Abstract
Integrated positron emission tomography/computed tomography (PET/CT) using 2-[18F]fluoro-2-deoxy-d-glucose (18F-FDG) has emerged as a powerful tool for combined metabolic and anatomic evaluation in clinical oncologic imaging. This review discusses the utility of 18F-FDG PET/CT as a tool for managing patients with lung cancer. We discuss different patient management stages, including diagnosis, initial staging, therapy planning, early treatment response assessment, re-staging, and prognosis.
Similar content being viewed by others
Introduction
Lung cancer is the most common cancer; despite major advances in prevention and treatment, it remains the leading cause of cancer-related death worldwide [1]. Over 85 % of cases are of non-small cell lung cancer (NSCLC), while the remainder are small cell lung cancers (SCLCs) [2]. Accurate staging is essential for treatment planning and determining patient prognosis. NSCLC staging is performed according to the tumor, node, metastasis (TNM) classification, which was updated in 2009 by the International Union Against Cancer and American Joint Committee on Cancer to include proposals from the International Association for the Study of Lung Cancer [3].
Integrated positron emission tomography/computed tomography (PET/CT) with 2-[18F]fluoro-2-deoxy-d-glucose (18F-FDG) is a powerful tool for combined metabolic and anatomic evaluation of cancer. In the clinical setting, 18F-FDG PET/CT has improved diagnostic accuracy and influenced the initial staging, treatment optimization, therapy response monitoring, restaging, and prognostication of lung cancer. Here, we review the current and future roles of 18F-FDG PET/CT in lung cancer management, and discuss its usefulness and limitations.
Diagnosis
A solitary pulmonary nodule (SPN) is defined as a single spherical or oval lesion (<3 cm in diameter) without accompanying atelectasis or adenopathy. 18F-FDG PET/CT has 97 % sensitivity and 85 % specificity for diagnosing SPN malignancy [4]. In a meta-analysis of 8511 nodules including 70 18F-FDG PET and PET/CT studies [5], the pooled sensitivity for the detection of SPN malignancy was 0.89 [95 % confidence interval (CI), 0.86–0.91] and the pooled specificity was 0.75 (95 % CI, 0.71–0.79). Although the specificity of 18F-FDG PET is superior to that of CT, it is far from ideal. Dual time-point 18F-FDG PET by acquisition of delayed imaging has been proposed as a means to improve diagnostic specificity for SPNs [6], although its usefulness remains controversial [7]. A meta-analysis [8] demonstrated that the sensitivity and specificity of dual time-point 18F-FDG PET/CT were 85 and 77 %, respectively, which are similar to those for single time-point 18F-FDG PET/CT. Kawano et al. [9] has compared the maximum standardized uptake value (SUVmax) of primary lung cancer between free-breathing PET/CT and deep-inspiration breath-hold PET/CT, and demonstrated that the SUVmax of free-breathing PET/CT should not be considered to be accurate, especially in the lower lung area and for small pulmonary lesions, whereas breath-hold PET/CT presented a complete match between CT and PET, leading to the expectation that it provides precise SUVmax values.
There are several potential pitfalls for SPN assessment using 18F-FDG PET. Inflammatory conditions such as pneumonia, aspergillosis, tuberculosis, active sarcoidosis, and granulomatosis with polyangiitis can result in high metabolic activity due to increased granulocyte and/or macrophage activity [10]. Current PET/CT cameras have limited spatial resolution (5–6 mm), leading to false-negative results and suggesting that a critical mass of metabolically active malignant cells must be present for accurate detection. Therefore, 18F-FDG PET could result in a false-negative diagnosis for lesions <1 cm and those with low metabolic activity and low cell density (e.g., carcinoid tumors, adenocarcinoma in situ, and well-differentiated adenocarcinoma) [11, 12].
Staging
Initial disease staging in newly diagnosed NSCLC can correctly differentiate patients with potentially curable disease from those indicated for palliative therapy. 18F-FDG PET/CT has greater staging accuracy than either of the modalities alone because of the improved detection of additional lymph node involvement or distant metastasis [13, 14].
T staging
Primary lung tumor extent is mostly evaluated using thoracic CT, which, in cases of superior sulcus extension, thoracic wall invasion, or heart or large vessel involvement, is supplemented by magnetic resonance imaging (MRI). The major contribution of 18F-FDG PET/CT is accurate tumor delineation from surrounding post-obstructive atelectasis (Fig. 1), which is important for therapy planning; 18F-FDG PET/CT can also be useful for detecting chest wall invasion [15].
A 68-year-old man with non-small-cell lung cancer with post-obstructive atelectasis and multiple lymph node metastases at initial staging. a Contrast-enhanced computed tomography (CT) shows a mass and atelectatic lung extending from the superior right hilum, without a clear distinction between the soft-tissue mass and the consolidated lung, as well as a 12 × 13 mm swollen subcarinal lymph node (#7) (arrow), suggesting the presence of spreading nodal cancer. b Positron emission tomography/CT using 2-[18F]fluoro-2-deoxy-d-glucose (18F-FDG) shows intense 18F-FDG uptake in the primary tumor (curved arrow), with no uptake in obstructive atelectasis of the right upper lobe. The swollen subcarinal lymph node shows intense FDG uptake (arrow), confirming nodal metastasis
Locoregional lymph node staging (N staging)
The most commonly used technique for N staging of patients with lung cancer is CT, due to its easy accessibility, relatively low cost, and noninvasiveness. Mediastinal and hilar lymph nodes with a short axis of >10 mm are classified as enlarged. However, lymph node size alone has poor specificity for detecting metastatic involvement because enlargement also occurs under benign inflammatory conditions. Moreover, small-sized nodes might contain tumoral deposits [16]. A critical advantage of 18F-FDG PET/CT over CT is the detection of neoplastic mediastinal adenopathies <1 cm in size (Fig. 2); the superiority of 18F-FDG PET [17] and PET/CT [18, 19] over CT for mediastinal staging is well established. A meta-analysis of 39 studies showed that the median sensitivity and specificity of CT were 61 and 79 %, respectively, whereas those for 18F-FDG PET were 85 and 90 % [17]. Furthermore, in a meta-analysis including 20 studies involving 3028 patients with NSCLC, 18F-FDG PET/CT had a pooled sensitivity of 0.72 (95 % CI, 0.68–0.75) and a specificity of 0.90 (95 % CI, 0.88–0.91) [18]. With respect to nodal size, the sensitivity of 18F-FDG PET/CT in detecting malignant involvement was 32.4 % in nodes <10 mm and 85.3 % in nodes ≥10 mm [19].
