Abstract
Objective
The objective of the study was to analyze surgical site infection (SSI) frequency with different duration antibiotic courses to establish the minimum necessary duration.
Methods
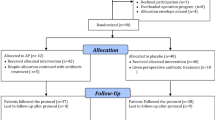
This is an observational study of prospective surveillance of 287 consecutive patients (mean age 67.8 years) operated on for acute cholecystitis of grade II severity in the first 72 h. Postoperative antibiotics had been withdrawn before diagnosis of any infection as an inclusion criterion. Patients were classified into three groups, according to therapy duration: group 1 (0–4 days, n = 45, 15.7 %); group 2 (5–7 days, n = 75, 26.1 %); and group 3 (>7 days, n = 167, 58.2 %). A multivariable analysis of risk infection was performed.
Results
Overall SSI frequency in groups 1, 2, and 3 was 2.2, 10.7, and 9 %, respectively. Risk analysis showed an increase in both crude and adjusted relative risks of overall infection in group 2 (crude relative risk (RR): 4.80 (0.62–37.13); adjusted RR, 2.03 (0.20–20.91)) and in group 3 (crude RR, 4.04 (0.55–29.79); adjusted RR, 2.35 (0.28–20.05)) by comparison with group 1, although without statistical significance. As a result, treatment lasting 4 days or less was not associated with overall surgical site infection incidence higher than longer treatment.
Conclusion
Antibiotic treatment over 4 days after early cholecystectomy provides no advantage in decreasing surgical site infection incidence.
Similar content being viewed by others
Introduction
Antibiotic treatment of variable duration after cholecystectomy for acute cholecystitis is a routine practice in many surgical departments, according to the recommendations of clinical guidelines,1,2 especially when there are clinical data of infection and in patients with high risk of septic complications.3 The necessary duration after emergency cholecystectomy is, however, not known. It is possible that after septic source removal, short courses of antibiotics are as useful as longer treatments, at least for flemonous or gangrenous cholecystitis, without empyema, perforation, or pericholecystic abscess. Continuation of antibiotics beyond the necessary time could, not only not provide benefits, but become deleterious. This practice could contribute to increasing bacterial resistance rates due to a higher exposure to the drugs or elimination of nonpathogenic flora. The patient exposed to drugs for a longer time has increased risk to adverse reactions. Finally, the costs are higher.
Only a few papers addressed the duration of antibiotic therapy. One article only gives a description of clinical practices concerning duration of antibiotics and surgeons' preferences, without any definitive conclusion or recommendation.4 In a randomized trial of cefamandole use in patients with acute cholecystitis who underwent open cholecystectomy, a short course (three doses) was as effective as a 7-day course.5 In another old study,6 longer treatment did not show any reduction in septic complications. The scanty recommendations available come from clinical guidelines,7,8 not particularly focused on acute cholecystitis with the exception of the Tokyo guidelines.1,2
The aim of this study is to analyze the frequency and risk of surgical site infections (SSI) with antibiotic courses of different duration after early cholecystectomy in order to establish the minimum necessary duration.
Methods
This is an observational study of prospective surveillance of 287 patients operated on for acute cholecystitis in the first 72 h after symptom onset (early cholecystectomy). The data comprise consecutive patients between 2005 and 2011 who met the following inclusion criteria: (1) fulfilling the Tokyo diagnostic criteria9 and histological confirmation of acute cholecystitis; (2) grade II severity according to the Tokyo classification;9 (3) surveillance at least for the first 30 postoperative days, excluding those who died; (4) no biliary leaks (defined as bilirubin concentration in the drain fluid at least three times the serum bilirubin concentration on or after postoperative day 3 or as the need for radiologic or operative intervention resulting from biliary collections or bile peritonitis); as a result, patients with bile in the drainage or percutaneously drained abscess with bile were excluded; (5) patients in whom a SSI had not been diagnosed before antibiotic withdrawal. This criterion excluded patients in whom prolongation of treatment could have been due to infection. Therefore, those patients having any SSI before antibiotic withdrawal was excluded. As a result, the study group consisted of 287 patients, 113 women (39.4 %) and 174 men (60.6 %), with a mean age of 67.8 years (SD, 13.8).
