Abstract
Background
Fifth metacarpal fractures are common and comprise a significant proportion of traditional orthopaedic fracture clinic workload. We reviewed the functional outcome and the satisfaction of patients managed with a new protocol that promoted “self-care” and resulted in the discharge of most of these patients from the emergency department with no further follow-up.
Methods
A retrospective study was performed of patients discharged with a fifth metacarpal fracture between April 2012 to October 2012. A postal questionnaire was sent to each patient, followed by a telephone call. Patient-reported outcome measures (EQ-5D, QuickDASH) and patient satisfaction were assessed. Of the 167 patients eligible for the study, 5 were excluded. Of the remaining 162, 64 were uncontactable or declined to participate. The mean follow-up time was 21.6 months (SD 1.9, range 18.1 to 24.7).
Results
The median EQ-5D health index score was 0.87 (IQR 0.74 to 1.00), and the median QuickDASH score was 2.3 (IQR 0 to 6.8). Seventy-nine (80.6 %) patients were satisfied with the outcome of their injury, while 83 (84.9 %) reported being satisfied with the process. There was no difference between those with a fracture or those without a fracture in EQ-5D (p = 0.307) or QuickDASH (p = 0.820).
Conclusion
Fifth metacarpal fractures can be managed effectively through an Emergency Department protocol without any formal orthopaedic follow-up. This pathway lead to excellent patient-reported outcome measures and patient satisfaction. This protocol has reduced unnecessary hospital attendances for patients and increased the time available for clinicians to deal with more challenging injuries.
Similar content being viewed by others
Introduction
Fifth metacarpal fractures are an extremely common orthopaedic presentation that represents up to 20 % of all hand fractures [8]. Patients are able to tolerate a marked amount of volar angulation [13]. The natural history of this fracture is one of excellent functional recovery over 2–3 months [15, 17]. The optimal treatment of this fracture remains under considerable debate [1, 2, 13, 14, 17, 20, 21]. Management options include surgical intervention, immobilisation with or without closed reduction and functional bracing. There is a considerable evidence base to show conservative treatment with functional bracing leads to high patient satisfaction and good functional outcomes [4–7, 10, 11, 17, 18, 21, 22]. Patients have conventionally been recalled for early and medium term follow-up in orthopaedic clinics to assess fracture position and functional recovery. Our unit has introduced a management protocol that places emphasis on “self-care”. Fractures with rotational deformity are referred by the Emergency Department (ED) at the time of presentation. The remainder are provided with verbal and written information about the expected recovery period and are managed with simple “buddy strapping”. They are provided with access to a helpline to contact if they have any concerns or worsening symptoms. They are not routinely reviewed in a follow-up clinic, which reduces inconvenience for the patient through transport needs and time off work. It is also beneficial to the orthopaedic department as it allows greater time in clinic to focus on patients with more complex injuries.
The aim of this study was to perform a clinical audit of the patient satisfaction and outcome of fifth metacarpal fractures treated with this new protocol.
Materials and Methods
A retrospective review of all patients who presented to our linked Emergency Department (ED) and minor injuries unit (MIU) with a fifth metacarpal fracture between April 2012 and October 2012 was performed. This was an intention to treat study, and therefore, the inclusion criteria involved all patients diagnosed with an acute fifth metacarpal fracture by our Emergency Department and managed via the new pathway. This study identified a small proportion where this diagnosis was found to be wrong (false positive diagnosis). A radiologist or reporting radiographer reviewed all radiographs performed in the ED. There were no patients during the study period who were subsequently diagnosed with a fracture that had been initially missed (false negative). As the study was a retrospective audit of routine clinical outcomes of standard treatment using simple validated questionnaires; it was not subject to research ethics committee (REC) review. In the United Kingdom (UK), review by a REC is required for research within the scope of the UK Health Departments’ Governance Arrangements for Research Ethics Committees. Non-operative treatment of this fracture has broad support in the literature. There was no allocation, randomisation, or treatment concealment. This project fell under the scope of clinical audit as it sought to measure the satisfaction and outcome of this accepted treatment in our health system, against that described in the literature.
All patients in the study were assessed and treated by an emergency medicine doctor or emergency nurse practitioner (ENP). Anteroposterior (AP) and oblique radiographs of the hand were performed. In patients with more complex injuries, including intra-articular extension, dislocation, open injuries, significant rotational deformities, and polytrauma, the treating clinician could opt to either discuss with the local hand service or refer the patient to a virtual fracture clinic for further review. All other patients with a positive diagnosis were treated with functional bracing, using “neighbour strapping” to the adjacent digit. The patient was given an information leaflet and discharged with no follow-up (Appendix A). This leaflet provided patients with information regarding their diagnosis and natural history of the injury, advice for early mobilisation and a helpline contact number. All x-rays were formally reported by a radiologist within 24 h, and any discrepancies with the ED’s diagnosis were referred back to a senior clinician.
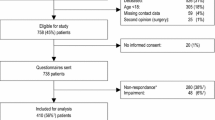
The patient cohort was collated from a search of the Emergency Department’s database EDIS (Emergency Department’s Information System, Omnis Software) that identified patients directly discharged from the Emergency Department with a fracture of the fifth metacarpal. This coding was made at the time of treatment by the relevant care provider. All radiographs were reviewed, verified, and classified by the senior author (LAR). They were classified into four subgroups: neck, shaft, base, and no fracture present. A satisfaction survey and patient-reported outcome measure questionnaires were administered at a minimum of 1 year following the injury. A postal questionnaire was sent to all patients. Those who did not reply were contacted by telephone. The overall response rate was 59 % (Fig. 1).
