levels. BMC Health Serv Res. 2017;17(1):533.
Chatterjee S, Riewpaiboon A, Piyauthakit P, Riewpaiboon W, Boupaijit K, Panpuwong N, et al. Cost of diabetes and its complications in Thailand: A complete picture of economic burden. Health Soc Care Community. 2011;19(3):289–98.
Aung WP, Htet AS, Bjertness E, Stigum H, Chongsuvivatwong V, Kjøllesdal MKR. Urban-rural differences in the prevalence of diabetes mellitus among 25–74 year-old adults of the Yangon Region, Myanmar: two cross-sectional studies. BMJ Open. 2018;8(3):e020406.
Sakboonyarat B, Pima W, Chokbumrungsuk C, Pimpak T, Khunsri S, Ukritchon S, et al. National trends in the prevalence of glycemic control among patients with type 2 diabetes receiving continuous care in Thailand from 2011 to 2018. Sci Rep. 2021;11(1):14260.
Deerochanawong C, Ferrario A. Diabetes management in Thailand: A literature review of the burden, costs, and outcomes. Global Health. 2013;9(1):11.
Rosenfeld RM, Kelly JH, Agarwal M, Aspry K, Barnett T, Davis BC, et al. Dietary Interventions to Treat Type 2 Diabetes in Adults with a Goal of Remission: An Expert Consensus Statement from the American College of Lifestyle Medicine. Am J Lifestyle Med. 2022;16(3):342–62.
Mayurasakorn K, Somthip N, Caengow S, Chulkarat N, Wanichsuwan M. Glycemic control and microvascular complications among type 2 diabetes at primary care units. J Med Assoc Thai. 2009;92(8):1094–101.
Khamthana P, Meebunmak Y, Siramaneerat I. Exploring the type 2 diabetes management in the primary care setting in Ratchaburi province. Thailand Open Public Health J. 2019;12(1):56–60.
American Diabetes Association. Cardiovascular disease and risk management: Standards of medical care in diabetes. Diabetes Care. 2020;43(Supplement 1):S111–34.
Sonthon P, Promthet S, Changsirikulchai S, Rangsin R, Thinkhamrop B, Rattanamongkolgul S, et al. The impact of the quality of care and other factors on progression of chronic kidney disease in Thai patients with type 2 diabetes mellitus: A nationwide cohort study. PLoS ONE. 2017;12(7):e0180977.
Harris R, Donahue K, Rathore SS, Frame P, Woolf SH, Lohr KN. Screening adults for type 2 diabetes: A review of the evidence for the U.S. preventive services task force. Ann Intern Med. 2003;138(3):215–29.
Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). UK Prospective Diabetes Study (UKPDS) Group. Lancet. 1998;352(9131):837–53.
Robert T, Rury H, Irene S, Carole C, Valeria F, Susan M, et al. Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38 UK Prospective Diabetes Study Group. BMJ. 1998;317(7160):703–13.
Worswick J, Wayne SC, Bennett R, Fiander M, Mayhew A, Weir MC, et al. Improving quality of care for persons with diabetes: an overview of systematic reviews - what does the evidence tell us? Syst Rev. 2013;2:26.
Thomopoulos C, Parati G, Zanchetti A. Effects of blood-pressure-lowering treatment on outcome incidence in hypertension: 10 - Should blood pressure management differ in hypertensive patients with and without diabetes mellitus? Overview and meta-analyses of randomized trials. J Hypertens. 2017;35(5):922–44.
Emdin CA, Rahimi K, Neal B, Callender T, Perkovic V, Patel A. Blood pressure lowering in type 2 diabetes: A systematic review and meta-analysis. JAMA. 2015;313(6):603–15.
Xie X, Atkins E, Lv J, Bennett A, Neal B, Ninomiya T, et al. Effects of intensive blood pressure lowering on cardiovascular and renal outcomes: Updated systematic review and meta-analysis. Lancet. 2016;387(10017):435–43.
Cushman WC, Evans GW, Byington RP, Goff DC Jr, Grimm RH Jr, Cutler JA, et al. Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med. 2010;362(17):1575–85.
Mihaylova B, Emberson J, Blackwell L, Keech A, Simes J, Barnes EH, et al. The effects of lowering LDL cholesterol with statin therapy in people at low risk of vascular disease: Meta-analysis of individual data from 27 randomised trials. Lancet. 2012;380(9841):581–90.
Kearney PM, Blackwell L, Collins R, Keech A, Simes J, Peto R, et al. Efficacy of cholesterol-lowering therapy in 18,686 people with diabetes in 14 randomised trials of statins: A meta-analysis. Lancet. 2008;371(9607):117–25.
Knopp RH, d’Emden M, Smilde JG, Pocock SJ. Efficacy and safety of atorvastatin in the prevention of cardiovascular end points in subjects with type 2 diabetes: The Atorvastatin Study for Prevention of Coronary Heart Disease Endpoints in non-insulin-dependent diabetes mellitus (ASPEN). Diabetes Care. 2006;29(7):1478–85.