A 65-year-old man with ipsilateral mediastinal and hilar nodal metastases arising from non-small cell lung cancer. a Contrast-enhanced computed tomography (CT) shows a 3.2 × 2.5 cm solid mass with enhancement in the right upper lobe, suggesting lung cancer. A small 7 × 8 mm lymph node is seen at the anterior mediastinum (#3a, arrow), suggesting the absence of spreading nodal cancer. b Contrast-enhanced CT shows one 10 × 12 mm swollen lymph node at the right hilar area (#12, arrow), suggesting the presence of spreading nodal cancer. c Positron emission tomography (PET)/CT using 2-[18F]fluoro-2-deoxy-d-glucose (18F-FDG) shows intense 18F-FDG uptakes corresponding to the lung mass and the anterior mediastinal node (arrow), confirming lung cancer and ipsilateral mediastinal nodal metastasis. d 18F-FDG PET/CT shows intense 18F-FDG uptake corresponding to the right hilar node (arrow), confirming the ipsilateral hilar nodal metastasis. The patient underwent right upper lobe resection and lymph node dissection; examination of the histopathological specimen revealed extensive lymph node involvement in the two nodes (pT2N2)
False-negative results due to micrometastasis occur because of the limited spatial resolution of PET, whereas false-positive results were reported in the setting of endemic granulomatous disease. Evidence suggests that 18F-FDG PET findings should not replace histological confirmation. A recent multicenter study indicated that 18F-FDG PET/CT had high NPV (91 %) and specificity (83 %) but a low positive predictive value (PPV) (29 %) [20]. Similar findings were confirmed in a prospective trial where the mediastinal staging of 149 patients by 18F-FDG PET/CT was confirmed histopathologically; overall sensitivity, specificity, PPV, and NPV were 70, 94, 64, and 95 %, respectively [21]. The low PPV indicated that invasive mediastinal sampling should be conducted when lymph node involvement is suspected and when making curative surgical decisions because false positivity could be a confounding factor, especially in those with granulomatous diseases [22]. In contrast, the high NPV of 18F-FDG PET/CT suggested that invasive sampling of mediastinal lymph nodes could be safely omitted. False-negative findings may be seen in cases of low tumoral burden in metastatic lymph nodes (“minimal N2”), where a reasonable prognosis after surgical resection is expected [23]. However, in the presence of a centrally located tumor or hilar lymphadenopathy, mediastinoscopy should be conducted because limitations in spatial resolution combined with highly active hilar lymph nodes or tumoral lesions might mask the metabolic activity of nearby lymph nodes.
In summary, 18F-FDG PET/CT is more accurate for N staging than CT; however, the spatial resolution of PET is not sufficient to detect early lymph node involvement and micrometastases, and 18F-FDG PET/CT cannot replace histological staging.
Extrathoracic staging (M staging)
Identification of distant metastases has major implications for management and prognosis. Approximately 18–36 % of patients with newly diagnosed NSCLC have distant metastases at presentation [24]. The adrenal glands, bones, liver, and brain are the most common metastatic sites.
Whole-body 18F-FDG PET/CT is more accurate than conventional imaging for detection of metastatic foci (Fig. 3) [13, 14]. A meta-analysis involving 6 studies with 659 patients [25] revealed that the pooled sensitivity and specificity of 18F-FDG PET/CT for detecting distant metastasis from NSCLC were 0.87 (95 % CI, 0.55–0.98) and 0.96 (95 % CI, 0.93–0.98), respectively.
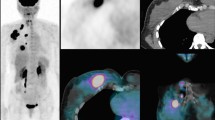
A 64-year-old woman with non-small cell lung cancer with liver, adrenal gland, lung, and bone metastases at initial staging. a Maximum intensity projection of an image acquired by positron emission tomography (PET) using 2-[18F]fluoro-2-deoxy-d-glucose (18F-FDG) shows multiple abnormal intense uptakes in both lungs as well as the liver, right adrenal gland, and spine. b 18F-FDG PET/computed tomography (CT) shows abnormal FDG uptakes corresponding to left lung cancer and metastasis to the vertebra (arrow). c 18F-FDG PET/CT shows abnormal FDG uptake corresponding to liver metastasis (arrow). d 18F-FDG PET/CT shows abnormal FDG uptake corresponding to adrenal gland metastasis (arrow). e 18F-FDG PET/CT and f CT alone show abnormal FDG uptakes corresponding to multiple osteolytic changes in the spine (arrows), confirming multiple bone metastases
18F-FDG PET/CT has high sensitivity (97 %) and specificity (86 %) for metastatic adrenal disease in NSCLC [26], which eliminates the need for invasive sampling [27]. However, the partial volume effect must be considered when evaluating small lesions (<1 cm). False positives have been reported; therefore, histopathological confirmation is warranted when treatment decisions are based on an isolated adrenal gland finding.
In patients with lung cancer, whole-body 18F-FDG PET/CT for detecting bone metastases showed sensitivity and specificity that were superior to bone scintigraphy [28, 29]. A systematic review that included 6 articles (1746 patients in total) demonstrated that the pooled sensitivity and specificity of 18F-FDG PET/CT and PET were 0.93 (95 % CI, 0.88–0.96) and 0.95 (95 % CI, 0.91–0.98), respectively, whereas those for bone scintigraphy were 0.87 (95 % CI, 0.79–0.93) and 0.82 (95 % CI, 0.62–0.92), respectively [29].
18F-FDG PET/CT can be used as a reliable and noninvasive method for the detection of pleural dissemination (Fig. 4), but the tiny lesion could not even be detected by 18F-FDG PET/CT (Fig. 5). Erasmus et al. [30] reported that the sensitivity, specificity, positive predictive value, negative predictive value, and accuracy of pretreatment 18F-FDG PET/CT for detecting pleural metastases in 25 patients with NSCLC were 95, 67, 95, 67, and 92 %, respectively.
A 76-year-old woman who underwent right lower lobe resection due to non-small cell lung cancer 6 months prior showing multiple recurrent lesions consisting of local recurrence, mediastinal nodal metastasis, pleural dissemination, liver metastases, and bone metastases at restaging. a Maximum intensity projection of an image acquired by positron emission tomography (PET) using 2-[18F]fluoro-2-deoxy-d-glucose (18F-FDG) shows multiple abnormal intense uptakes in the right lung, mediastinum, right pleura, liver, and spine. b 18F-FDG PET/computed tomography (CT) and c CT alone show abnormal FDG uptake corresponding to local recurrence at the postoperative stump (arrow). It is difficult to diagnose this local recurrence by CT alone. d 18F-FDG PET/CT and e CT show abnormal FDG uptakes corresponding to the right pleural dissemination (arrows). It is difficult to diagnose pleural dissemination by CT alone. f 18F-FDG PET/CT shows abnormal FDG uptakes corresponding to liver metastases (arrows) and pedicle bony metastasis (curved arrow). It is difficult to diagnose this bone metastasis based on CT alone
A 79-year-old man with non-small cell lung cancer and mediastinal and hilar nodal metastases at therapy response evaluation. a Pretreatment maximum intensity projection of an image acquired by positron emission tomography (PET) using 2-[18F]fluoro-2-deoxy-d-glucose (18F-FDG) shows multiple abnormal intense uptakes in the left lung, hilum, and mediastinum. b Pretreatment 18F-FDG PET/computed tomography (CT) and c CT show moderate FDG uptakes corresponding to one left 2.3 × 2.3 cm solid mass (SUVmax 8.38), one 9 × 9 mm swollen hilar lymph node (SUVmax 4.70, arrow), and one 14 × 16 mm swollen mediastinal lymph node (SUVmax 5.52, curved arrow), suggesting lung cancer with nodal metastases (cT1N2). Curative surgery was attempted in this patient but it was not accomplished because of tiny pleural dissemination which could not be detected by 18F-FDG PET/CT. The patient underwent chemotherapy. d MIP by 18F-FDG PET at 3 months after starting gefitinib treatment shows faint uptakes in the left lung, hilum, and mediastinum. e 18F-FDG PET/CT and f CT at 3 months after starting gefitinib treatment show mildly decreased or a virtual absence of 18F-FDG uptake corresponding to the primary tumor (18 × 21 mm, SUVmax 1.71), the metastatic hilar node (8 mm, SUVmax 2.15, arrow), and the metastatic mediastinal node (10 × 17 mm, SUVmax 1.70, curved arrow)
High glucose uptake by gray matter and small lesion size limit the diagnostic power of 18F-FDG PET, so MRI is the preferred modality for detecting brain metastases [31].