Diagnosis and severity assessment was done according to the Tokyo guidelines.9 Moderate acute cholecystitis (grade II) were those associated with any one of the following conditions: leukocyte count over 18,000/ml, palpable tender mass in the upper right abdominal quadrant, duration of complaints >72 h, marked local inflammation (biliary peritonitis, pericholecystic abscess, hepatic abscess, gangrenous cholecystitis, emphysematous cholecystitis), with no dysfunction in any one organ/system (Table 1).
Anesthetic surgical risk was assessed by the American Society of Anesthesiologists (ASA) classification.10
The surgical approach was laparoscopic in 212 cases (73.9 %) and open in 75 (26.1 %), according to the experience and criteria of the attending surgeon. Samples for culture from either or both the gallbladder content and peritoneal exudate were taken in most cases.
The clinical diagnosis of acute cholecystitis was histologically confirmed in every case.
Empiric antibiotic therapy was initiated before cholecystectomy and continued in the postoperative period for a variable duration. Antibiotic choice was done following the Tokyo and Infectious Diseases Society of America guidelines1,7 which addressed the therapy by the years of the study. The used drugs showed activity against the expected germs and adequate biliary penetration: piperacillin–tazobactam in 161 patients (56.1 %), amoxicillin–clavulanate in 60 (20.9 %), and others in 59 (20.6 %). The criterion for selection and duration of the treatment was personal to the attending surgeon. Patients were arbitrarily classified into three groups, according to therapy duration: group 1 (0–4 days, n = 45, 15.7 %); group 2 (5–7 days, n = 75, 26.1 %); and group 3 (>7 days, n = 167, 58.2 %). The definition of the groups was arbitrary since there is no previous data on this ground in the literature. However, the first limit (group 1) coincides with the minimum of 4 days of treatment recommended by the Tokyo guidelines9 and the second limit (group 2) coincides with the maximum of 7 days.
Infection risk was assessed by the National Nosocomial Infections Surveillance (NNIS) score.11 Briefly, for cholecystectomy, the following factors added 1 point: surgery time over 120 min, contaminated or dirty operation, and ASA III or IV. The final score resulted from subtracting 1 point from the former addition in case of laparoscopic approach.
Overall, incisional and organ/space SSI were registered until at least 1 month after operation. SSI definitions were based on CDC/NHSN recommendations.12
To estimate homogeneity of distribution of the variables most frequently associated with surgical infection risk in the different study groups, pair comparison of such variables was performed (Table 2). Among others, data concerning age mean and proportion of ASA status, NNIS, or disease severity are shown. The significant differences found in several variables indicate that the groups are not directly comparable. As a result, a multivariable analysis was needed.
Statistical analysis was done using Chi square test for noncontinuous variables and Fisher's exact test when necessary. For multiple pair comparisons, Bonferroni's correction was used. For quantitative variables, variance analysis (ANOVA) was used, with Bonferroni's test to estimate variance homogeneity and Scheffé's test for post hoc comparisons.
Relative risks (RR) were calculated for the analysis of association between the variables and infection risk, with a 95 % confidence interval. Estimations of independent predictors of surgical infection and its adjusted RR were done by means of multivariate analysis with a model of multiple logistic regression.
Results
Age, ASA classification, NNIS score, and other clinical variables in the different groups are shown in Table 2. Significantly lower NNIS scores were found in group 1 than in groups 2 and 3.
Culture was available in 152 patients, which was negative in 54 (35.5 %) and positive in 98 (64.5 %). The most frequent isolates were: Escherichia coli alone (26 cases, 26.5 %) or in association with other bacteria (9 cases, 9.2 %), Streptococcus of several species (19 cases, 19.4 %), Enterococcus of several species (17 cases, 17.3 %), Clostridium perfringens (6 cases, 6.1 %) either alone or in association with aerobes, Citrobacter freundii (5 cases, 5.1 %), and Klebsiella oxytoca (5 cases, 5.1 %).
Overall morbidity rate was 16.4 %. There were nonsurgical complications (cardiac, pulmonary, renal) in 18 patients (6.3 %) and surgical (infectious, bleeding from abdomen or laparoscopic ports, incisional hernia) in 34 (11.9 %). There was no major complication concerning antibiotic therapy, not even a single case of Clostridium difficile infection—no patient was tested since none had suspicion.