Liu L, Quang ND, Banu R, Kumar H, Tham Y-C, Cheng C-Y, et al. Hypertension, blood pressure control and diabetic retinopathy in a large population-based study. PLoS One. 2020;15(3):0229665-e.
Aronson R, Orzech N, Ye C, Brown RE, Goldenberg R, Brown V. Specialist-led diabetes registries and prevalence of poor glycemic control in type 2 diabetes: The Diabetes Registry Outcomes Project for A1C Reduction (DROP A1C). Diabetes Care. 2016;39(10):1711–7.
American Diabetes Association. Pharmacologic approaches to glycemic treatment: Standards of medical care in diabetes-2019. Diabetes Care. 2019;42(1Supplement_1):S90.
Diabetes Association of Thailand. Clinical practice guideline for diabetes 2017 [Internet]. Diabetes Association of Thailand. 2017. Available from: https://www.dmthai.org/index.php/knowledge/healthcare-providers/cpg/443-guideline-diabetes-care-2017.
Casay D, Thomas R, Bhalla V, Commodore-Mensah Y, Heidenreich P, Kolte D. AHA/ACC clinical performance and quality measures for adults with high blood pressure: A report of the American College of Cardiology/American Heart Association task force on performance measures. Cir Cardiovasc Qual Outcomes. 2019;12(11):e000057.
Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18(6):499–502.
Rate RG, Knowler WC, Morse HG, Bonnell MD, McVey J, Chervenak CL, et al. Diabetes mellitus in Hopi and Navajo Indians: Prevalence of microvascular complications. Diabetes. 1983;32(10):894.
Stratton IM, Adler AI, Neil HAW, Matthews DR, Manley SE, Cull CA, et al. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): Prospective observational study. BMJ. 2000;321(7258):405.
Stevens PE, Levin A. Evaluation and management of chronic kidney disease: synopsis of the kidney disease: improving global outcomes 2012 clinical practice guideline. Ann Intern Med. 2013;158(11):825–30.
Levin A, Stevens PE. Summary of KDIGO 2012 CKD guideline: Behind the scenes, need for guidance, and a framework for moving forward. Kidney Int. 2014;85(1):49–61.
Mayfield JA, Reiber GE, Sander LJ, Janisse D, Pogach LM. Preventice foot care in diabetes. Diabetes Care. 2004;27:S63.
Skyler JS. Effects of glycemic control on diabetes complications and on the prevention of diabetes. Clin Diabetes. 2004;22(4):162.
Vaag AA. Glycemic control and prevention of microvascular and macrovascular disease in the STENO 2 study. Endocr Pract. 2006;12(Supplement 1):89–92.
Simmons RK, Griffin SJ, Lauritzen T, Sandbæk A. Effect of screening for type 2 diabetes on risk of cardiovascular disease and mortality: A controlled trial among 139,075 individuals diagnosed with diabetes in Denmark between 2001 and 2009. Diabetologia. 2017;60(11):2192–9.
Hu XJ, Wu HF, Li YT, Wang Y, Cheng H, Wang JJ, et al. Influence of health education on clinical parameters in type 2 diabetic subjects with and without hypertension: A longitudinal, comparative analysis in routine primary care settings. Diabetes Res Clin Pract. 2020;170:108539.
Wang HHX, Li YT, Wong MCS. Leveraging the power of health communication: messaging matters not only in clinical practice but also in public health. Hong Kong Med J. 2022;28(2):103–5.
Hu XJ, Wang HHX, Li YT, Wu XY, Wang Y, Chen JH, et al. Healthcare needs, experiences and treatment burden in primary care patients with multimorbidity: An evaluation of process of care from patients’ perspectives. Health Expect. 2022;25(1):203–13.
Pati S, Pati S, van den Akker M, Schellevis FG, Sahoo KC, Burgers JS. Managing diabetes mellitus with comorbidities in primary healthcare facilities in urban settings: a qualitative study among physicians in Odisha, India. BMC Fam Pract. 2021;22(1):99.
Gant CM, Binnenmars SH, Harmelink M, Soedamah-Muthu SS, Bakker SJL, Navis G, et al. Real-life achievement of lipid-lowering treatment targets in the DIAbetes and LifEstyle Cohort Twente: systemic assessment of pharmacological and nutritional factors. Nutr Diabetes. 2018;8:24.
Tapp H, Phillips SE, Waxman D, Alexander M, Brown R, Hall M. Multidisciplinary team approach to improved chronic care management for diabetic patients in an urban safety net ambulatory care clinic. J Am Board of Fam Med. 2012;25(2):245.
Chwastiak LA, Jackson SL, Russo J, DeKeyser P, Kiefer M, Belyeu B, et al. A collaborative care team to integrate behavioral health care and treatment of poorly-controlled type 2 diabetes in an urban safety net primary care clinic. Gen Hosp Psychiatry. 2017;44:10–5.