18F-FDG PET/CT could unveil metastases that otherwise escape detection (e.g., soft-tissue lesions, small supraclavicular lymph nodes, and retroperitoneal lymph nodes). Previous studies found that 18F-FDG PET and PET/CT resulted in a staging change in 27–62 % of patients with NSCLC and altered patient management in 19–52 % [13, 14, 32, 33]. Hicks et al. showed that 18F-FDG PET staging had a major impact on the treatment plan in 54 of 153 (35 %) patients with newly diagnosed NSCLC [32]. Treatment was changed from curative to palliative in 34 patients and from palliative to curative in 6. In 14 patients, the treatment modality was altered without a change in treatment intent. In summary, 18F-FDG PET/CT is a highly sensitive and specific modality for detecting distant metastases of lung cancer (excluding brain metastases).
Radiotherapy planning
Radiotherapy is the treatment of choice for curative intent in patients with early-stage (stage I–II) NSCLC who are contraindicated for surgery. The majority of 18F-FDG PET studies are performed for preoperative staging; however, the metabolic information provided by the procedure may facilitate radiotherapy planning. Accurate identification of locoregional tumor load could determine the type of therapeutic intervention, the tumor volume targeted by radiotherapy, and (consequently) the toxicity. For classical radiotherapy planning, CT is used to delineate the target tumor volume. Disadvantages associated with CT include poor delineation of some tumors because of accompanying atelectasis and limited accuracy for detecting lymphatic involvement. With its improved accuracy, 18F-FDG PET/CT-based radiotherapy planning could improve delineation and avoid unnecessary irradiation to adjacent nontumoral tissues. Furthermore, in patients with NSCLC, 18F-FDG PET could lead to significant treatment strategy modifications and radiotherapy planning alterations [34]. Studies concerning the impact of 18F-FDG PET/CT on radiotherapy planning have demonstrated that the tumoral and nodal contours could be altered in >50 % of patients with probable improved tumoral coverage [35]. Additionally, 18F-FDG PET/CT-derived tumor volumes were smaller compared to those derived by CT alone; this facilitates radiation dose escalation while respecting normal tissue constraints [36]. In a study of 21 patients with clinical CT stage N2–3 tumors, the gross tumor volume significantly decreased from 13.7 ± 3.8 cm3 on the CT scan to 9.8 ± 4.0 cm3 on the 18F-FDG PET/CT scan. In another study, the incorporation of 18F-FDG PET/CT data for radiotherapy planning significantly reduced the estimated doses to the esophagus and lungs [37]. Moreover, interobserver variability in delineating tumor volumes was diminished when 18F-FDG PET was used for planning [38]. In addition to its enhanced clinical value in radiotherapy planning, the use of 18F-FDG PET/CT altered the therapeutic strategy in 40 % of patients with NSCLC, which resulted in an overall cost reduction for treatment in this group [39].
The use of respiratory gating in integrated 18F-FDG PET/CT has been evaluated recently, especially its clinical impact on planning target volumes for radiation therapy. Preliminary results in patients with lung cancer showed that respiratory-gated 18F-FDG PET/CT, which tailors the target volume to lesion motion, can affect the size and shape of target volumes, leading to improved delineation [40].
Therapy response evaluation
In oncological settings, early assessment of therapeutic response enables treatment alteration in cases of nonresponse. Response assessment using conventional imaging depends mostly on changes in tumor volume. Therapy-induced tumor size reduction is measured by radiologic techniques, such as CT, according to the World Health Organization and the response evaluation criteria in solid tumors (RECIST). However, compared to conventional structural imaging modalities, evaluation of metabolic activity using 18F-FDG PET provides valuable response information at an earlier time point [41]. In 73 NSCLC patients evaluated using 18F-FDG PET and enhanced CT before and at a median interval of 70 days after radiotherapy and chemoradiotherapy, 18F-FDG PET metabolic and CT morphologic response categories were identical in 40 % of patients, with significantly more patients (n = 34) showing a complete metabolic response (CMR) than showing a complete response on CT (n = 10) [42]. Furthermore, response assessment with morphologic imaging techniques has limitations in distinguishing necrotic tumors or fibrotic scars from residual tumor tissue. From this point of view, PET can be used to characterize tissues based on their biochemical and biological features (Fig. 5) [41].
Response evaluation using 18F-FDG PET in patients who underwent chemotherapy or chemoradiotherapy has been evaluated extensively [43–46]. Studies comparing 18F-FDG PET and non-enhanced CT suggested that 18F-FDG PET was a better predictor of response [47]. Changes in tumor metabolic activity on 18F-FDG PET scans were significantly greater in histologically confirmed chemotherapy responders compared to nonresponders [43]. Furthermore, the change in SUVmax after chemotherapy/chemoradiotherapy showed a near-linear relationship with the percentage of nonviable tumor cells in the resected tumors [44]. The outcomes of patients who demonstrated a CMR were superior to those of the patients who did not [41–46].
The utility of 18F-FDG PET for therapy response assessment and outcome prediction after neoadjuvant radiochemotherapy was evaluated in 70 patients with stage III NSCLC [45]. That study demonstrated that the sensitivity, specificity, and accuracy of FDG-PET to detect residual viable primary tumor were 95, 80, and 91 %, respectively. Additionally, patients with a CMR (as determined by qualitative criteria) or an 80 % reduction in the SUVmax had significantly longer survival compared to those with a partial metabolic response (PMR). Progressive disease on 18F-FDG PET was significantly associated with an unfavorable outcome. Similarly, Mac Manus et al. [42] demonstrated that patients showing a CMR survived longer than those showing a PMR; in turn, survival in the latter group was superior to that of nonresponders (stable or progressive metabolic disease). By contrast, a recent study involving 89 patients from two consecutive phase II clinical trials of chemotherapy for NSCLC found that the response on 18F-FDG PET did not predict outcome, whereas RECIST responses were associated with overall survival (OS) [47].