Overall, incisional and organ/space SSI incidences are shown in Table 3. Infection risk factor multivariate analysis is shown in Table 4. Factors not associated with increased risk were gender, age, or diabetes. The NNIS score showed differences in the three study groups, with different SSI frequencies in the univariate analysis. However, it did not show any significant influence in the multivariate analysis. Also, patients operated through open or laparoscopic, but converted, approach had a higher infection risk, although not significant.
Risk analysis concerning treatment duration showed an increase in crude and adjusted relative risks of SSI infection in groups 2 and 3 by comparison with group 1, although without significance. This suggests that shorter treatments are at least as good as longer treatments.
Since not every patient had received the same antibiotic, we analyzed the NNIS score and found significant differences among those treated with amoxicillin–clavulanate (with lower NNIS scores) and piperacillin–tazobactam (with higher NNIS scores) (p = 0.0001). This can be in part explained by the choice of piperacillin–tazobactam in cases with more severe inflammatory findings.
Overall SSI was slightly higher, but not significantly, in the patients operated by open (12 %) rather than by laparoscopic approach (7.1 %). This difference seems due to a higher incisional infection (9.3 vs 3.8 %) (p = 0.06), since the organ/space SSI incidences were very similar (2.7 vs 3.3 %) (p = 0.6). In group 1, there were significantly more cases with laparoscopic approach (86.7 %) than in either group 2 (64 %) (p = 0.001) or group 3 (74.9 %) (p = 0.02), although this factor is included in the NNIS score.
We performed an additional analysis limited to patients having positive cultures. SSI incidences were 0 % in group 1, 16 % in group 2, and 12.7 % in group 3 (p = 0.24), thus suggesting again longer treatments were of no benefit.
Although all the patients had grade II acute cholecystitis, those having marked local inflammation features (gangrenous cholecystitis, pericholecystic abscess, hepatic abscess, biliary peritonitis, emphysematous cholecystitis) could have higher risk of infection. Therefore, we analyzed separately these “high risk patients” (208 cases, 72.5 %) and those not showing these features (79 cases, 27.5 %). The SSI frequencies were 6.7 and 11.7 %, respectively, with no statistical significant difference (p = 0.2).
As a result, our data suggest that antibiotic treatment over 4 days after cholecystectomy for acute cholecystitis does not reduce SSI incidences.
Discussion
Antibiotic therapy after cholecystectomy for acute cholecystitis is a usual practice in most surgical departments, at least in moderate or severe cases. The aims are to complete the elimination of infecting microorganisms, to decrease the likelihood of infectious complications, and to shorten the time until resolution of clinical signs of infection. However, the postoperative need of antibiotics is controversial, at least in less severe cases, as is the duration of the therapy. The guidelines of the Infectious Diseases Society of America recommend antibiotic treatment if infection is suspected on the basis of laboratory and clinical findings (more than 12,500 leukocytes/mm3 or a temperature of more than 38.5 °C) and radiographic findings (i.e. air in the gallbladder or gallbladder wall).8 The Tokyo guidelines also recommend that antimicrobial agents should be administered to patients diagnosed with acute cholecystitis.2,9 On the other hand, the need for antibiotics has even been challenged, at least in mild cases not treated by surgery.13
Only a few studies have focused on duration of postoperative therapy, probably because the dominant surgical attitude was, for many years, to perform elective cholecystectomy after clinical resolution of the acute cholecystitis episode. Nowadays, however, there is enough clinical evidence to support urgent cholecystectomy (in the first 3–5 days), since postoperative morbidity is not increased, and with the advantages of avoiding treatment failures, new acute episodes and shortening in-hospital stays and thus, decreasing costs.2,14,15 One study gives only a description of the postoperative treatment duration and of surgeons' preference.4 In a randomized trial of the use of cefamandole in patients with acute cholecystitis who underwent open cholecystectomy, a short course (three doses) was as effective as a 7-day course.5 An old study