De Berardis G, Pellegrini F, Franciosi M, Belfiglio M, Di Nardo B, Greenfield S, et al. Quality of care and outcomes in type 2 diabetic patients: A comparison between general practice and diabetes clinics. Diabetes Care. 2004;27(2):398–406.
Nasir B, Abd Aziz A, Abdullah M, Norhayati N. Waist height ratio compared to body mass index and waist circumference in relation to glycemic control in Malay type 2 diabetes mellitus patients, Hospital Universiti Sains Malaysia. Int J Collab Res Inter Med Public Health. 2012;4:406.
Duckworth W, Abraira C, Moritz T, Reda D, Emanuele N, Reaven PD, et al. Glucose control and vascular complications in veterans with type 2 diabetes. N Engl J Med. 2009;360(2):129–39.
Maghbooli Z, Pasalar P, Keshtkar A, Farzadfar F, Larijani B. Predictive factors of diabetic complications: A possible link between family history of diabetes and diabetic retinopathy. J Diabetes Metab Disord. 2014;13(1):55.
Mamo Y, Bekele F, Nigussie T, Zewudie A. Determinants of poor glycemic control among adult patients with type 2 diabetes mellitus in Jimma University Medical Center, Jimma zone, south west Ethiopia: A case control study. BMC Endocr Disord. 2019;19(1):91.
Gray N, Picone G, Sloan F, Yashkin A. Relation between BMI and diabetes mellitus and its complications among US older adults. South Med J. 2015;108(1):29–36.
Yang G-R, Yuan M-X, Wan G, Zhang X-L, Fu H-J, Yuan S-Y, et al. Neck circumference and waist circumference associated with cardiovascular events in type 2 diabetes (Beijing Community Diabetes Study 23). Sci Rep. 2021;11(1):9491.
Saneei P, Shahdadian F, Moradi S, Ghavami A, Mohammadi H, Rouhani MH. Neck circumference in relation to glycemic parameters: a systematic review and meta-analysis of observational studies. Diabetol Metab Syndr. 2019;11(1):50.
Zhang Y, Wu H, Xu Y, Qin H, Lan C, Wang W. The correlation between neck circumference and risk factors in patients with hypertension: What matters. Medicine. 2020;99(47):e22998.
Cho NH, Oh TJ, Kim KM, Choi SH, Lee JH, Park KS, et al. Neck circumference and incidence of diabetes mellitus over 10 years in the Korean Genome and Epidemiology Study (KoGES). Sci Rep. 2015;5:18565.
Khan HA, Sobki SH, Khan SA. Association between glycaemic control and serum lipids profile in type 2 diabetic patients: HbA1c predicts dyslipidaemia. Clin Exp Med. 2007;7(1):24–9.
Hussain A, Ali I, Ijaz M, Rahim A. Correlation between hemoglobin A1c and serum lipid profile in Afghani patients with type 2 diabetes: Hemoglobin A1c prognosticates dyslipidemia. Ther Adv Endocrinol Metab. 2017;8(4):51–7.
Christman AL, Selvin E, Margolis DJ, Lazarus GS, Garza LA. Hemoglobin A1c predicts healing rate in diabetic wounds. J Invest Dermatol. 2011;131(10):2121–7.
Mohammad H, Girish T, Sarvajeet K, Surulivelrajan M. Correlation of glycosylated hemoglobin levels with fasting and posprandial glucose in south indian type 2 diabetic patients. Inter J Pharm Pharm Sci. 2016;8(8):285–8.
Acknowledgements
Authors are very grateful for the study participants, data collections and supervision.
Funding
This work was supported by Research Division, Faculty of Medicine Siriraj Hospital, Mahidol University (IO) R016132013. The funder had no role in the design of the study and collection, analysis, and interpretation of the data and in manuscript preparation.
Author information
Authors and Affiliations
Contributions
THP and TAP involved in conceiving the idea, study design, and data analysis. TAP, THP, NC involved in interpretation and managers the overall progress of the study. TAP and THP wrote the manuscript. CB performed on-site data collection. TAP, BP, PM made comments and suggestions. AS performed statistical analyses. TAP and KM reviewed the first and subsequent versions of the manuscript. Finally, all read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by Siriraj Institutional Review Board (095/2560 (EC1)). All methods in this study were carried out in accordance with relevant guidelines and regulations. We obtained written informed consent from all subjects before data collection.
Consent for publication
Not Applicable.
Competing interests
All authors declared that there was no competing interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Puangpet, T., Pongkunakorn, T., Chulkarat, N. et al. Control and complications of diabetes in urban primary care units in Thailand: a cross-sectional study. BMC Prim. Care 23, 212 (2022). https://doi.org/10.1186/s12875-022-01823-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12875-022-01823-7