Total lesion glycolysis (TLG) is calculated as the product of metabolic tumor volume (MTV) and the mean SUV of all voxels. MTV is defined as the volume of the delineated tumor on PET. In patients with locally advanced NSCLC treated with concomitant chemoradiotherapy, TLG has emerged as a predictor of progression-free survival (PFS) [48] and OS [49]. Yossi et al. [49] showed that a TLG decrease of >15 % after 30 Gy (up to a total dose of 66–70 Gy in 2-Gy fractions) was associated with improved OS and PFS.
One advantage of 18F-FDG PET is the early detection of biological changes caused by decreased glucose metabolism in nonvital tissue, which facilitates earlier detection of responders and nonresponders as measured by 18F-FDG retention [41, 50]. A significant reduction of 18F-FDG uptake after one chemotherapy cycle was noted with various therapeutic regimens, and changes in uptake correlated with both response according to RECIST1.1 and survival [51–53]. Treatment can be adjusted on an individual basis according to tumor chemosensitivity as assessed by 18F-FDG PET. Measurement methods of 18F-FDG uptake are diverse, and timing with respect to anticancer therapy and thresholds used to define responses are variable. Therefore, further studies are required before definite conclusions can be drawn on using 18F-FDG PET as a tool for therapy response monitoring.
In addition to its role in response evaluation of neoadjuvant chemotherapy in NSCLC, 18F-FDG PET/CT has shown promise in monitoring response to biological agents such as epidermal growth factor receptor tyrosine kinase inhibitors (Fig. 5) [54–57]. A review of 18F-FDG PET/CT use in targeted treatment for NSCLC suggested that response monitoring could be performed 1–2 weeks after treatment initiation, and that tumors showing a substantial decrease in metabolic activity would probably benefit from continued treatment. Refining FDG-PET response criteria might assist in clinical decision-making on the continuation or discontinuation of targeted treatment [57].
In summary, 18F-FDG PET/CT is emerging as a promising tool for early monitoring of the effectiveness of chemotherapy or chemoradiotherapy in lung cancer. However, there are substantial disparities with respect to response assessment, so standardization remains a requirement.
Monitoring of recurrence (restaging)
NSCLC has a high recurrence rate, even in patients treated with curative intent. Therefore, a method of selecting patients who have an increased risk of recurrence for further adjuvant therapy would be highly beneficial. Imaging plays a central role in recurrence detection, but chest radiograph and CT scan interpretation can be challenging because of posttreatment anatomical changes such as bronchi distortion, lung parenchyma infiltration, and fibrosis. In these settings, 18F-FDG PET/CT is a powerful adjunct for patient follow-up after therapy (Fig. 4). After radiotherapy, local tumor recurrence usually occurs within 2 years, but may create a diagnostic challenge because of the presence of mass-like radiation-induced fibrosis [58]. 18F-FDG PET can distinguish recurrent tumors from fibrosis, providing that sufficient time (i.e., 3 months) has elapsed since treatment to eliminate the risk of false positivity associated with inflammatory changes [59]. In 62 NSCLC patients with suspected postsurgical recurrence, 18F-FDG PET had a sensitivity and specificity of 93 and 89 %, respectively, for relapse detection [60].
Distant metastases are the most prevalent form of NSCLC recurrence. Several groups have demonstrated the usefulness of NSCLC restaging using 18F-FDG PET/CT (Fig. 4) [61, 62]. 18F-FDG PET/CT showed high diagnostic performance for recurrence detection in 241 consecutive patients who underwent potentially curative surgery for NSCLC [61]. Because of the high NPV for recurrence detection, it was proposed that further conventional imaging (except for brain MRI) could be omitted in cases where 18F-FDG PET/CT did not detect recurrence. In a recent meta-analysis that included 13 studies (1035 patients in total) on lung cancer recurrence, the pooled sensitivity and specificity were 0.90 (95 % CI, 0.84–0.95) and 0.90 (0.87–0.93), respectively, for 18F-FDG PET/CT; and 0.78 (0.71–0.84) and 0.80 (0.75–0.84), respectively, for conventional imaging techniques [62]. Despite extensive studies showing excellent results for NSCLC restaging using 18F-FDG PET/CT, the most recent American College of Chest Physicians evidence-based guidelines do not recommend 18F-FDG PET/CT for routine surveillance after curative-intent treatment [63].
Prognostication
Primary lesion metabolic activity is associated with indicators of aggressive biologic behavior such as the tumor doubling time and degree of differentiation [64]. Therefore, 18F-FDG PET metabolic information might provide additional prognostic information based on the biological behavior of the tumor. Although most studies have reported that a high SUVmax was associated with a poorer prognosis [65–69], others found that it was not an independent predictor for OS [70, 71]. In a study of 162 consecutive patients with stage I–IIIb NSCLC, the presence of low tumoral SUVmax was associated with increased 2-year disease-free survival rates for both early (I–II) and late (IIIa–IIIb) stage patients [65]. In a study that included 487 patients, SUVmax was an independent prognostic determinant along with the TNM stage, but it did not contribute to the prognostic value of pathologic staging [67]. A recent meta-analysis (1805 patients in total) including 18 studies demonstrated that both pre-radiotherapy and post-radiotherapy primary tumor SUVmax could predict the outcomes of patients with NSCLC who underwent radiotherapy [68].
In contrast, Agarwal et al. studied 363 patients with stage I and II NSCLC and demonstrated that the preoperative SUVmax was not an independent prognosticator for OS [70]. Similar results were noted in a retrospective analysis of 214 patients with stage IIIA, IIIB, and IV NSCLC [71]. SUVmax is not recommended for risk stratification in the 7th edition of the American Joint Committee on Cancer staging manual [3], and is not considered a prognostic biomarker in the National Comprehensive Cancer Network guidelines (version 3, 2014) [72].
Recent studies suggest that, compared to SUVmax, metabolic indices such as MTV and TLG might have better prognostic implications related to whole-body and primary tumor burdens [73–78]. A recent meta-analysis (1581 patients in total) including 13 studies demonstrated that patients with a high MTV had worse prognosis for adverse events [hazard ratio (HR), 2.71; 95 % CI, 1.82–4.02] and death (HR, 2.31; 95 % CI, 1.54–3.47) compared to those with a low MTV [78]. Additionally, patients with a high TLG had worse prognosis with respect to adverse events (HR, 2.35; 95 % CI, 1.91–2.89) and death (HR, 2.43; 95 % CI, 1.89–3.11) [78].
In addition to its prognostic value in pre-treatment evaluation, a recent prospective trial in patients with stage III NSCLC indicated that high tumor SUV after treatment was associated with poor prognosis [79]. A retrospective study of surveillance 18F-FDG PET/CT during follow-up >6 months after treatment showed that 18F-FDG PET was a prognosticator of OS [80]. Patients without recurrence according to 18F-FDG PET/CT had a median survival time (MST) of 81.6 months compared with an MST of 32.9 months in those with suspected recurrence. Zhang et al. demonstrated that postsurgical whole-body metabolic tumor burden and tumor SUVmax were related to OS in patients with NSCLC, independent of age, sex, TNM restaging, and postsurgical therapy [81].