from 1975 did not find any difference in septic complications between patients with and without antibiotic treatment,6 although the available drugs at that moment were different from those currently available. Another study suggests giving antibiotics after cholecystectomy if the patient has two or more of the following risk factors: temperature higher than 37.7 °C, total serum bilirubin greater than 8.6 μmol/L, and leukocyte count higher than 14,000/L.16 The Spanish Consensus on antibiotic therapy of intra-abdominal infections gives only generic recommendations of limiting the antibiotics to 3 days provided the septic source has been removed and there are no risk factors of bad evolution, although there is no specific reference to the case of acute cholecystitis.7 Also, the Infectious Diseases Society of America guidelines8 give generic recommendations of continuing until resolution of infection clinical signs occurs, including normalization of temperature and leukocyte count and return of gastrointestinal function with antibiotic maintenance, in case of persistent or recurrent clinical evidence of intra-abdominal infection after 5–7 days of therapy. Concerning duration, the 2013 Tokyo guidelines recommend 4–7 treatment days after source control in grade II and III cases; if there is Gram-positive bacteremia, therapy must be prolonged a minimum of 2 weeks; in grade I cases, treatment can be discontinued 24 h after cholecystectomy.2
The present study has been performed in a sample of patients with acute cholecystitis of grade II severity treated by cholecystectomy in the first 3 days. We analyzed the cases with postoperative antibiotic therapy which was withdrawn before any clinical evidence of SSI had arisen. Following this selection criterion, those patients with antibiotic therapy prolonged due to infection were excluded. The first finding is that most patients received a prolonged antibiotic therapy without obvious reasons. The most important finding has been, however, that the prolongation of postoperative antibiotic treatment for more than 4 days, without clinical signs of infection, did not reduce SSI incidences. This suggests, therefore, that there is no benefit of continuing postoperative treatment beyond 4 days. These findings coincide with those of Lau et al.5
A higher risk of SSI has been reported in patients with positive bile cultures.17 In our series, however, no significant difference in the positivity of cultures (from bile or peritoneal exudates) among the treatment groups was found, and therefore, they did not influence the results.
Our study has some limitations. Although the series size is considerable and the data were prospectively collected, the design was not strictly prospective, since the objectives were not established before patient recruitment. Also, the lower mean age and the higher proportion of laparoscopic cholecystectomy in group 1 could have influenced the lower although not significant overall SSI. Both factors could have biased the interpretation of the results. Another confounding factor was the heterogeneity in the drugs used, although most patients were treated with amoxicillin–clavulanate or piperacillin–tazobactam and the analysis was performed stratifying by drug type. Again, a treatment beyond 4 days conferred no advantage in reducing SSI incidence. The main disturbing factor was the NNIS score, associated with higher SSI infection frequency in the univariate analysis and showing lower scores in group 1. Because of the heterogeneity in the variables among the study groups, a multivariate analysis was performed. Risk analysis showed that the SSI risk in group 1 was even lower than in groups 2 or 3. This allows us to conclude that treatments lasting no more than 4 days are probably as good as treatments beyond 4 days.
According to the current bacterial resistance patterns and recommendations, many patients had needed carbapenems to empirically treat extended-spectrum beta-lactamase-producing bacteria,2,7 but this was not the case for the years of the study.
We conclude, despite the relative limitations of this study, that SSI incidence does not decrease with antibiotic treatment beyond 4 days. As a result, if there is no clinical evidence or high suspicion of infection, antibiotics ought not to be continued beyond the fourth postoperative day, at least for nonsevere cases. It is even possible that no postoperative antibiotics are needed in mild cases, something which future studies might address.