In summary, 18F-FDG PET/CT, including SUVmax, MTV, and TLG, might have prognostic value in patients with lung cancer, but further clarification studies are warranted.
SCLC
SCLC accounts for 15 % of lung cancers and is characterized by a rapid doubling time and aggressive clinical behavior, with a high prevalence of disseminated disease at diagnosis [2]. Although TNM staging is applied occasionally, the simplified dichotomous classification method of limited stage (LS) and extensive stage (ES) is used for SCLC staging. The standard therapies are concurrent chemoradiotherapy for patients with good performance status and LS disease, and palliative chemotherapy for those with ES disease. Despite initial chemosensitivity, overall prognosis is poor due to relapses. Given the difference in treatment strategies, accurate staging of SCLC is crucial. However, data concerning the use of 18F-FDG PET/CT for SCLC staging [25, 28, 29, 82–87], radiotherapy planning [82, 83], therapy response evaluation [88–90], and prognosis [89–94] are limited.
In a recent meta-analysis encompassing 12 papers and 369 patients, the pooled sensitivity and specificity of 18F-FDG PET or PET/CT for the detection of extensive disease in SCLC were 0.98 (95 % CI 0.94–0.99) and 0.98 (95 % CI 0.95–0.99) [86]. The impact of 18F-FDG PET on stage classification of newly diagnosed SCLC has been investigated in several studies which suggested that 18F-FDG PET facilitated modifications of stage and clinical management in 12–26 % of cases [82–86]. Studies indicated that the incorporation of 18F-FDG PET/CT data during initial staging led to changes in radiation fields in 37 % of patients [82]. High mean SUVmax values in pretreatment 18F-FDG PET/CT scans were associated with poorer OS and PFS in both LS and ES SCLC patients [91]. Whole-body MTV of 18F-FDG was of prognostic value in SCLC, and incorporation of metabolic data during TNM staging has been proposed to improve prognostic information [92]. Moreover, changes in MTV after radiotherapy correlated with survival in patients with LS SCLC [93].
Conclusion
18F-FDG PET/CT permits the combined metabolic and morphological assessment of tumors, with significant improvements in diagnostic accuracy and considerable impact on patient management, initial staging, therapy planning, early treatment response assessment, re-staging, and prognostication of lung cancer.
Further analyses to refine 18F-FDG PET/CT response criteria, the standardization of 18F-FDG PET/CT timing for chemotherapy or chemoradiotherapy response evaluation, the development of new PET cameras with higher spatial resolution, and the design of new radiotracers other than 18F-FDG are required.
References
DeSantis CE, Lin CC, Mariotto AB, Siegel RL, Stein KD, Kramer JL, et al. Cancer treatment and survivorship statistics, 2014. CA Cancer J Clin. 2014;64:252–71.
Rodriguez E, Lilenbaum RC. Small cell lung cancer: past, present, and future. Curr Oncol Rep. 2010;12:327–34.
Detterbeck FC, Boffa DJ, Tanoue LT. The new lung cancer staging system. Chest. 2009;136:260–71.
Kim SK, Allen-Auerbach M, Goldin J, Fueger BJ, Dahlbom M, Brown M, et al. Accuracy of PET/CT in characterization of solitary pulmonary lesions. J Nucl Med. 2007;48:214–20.
Deppen SA, Blume JD, Kensinger CD, Morgan AM, Aldrich MC, Massion PP, et al. Accuracy of FDG-PET to diagnose lung cancer in areas with infectious lung disease: a meta-analysis. JAMA. 2014;312:1227–36.
Zhuang H, Pourdehnad M, Lambright ES, Yamamoto AJ, Lanuti M, Li P, et al. Dual time point 18F-FDG PET imaging for differentiating malignant from inflammatory processes. J Nucl Med. 2001;42:1412–7.
Shinozaki T, Utano K, Fujii H, Utano Y, Sasaki T, Kijima S, et al. Routine use of dual time 18F-FDG PET for staging of preoperative lung cancer: does it affect clinical management? Jpn J Radiol. 2014;32:476–81.
Barger RL Jr, Nandalur KR. Diagnostic performance of dual-time 18F-FDG PET in the diagnosis of pulmonary nodules: a meta-analysis. Acad Radiol. 2012;19:153–8.
Kawano T, Ohtake E, Inoue T. Deep-inspiration breath-hold PET/CT of lung cancer: maximum standardized uptake value analysis of 108 patients. J Nucl Med. 2008;49:1223–31.
Bakheet SM, Saleem M, Powe J, Al-Amro A, Larsson SG, Mahassin Z. F-18 fluorodeoxyglucose chest uptake in lung inflammation and infection. Clin Nucl Med. 2000;25:273–8.
Erasmus JJ, McAdams HP, Patz EF Jr, Coleman RE, Ahuja V, Goodman PC. Evaluation of primary pulmonary carcinoid tumors using FDG PET. AJR Am J Roentgenol. 1998;170:1369–73.
Iwano S, Ito S, Tsuchiya K, Kato K, Naganawa S. What causes false-negative PET findings for solid-type lung cancer? Lung Cancer. 2013;79:132–6.
Shim SS, Lee KS, Kim BT, Chung MJ, Lee EJ, Han J, et al. Non-small cell lung cancer: prospective comparison of integrated FDG PET/CT and CT alone for preoperative staging. Radiology. 2005;236:1011–9.
De Wever W, Ceyssens S, Mortelmans L, Stroobants S, Marchal G, Bogaert J, et al. Additional value of PET-CT in the staging of lung cancer: comparison with CT alone, PET alone and visual correlation of PET and CT. Eur Radiol. 2007;17:23–32.
Kligerman S, Digumarthy S. Staging of non-small cell lung cancer using integrated PET/CT. AJR Am J Roentgenol. 2009;193:1203–11.
Gross BH, Glazer GM, Orringer MB, Spizarny DL, Flint A. Bronchogenic carcinoma metastatic to normal-sized lymph nodes: frequency and significance. Radiology. 1988;166:71–4.
Gould MK, Kuschner WG, Rydzak CE, Maclean CC, Demas AN, Shigemitsu H, et al. Test performance of positron emission tomography and computed tomography for mediastinal staging in patients with non-small-cell lung cancer: a meta-analysis. Ann Intern Med. 2003;139:879–92.
Zhao L, He ZY, Zhong XN, Cui ML. 18FDG-PET/CT for detection of mediastinal nodal metastasis in non-small cell lung cancer: a meta-analysis. Surg Oncol. 2012;21:230–6.
Lv YL, Yuan DM, Wang K, Miao XH, Qian Q, Wei SZ, et al. Diagnostic performance of integrated positron emission tomography/computed tomography for mediastinal lymph node staging in non-small cell lung cancer: a bivariate systematic review and meta-analysis. J Thorac Oncol. 2011;6:1350–8.
Li X, Zhang H, Xing L, Xie P, Zhang L, Xu X, et al. Mediastinal lymph nodes staging by 18F-FDG PET/CT for early stage non-small cell lung cancer: a multicenter study. Radiother Oncol. 2012;102:246–50.
Darling GE, Maziak DE, Inculet RI, Gulenchyn KY, Driedger AA, Ung YC, et al. Positron emission tomography-computed tomography compared with invasive mediastinal staging in non-small cell lung cancer: results of mediastinal staging in the early lung positron emission tomography trial. J Thorac Oncol. 2011;6:1367–72.
Silvestri GA, Gonzalez AV, Jantz MA, Margolis ML, Gould MK, Tanoue LT, et al. Methods for staging non-small cell lung cancer: diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2013;143:e211S–50S.
Sahiner I, Vural GU. Positron emission tomography/computerized tomography in lung cancer. Quant Imaging Med Surg. 2014;4:195–206.
Quint LE. Staging non-small cell lung cancer. Cancer Imaging. 2007;7:148–59.
Li J, Xu W, Kong F, Sun X, Zuo X. Meta-analysis: accuracy of 18FDG PET-CT for distant metastasis staging in lung cancer patients. Surg Oncol. 2013;22:151–5.
Brady MJ, Thomas J, Wong TZ, Franklin KM, Ho LM, Paulson EK. Adrenal nodules at FDG PET/CT in patients known to have or suspected of having lung cancer: a proposal for an efficient diagnostic algorithm. Radiology. 2009;250:523–30.
Marom EM, McAdams HP, Erasmus JJ, Goodman PC, Culhane DK, Coleman RE, et al. Staging non-small cell lung cancer with whole-body PET. Radiology. 1999;212:803–9.
Qu X, Huang X, Yan W, Wu L, Dai K. A meta-analysis of 18FDG-PET-CT, 18FDG-PET, MRI and bone scintigraphy for diagnosis of bone metastases in patients with lung cancer. Eur J Radiol. 2012;81:1007–15.
Chang MC, Chen JH, Liang JA, Lin CC, Yang KT, Cheng KY, et al. Meta-analysis: comparison of F-18 fluorodeoxyglucose-positron emission tomography and bone scintigraphy in the detection of bone metastasis in patients with lung cancer. Acad Radiol. 2012;19:349–57.
Erasmus JJ, McAdams HP, Rossi SE, Goodman PC, Coleman RE, Patz EF. FDG PET of pleural effusions in patients with non-small cell lung cancer. AJR Am J Roentgenol. 2000;175:245–9.
Yi CA, Shin KM, Lee KS, Kim BT, Kim H, Kwon OJ, et al. Non-small cell lung cancer staging: efficacy comparison of integrated PET/CT versus 3.0-T whole-body MR imaging. Radiology. 2008;248:632–42.
Hicks RJ, Kalff V, MacManus MP, Ware RE, Hogg A, McKenzie AF, et al. 18F-FDG PET provides high-impact and powerful prognostic stratification in staging newly diagnosed non-small cell lung cancer. J Nucl Med. 2001;42:1596–604.
Hoekstra CJ, Stroobants SG, Hoekstra OS, Vansteenkiste J, Biesma B, Schramel FJ, et al. The value of [18F]fluoro-2-deoxy-d-glucose positron emission tomography in the selection of patients with stage IIIA-N2 non-small cell lung cancer for combined modality treatment. Lung Cancer. 2003;39:151–7.
Pommier P, Touboul E, Chabaud S, Dussart S, Le Pechoux C, Giammarile F, et al. Impact of 18F-FDG PET on treatment strategy and 3D radiotherapy planning in non-small cell lung cancer: a prospective multicenter study. AJR Am J Roentgenol. 2010;195:350–5.
Bradley J, Bae K, Choi N, Forster K, Siegel BA, Brunetti J, et al. A phase II comparative study of gross tumor volume definition with or without PET/CT fusion in dosimetric planning for non-small cell lung cancer (NSCLC): primary analysis of Radiation Therapy Oncology Group (RTOG) 0515. Int J Radiat Oncol Biol Phys. 2012;82:435–41.
Bradley J, Thorstad WL, Mutic S, Miller TR, Dehdashti F, Siegel BA, et al. Impact of FDG-PET on radiation therapy volume delineation in non-small-cell lung cancer. Int J Radiat Oncol Biol Phys. 2004;59:78–86.
van Der Wel A, Nijsten S, Hochstenbag M, Lamers R, Boersma L, Wanders R, et al. Increased therapeutic ratio by 18FDG-PET CT planning in patients with clinical CT stage N2-N3M0 non-small-cell lung cancer: a modeling study. Int J Radiat Oncol Biol Phys. 2005;61:649–55.
Nestle U, Walter K, Schmidt S, Licht N, Nieder C, Motaref B, et al. 18F-deoxyglucose positron emission tomography (FDG-PET) for the planning of radiotherapy in lung cancer: high impact in patients with atelectasis. Int J Radiat Oncol Biol Phys. 1999;44:593–7.
Remonnay R, Morelle M, Pommier P, Giammarile F, Carrère MO. Assessing short-term effects and costs at an early stage of innovation: the use of positron emission tomography on radiotherapy treatment decision making. Int J Technol Assess Health Care. 2008;24:212–20.
Guerra L, Meregalli S, Zorz A, Niespolo R, De Ponti E, Elisei F, et al. Comparative evaluation of CT-based and respiratory-gated PET/CT-based planning target volume (PTV) in the definition of radiation treatment planning in lung cancer: preliminary results. Eur J Nucl Med Mol Imaging. 2014;41:702–10.
Hicks RJ. Role of 18F-FDG PET in assessment of response in non-small cell lung cancer. J Nucl Med. 2009;50:31S–42S.
Mac Manus MP, Hicks RJ, Matthews JP, McKenzie A, Rischin D, Salminen EK, et al. Positron emission tomography is superior to computed tomography scanning for response-assessment after radical radiotherapy or chemoradiotherapy in patients with non-small-cell lung cancer. J Clin Oncol. 2003;21:1285–92.
Yamamoto Y, Nishiyama Y, Monden T, Sasakawa Y, Ohkawa M, Gotoh M, et al. Correlation of FDG-PET findings with histopathology in the assessment of response to induction chemoradiotherapy in non-small cell lung cancer. Eur J Nucl Med Mol Imaging. 2006;33:140–7.
Cerfolio RJ, Bryant AS, Winokur TS, Ohja B, Bartolucci AA. Repeat FDG-PET after neoadjuvant therapy is a predictor of pathologic response in patients with non-small cell lung cancer. Ann Thorac Surg. 2004;78:1903–9.
Eschmann SM, Friedel G, Paulsen F, Reimold M, Hehr T, Budach W, et al. 18F-FDG PET for assessment of therapy response and preoperative re-evaluation after neoadjuvant radio-chemotherapy in stage III non-small cell lung cancer. Eur J Nucl Med Mol Imaging. 2007;34:463–71.