References
Yoshida M, Takada T, Kawarada Y, Tanaka A, Nimura Y, Gomi H, Hirota M, Miura F, Wada K, Mayumi T, Solomkin JS, Strasberg S, Pitt HA, Belghti J, de Santibanes E, Fan ST, Chen MF, Belli G, Hilvano SC, Kim SW, Ker CG. Antimicrobial therapy for acute cholecystitis: Tokyo Guidelines. J Hepatobiliary Pancreat Surg 2007; 14: 83–90
Gomi A, Solomkin JS, Takada T, Strasberg SM, Pitt HA, Yoshida M, Kusachi S, Mayumi T, Miura F, Kiriyama S, Yokoe M, Kimura Y, Higuchi R, Windsor JA, Dervenis C, Liau KH, Kim MH. TG13 antimicrobial therapy for acute cholangitis and cholecystitis. J Hepatobiliary Pancreat Sci 2013; 20: 60–70
Strasberg SM. Acute Calculous Cholecystitis. N Eng J Med 2008; 358: 2804–11
Kanafani, ZA, Khalifé N, Kanj SS, Araj GF, Khalifeh M, Sharara AI. Antibiotic use in acute cholecystitis: practice patterns in the absence of evidence-based guidelines. J Infect 2005; 51: 128–134
Lau WY, Yuen WK, Chu KW, Chong KK, Li AK. Systemic antibiotic regimens for acute cholecystitis treated by early cholecystectomy. Aust N Z J Surg 1990; 60: 539–43
Kune GA, Burdon JG. Are antibiotics necessary in acute cholecystitis? Med J Aust 1975; 2: 627–30
Guirao X, Arias J, Badía JM, García-Rodríguez JA, Mensa J, Álvarez-Lerma F, Borges M, Barberán J, Maseda M, Salavert M, Llinares P, Gobernadó M, García Rey C. Recomendaciones en el tratamiento antibiótico empírico de la infección intraabdominal. Cir Esp 2010; 87: 63–81
Solomkin JS, Mazuski JE, Baron EJ, Sawyer RG, Nathens AB, DiPiro JT et al. Guidelines for the selection of anti-infective agents for complicated intra-abdominal infections. Clin Infect Dis 2003; 37: 997–1005
Yokoe M, Takada T, Strasberg SM, Solomkin JS, Mayumi T, Gomi H, Pitt HA, Garden OJ, Kiriyama S, Gouma DJ, Garden OJ, Büchler MW, Kiriyama S, Hata J, Gabata T, Yoshida M, Miura F, Okamoto K, Tsuyuguchi T, Itoi T, Yamashita Y, Dervenis C, Chan ACW, Lau WY, Supe AN, Belli G, Hilvano SC, Liau KH, Kim MH, Kim SH, Ker CG. TG13 diagnostic criteria and severity grading of acute cholecystitis (with videos). J Hepatobiliary Pancreat Sci 2013; 20: 35–46
Little JP. Consistency of ASA grading. Anaesthesia 1995; 50: 658–659
Culver DH, Horan TC, Gaynes RP, Martone WJ, Jarvis WR, Emori TG, Banerjee SN, Edwuards JR, Tolson JS, Henderson TS, Hughes JM, National Nosocomial Infections surveillance system. Surgical wound infection rates by wound class, operative procedure, and patient risk index. Am J Med 1991; 91 (Suppl 2): 152S–157S
Horan TC, Andrus M, Dudeck MA. CDC/NHSN surveillance definition of health care–associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control 2008; 36: 309–332
Mazeh H, Mizrahi I, Dior U, Simanovsky N, Shapiro M, Freund HR, Eid A. Role of antibiotics in mild acute calculous cholecystitis: A prospective randomized controlled trial. World J Surg 2012: 36: 1750–9
Papi C, Catarci M, D'Ambrosio L, Gili L, Koch M, Grassi GB, Capurso L. Timing of cholecystectomy for acute calculous cholecystitis: A meta-analysis. Am J Gastroenterol 2004; 99: 147–155
Gurusamy KS, Samraj K. Early versus delayed laparoscopic cholecystectomy for acute cholecystitis. Cochrane Database Syst Rev. 2006 Oct 18; (4):CD005440.
Thompson JE, Bennion RS, Doty JE, Muller EL, Pitt HA. Predictive factors for bactibilia in acute cholecystitis. Arch Surg 1990; 125: 261–264
Galili O, Eldar S Jr, Matter I, Madi H, Brodsky A, Galis I, Eldar S Sr. The effect of bactibilia on the course and outcome of laparoscopic cholecystectomy. Eur J Clin Microbiol Infect Dis. 2008; 27: 797–803
Author information
Authors and Affiliations
Corresponding author
Additional information
The study was approved by the local Committee of ethics in Clinical Research.
Rights and permissions
About this article
Cite this article
Rodríguez-Sanjuán, J.C., Casella, G., Antolín, F. et al. How Long Is Antibiotic Therapy Necessary After Urgent Cholecystectomy for Acute Cholecystitis?. J Gastrointest Surg 17, 1947–1952 (2013). https://doi.org/10.1007/s11605-013-2321-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-013-2321-3