Decoster L, Schallier D, Everaert H, Nieboer K, Meysman M, Neyns B, et al. Complete metabolic tumour response, assessed by 18-fluorodeoxyglucose positron emission tomography (18FDG-PET), after induction chemotherapy predicts a favourable outcome in patients with locally advanced non-small cell lung cancer (NSCLC). Lung Cancer. 2008;62:55–61.
Tanvetyanon T, Eikman EA, Sommers E, Robinson L, Boulware D, Bepler G. Computed tomography response, but not positron emission tomography scan response, predicts survival after neoadjuvant chemotherapy for resectable non-small-cell lung cancer. J Clin Oncol. 2008;26:4610–6.
Usmanij EA, de Geus-Oei LF, Troost EG, Peters-Bax L, van der Heijden EH, Kaanders JH, et al. 18F-FDG PET early response evaluation of locally advanced non-small cell lung cancer treated with concomitant chemoradiotherapy. J Nucl Med. 2013;54:1528–34.
Yossi S, Krhili S, Muratet JP, Septans AL, Campion L, Denis F. Early assessment of metabolic response by 18F-FDG PET during concomitant radiochemotherapy of non-small cell lung carcinoma is associated with survival: a retrospective single-center study. Clin Nucl Med. 2015;40:e215–21.
Skoura E, Datseris IE, Platis I, Oikonomopoulos G, Syrigos KN. Role of positron emission tomography in the early prediction of response to chemotherapy in patients with non-small-cell lung cancer. Clin Lung Cancer. 2012;13:181–7.
van Elmpt W, Ollers M, Dingemans AM, Lambin P, De Ruysscher D. Response assessment using 18F-FDG PET early in the course of radiotherapy correlates with survival in advanced-stage non-small cell lung cancer. J Nucl Med. 2012;53:1514–20.
Nahmias C, Hanna WT, Wahl LM, Long MJ, Hubner KF, Townsend DW. Time course of early response to chemotherapy in non-small cell lung cancer patients with 18F-FDG PET/CT. J Nucl Med. 2007;5:744–51.
Lee DH, Kim SK, Lee HY, Lee SY, Park SH, Kim HY, et al. Early prediction of response to first-line therapy using integrated 18F-FDG PET/CT for patients with advanced/metastatic non-small cell lung cancer. J Thorac Oncol. 2009;7:816–21.
O’Brien ME, Myerson JS, Coward JI, Puglisi M, Trani L, Wotherspoon A, et al. A phase II study of 18F-fluorodeoxyglucose PET-CT in non-small cell lung cancer patients receiving erlotinib (Tarceva); objective and symptomatic responses at 6 and 12 weeks. Eur J Cancer. 2012;48:68–74.
Takahashi R, Hirata H, Tachibana I, Shimosegawa E, Inoue A, Nagatomo I, et al. Early [18F]fluorodeoxyglucose positron emission tomography at two days of gefitinib treatment predicts clinical outcome in patients with adenocarcinoma of the lung. Clin Cancer Res. 2012;18:220–8.
Bengtsson T, Hicks RJ, Peterson A, Port RE. 18F-FDG PET as a surrogate biomarker in non-small cell lung cancer treated with erlotinib: newly identified lesions are more informative than standardized uptake value. J Nucl Med. 2012;53:530–7.
van Gool MH, Aukema TS, Hartemink KJ, Valdés Olmos RA, van Tinteren H, Klomp HM. FDG-PET/CT response evaluation during EGFR-TKI treatment in patients with NSCLC. World J Radiol. 2014;6:392–8.
Koenig TR, Munden RF, Erasmus JJ, Sabloff BS, Gladish GW, Komaki R, et al. Radiation injury of the lung after three-dimensional conformal radiation therapy. AJR Am J Roentgenol. 2002;178:1383–8.
Larici AR, del Ciello A, Maggi F, Santoro SI, Meduri B, Valentini V, et al. Lung abnormalities at multimodality imaging after radiation therapy for non-small cell lung cancer. Radiographics. 2011;31:771–89.
Hellwig D, Gröschel A, Graeter TP, Hellwig AP, Nestle U, Schäfers HJ, et al. Diagnostic performance and prognostic impact of FDG-PET in suspected recurrence of surgically treated non-small cell lung cancer. Eur J Nucl Med Mol Imaging. 2006;33:13–21.
Kanzaki R, Higashiyama M, Maeda J, Okami J, Hosoki T, Hasegawa Y, et al. Clinical value of F18-fluorodeoxyglucose positron emission tomography-computed tomography in patients with non-small cell lung cancer after potentially curative surgery: experience with 241 patients. Interact Cardiovasc Thorac Surg. 2010;10:1009–14.
He YQ, Gong HL, Deng YF, Li WM. Diagnostic efficacy of PET and PET/CT for recurrent lung cancer: a meta-analysis. Acta Radiol. 2014;55:309–17.
Colt HG, Murgu SD, Korst RJ, Slatore CG, Unger M, Quadrelli S. Follow-up and surveillance of the patient with lung cancer after curative-intent therapy: diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2013;143(5 suppl):e437S–54S.
Yamamoto Y, Nishiyama Y, Ishikawa S, Nakano J, Chang SS, Bandoh S, et al. Correlation of 18F-FLT and 18F-FDG uptake on PET with Ki-67 immunohistochemistry in non-small cell lung cancer. Eur J Nucl Med Mol Imaging. 2007;34:1610–6.
Sasaki R, Komaki R, Macapinlac H, Erasmus J, Allen P, Forster K, et al. [18F] fluorodeoxyglucose uptake by positron emission tomography predicts outcome of non-small-cell lung cancer. J Clin Oncol. 2005;23:1136–43.
Davies A, Tan C, Paschalides C, Barrington SF, O’Doherty M, Utley M, et al. FDG-PET maximum standardised uptake value is associated with variation in survival: analysis of 498 lung cancer patients. Lung Cancer. 2007;55:75–8.
Downey RJ, Akhurst T, Gonen M, Park B, Rusch V. Fluorine-18 fluorodeoxyglucose positron emission tomographic maximal standardized uptake value predicts survival independent of clinical but not pathologic TNM staging of resected non-small cell lung cancer. J Thorac Cardiovasc Surg. 2007;133:1419–27.
Na F, Wang J, Li C, Deng L, Xue J, Lu Y. Primary tumor standardized uptake value measured on F18-fluorodeoxyglucose positron emission tomography is of prediction value for survival and local control in non-small-cell lung cancer receiving radiotherapy: meta-analysis. J Thorac Oncol. 2014;9:834–42.
Kwon W, Howard BA, Herndon JE, Patz EF Jr. FDG uptake on positron emission tomography correlates with survival and time to recurrence in patients with stage I non-small-cell lung cancer. J Thorac Oncol. 2015;10:897–902.
Agarwal M, Brahmanday G, Bajaj SK, Ravikrishnan KP, Wong CY. Revisiting the prognostic value of preoperative 18F-fluoro-2-deoxyglucose (18F-FDG) positron emission tomography (PET) in early-stage (I & II) non-small cell lung cancers (NSCLC). Eur J Nucl Med Mol Imaging. 2010;37:691–8.
Hoang JK, Hoagland LF, Coleman RE, Coan AD, Herndon JE 2nd, Patz EF Jr. Prognostic value of fluorine-18 fluorodeoxyglucose positron emission tomography imaging in patients with advanced-stage non-small-cell lung carcinoma. J Clin Oncol. 2008;26:1459–64.
National Comprehensive Cancer Network. Non-small cell lung cancer (version 3. 2014). http://www.nccn.org/professionals/physician_gls/pdf/nscl.pdf. Accessed 7 Feb 2016.
Chen HH, Chiu NT, Su WC, Guo HR, Lee BF. Prognostic value of whole-body total lesion glycolysis at pretreatment FDG PET/CT in non-small cell lung cancer. Radiology. 2012;264:559–66.
Zhang H, Wroblewski K, Liao S, Kampalath R, Penney BC, Zhang Y, et al. Prognostic value of metabolic tumor burden from 18F-FDG PET in surgical patients with non-small-cell lung cancer. Acad Radiol. 2013;20:32–40.
Hyun SH, Ahn HK, Kim H, Ahn MJ, Park K, Ahn YC, et al. Volume-based assessment by 18F-FDG PET/CT predicts survival in patients with stage III non-small-cell lung cancer. Eur J Nucl Med Mol Imaging. 2014;41:50–8.
Satoh Y, Onishi H, Nambu A, Araki T. Volume-based parameters measured by using FDG PET/CT in patients with stage I NSCLC treated with stereotactic body radiation therapy: prognostic value. Radiology. 2014;270:275–81.
Park SY, Cho A, Yu WS, Lee CY, Lee JG, Kim DJ, et al. Prognostic value of total lesion glycolysis by 18F-FDG PET/CT in surgically resected stage IA non-small cell lung cancer. J Nucl Med. 2015;56:45–9.
Im HJ, Pak K, Cheon GJ, Kang KW, Kim SJ, Kim IJ, et al. Prognostic value of volumetric parameters of 18F-FDG PET in non-small-cell lung cancer: a meta-analysis. Eur J Nucl Med Mol Imaging. 2015;42:241–51.
Machtay M, Duan F, Siegel BA, Snyder BS, Gorelick JJ, Reddin JS, et al. Prediction of survival by [18F]fluorodeoxyglucose positron emission tomography in patients with locally advanced non-small-cell lung cancer undergoing definitive chemoradiation therapy: results of the ACRIN 6668/RTOG 0235 trial. J Clin Oncol. 2013;31:3823–30.
Antoniou AJ, Marcus C, Tahari AK, Wahl RL, Subramaniam RM. Follow-up or surveillance 18F-FDG PET/CT and survival outcome in lung cancer patients. J Nucl Med. 2014;55:1062–8.
Zhang C, Liao C, Penney BC, Appelbaum DE, Simon CA, Pu Y. Relationship between overall survival of patients with non-small cell lung cancer and whole-body metabolic tumor burden seen on postsurgical fluorodeoxyglucose PET images. Radiology. 2015;275:862–9.
Kamel EM, Zwahlen D, Wyss MT, Stumpe KD, von Schulthess GK, Steinert HC. Whole-body 18F-FDG PET improves the management of patients with small cell lung cancer. J Nucl Med. 2003;44:1911–7.
Bradley JD, Dehdashti F, Mintun MA, Govindan R, Trinkaus K, Siegel BA. Positron emission tomography in limited-stage small-cell lung cancer: a prospective study. J Clin Oncol. 2004;22:3248–54.
Brink I, Schumacher T, Mix M, Ruhland S, Stoelben E, Digel W, et al. Impact of [18F]FDG-PET on the primary staging of small-cell lung cancer. Eur J Nucl Med Mol Imaging. 2004;31:1614–20.
Fischer BM, Mortensen J, Langer SW, Loft A, Berthelsen AK, Petersen BI, et al. A prospective study of PET/CT in initial staging of small-cell lung cancer: comparison with CT, bone scintigraphy and bone marrow analysis. Ann Oncol. 2007;18:338–45.
Azad A, Chionh F, Scott AM, Lee ST, Berlangieri SU, White S, et al. High impact of 18F-FDG PET on management and prognostic stratification of newly diagnosed small cell lung cancer. Mol Imaging Biol. 2010;12:433–51.
Lu YY, Chen JH, Liang JA, Chu S, Lin WY, Kao CH. 18F-FDG PET or PET/CT for detecting extensive disease in small-cell lung cancer: a systematic review and meta-analysis. Nucl Med Commun. 2014;35:697–703.
Yamamoto Y, Kameyama R, Murota M, Bandoh S, Ishii T, Nishiyama Y. Early assessment of therapeutic response using FDG PET in small cell lung cancer. Mol Imaging Biol. 2009;11:467–72.
Ziai D, Wagner T, El Badaoui A, Hitzel A, Woillard JB, Melloni B, et al. Therapy response evaluation with FDG-PET/CT in small cell lung cancer: a prognostic and comparison study of the PERCIST and EORTC criteria. Cancer Imaging. 2013;13:73–80.
van Loon J, Offermann C, Ollers M, van Elmpt W, Vegt E, Rahmy A, et al. Early CT and FDG-metabolic tumour volume changes show a significant correlation with survival in stage I–III small cell lung cancer: a hypothesis generating study. Radiother Oncol. 2011;99:172–5.
Lee YJ, Cho A, Cho BC, Yun M, Kim SK, Chang J, et al. High tumor metabolic activity as measured by fluorodeoxyglucose positron emission tomography is associated with poor prognosis in limited and extensive stage small-cell lung cancer. Clin Cancer Res. 2009;15:2426–32.
Oh JR, Seo JH, Chong A, Min JJ, Song HC, Kim YC, et al. Whole-body metabolic tumour volume of 18F-FDG PET/CT improves the prediction of prognosis in small cell lung cancer. Eur J Nucl Med Mol Imaging. 2012;39:925–35.
Shirvani SM, Komaki R, Heymach JV, Fossella FV, Chang JY. Positron emission tomography/computed tomography-guided intensity-modulated radiotherapy for limited-stage small-cell lung cancer. Int J Radiat Oncol Biol Phys. 2012;82:e91–7.
Kishimoto M, Iwano S, Ito S, Kato K, Ito R, Naganawa S. Prognostic evaluations of small size lung cancers by 18F-FDG PET/CT and thin-section CT. Lung Cancer. 2014;86:180–4.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
We declare no financial support or relationship that may pose a conflict of interest.
About this article
Cite this article
Kitajima, K., Doi, H., Kanda, T. et al. Present and future roles of FDG-PET/CT imaging in the management of lung cancer. Jpn J Radiol 34, 387–399 (2016). https://doi.org/10.1007/s11604-016-0546-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11604-016-0546-2