The initial study group included 167 patients. Ninety-eight (59 %) of patients responded to the questionnaire. Twenty-three (23.5 %) were female and 75 (76.5 %) were male. Twenty-one (21.4 %) were left-sided fractures and 77 (78.6 %) were right. There were 52 (53.1 %) neck fractures, 14 (14.3 %) shaft, 24 (24.5 %) base, and 8 (8.2 %) patients in whom no fracture was identified (Table 1). There was no difference between the study group and those lost to follow-up in terms of age (p = 0.903, MWU), gender (p = 0.092, MWU), or socioeconomic deprivation (p = 0.420, MWU) (Table 2). There was a small difference in loss to follow-up between injury type, with the “no fracture” group having the highest loss to follow-up rate (Table 2).
Satisfaction was rated by a 4-level Likert scale with the options: very satisfied, satisfied, dissatisfied, and very dissatisfied. Patients were also asked if [1] they were satisfied with the outcome of their injury [2], if they were satisfied with the process and information provided [3], if they had visited any other physician about this injury, and if so [4], what was the reason for the visit(s).
Patient-reported outcome measures were used to assess functional outcome. The QuickDASH and EQ-5D scores were used. The QuickDASH uses 11 items to measure physical function and symptoms in people with any or multiple musculoskeletal disorders of the upper limb [3]. The EQ5D is a standardised instrument for use as a measure of health outcome [16].
The satisfaction rates for each question were then analysed as simple proportions. When multiple proportions were compared, a χ 2 test was used to assess statistical significance. The data was checked for normality with histograms. This tended to be skewed; therefore, nonparametric tests (Mann–Whitney U [MWU]; Kruskal–Wallis [KW]) were used and medians with interquartile ranges were reported. The level of significance was set at 0.05.
Results
Seventy-nine (80.6 %) patients reported being very satisfied or satisfied with the outcome of their injury, while 83 (84.9 %) reported being satisfied with the new process (Table 3) (Fig. 2). Three (3.1 %) patients contacted the helpline. Twenty contacted their general practitioner, of which 11 were to obtain sick lines.
The median EQ-5D health index score was 0.87 (IQR 0.74 to 1.00) (Fig. 3), and the median QuickDASH score was 2.3 (IQR 0 to 6.8). There was no association between gender and EQ-5D (p = 0.515, MWU) or QuickDASH (p = 0.789, MWU). There was a significant correlation between age and EQ-5D (r = −0.38, p < 0.001) and QuickDASH (r = 0.313, p = 0.002). There was no association between fracture location and EQ-5D (p = 0.717, KW) or QuickDASH (p = 0.327, KW). There was no association between the Scottish Index of Multiple Deprivation (SIMD) and EQ-5D (p = 0.952, KW) or QuickDASH (p = 0.582, KW).
A binary logistic regression model was used to control for age, deprivation, gender and fracture type, and the interaction of the EQ-5D domains with satisfaction (Table 4). The only independent predictor of outcome was pain (OR 3.03, 95 % CI 1.72 to 5.31 for each point worse on pain score). There was no difference between those with a fracture or those without a fracture in EQ-5D (p = 0.307, MWU) or QuickDASH (p = 0.820, MWU).
Discussion
This study has demonstrated good satisfaction and functional outcomes by promoting self-care for patients with fifth metacarpal fractures. The literature supports conservative management for this patient group and rationalising follow-up for this injury [2]. This study is the first to report satisfaction scores and outcomes following early discharge from the ED with no routine face to face follow-up. These results demonstrate similar excellent patient satisfaction to other fractures that have been managed in the same way in the ED [9]. This study supports those findings and provides additional evidence of excellent functional outcomes when self-care is promoted, with follow-up for failure to progress. This study has demonstrated comparable patient satisfaction levels with other literature [1, 5] and comparable patient-reported outcome measures to traditional management approaches [2]. Normative data for the QuickDASH has recently been reported. This demonstrated mean = 10.9, SD = 15.3, median = 4.5, IQR 0 to 14.3, range 0–88.6. Furthermore, the median in males was lower at 2.27 (IQR 0 to 9.09), and similarly lower in the 19–35 age group at 2.27 (IQR 0 to 6.82). This normative data suggests that the population distribution demonstrates a left skew. Our data is in keeping with the population median, particularly in a young male population. The leaflet provides excellent information regarding the injury and the time frame for recovery, and the helpline gives a safety net and contact point if any patient’s recovery is performing below expectations.
Patients who sustain this fracture are known to be poorly compliant with follow-up with as little as 38 % of patients attending the final review [12]. A study identified the factors associated with non-attendance after a metacarpal fracture as being single or divorced, having no health insurance, being unemployed or disabled and having a fracture of the fifth metacarpal [20]. Our health system (National Health Service [UK]) does not require insurance; therefore, there would be less influence of this factor in our population. The identification of a lower attendance rate following a fifth metacarpal fracture, after controlling for other demographic factors, suggests that there is a particular quality of this injury that leads to patient’s choosing not to attend a follow-up appointment. We would suggest that this finding represents the excellent natural history of this fracture.
As this was a pragmatic study design and we could not justify exposing patients to additional clinical review or ionising radiation exposure, we did not routinely measure angulation or shortening. We also included all variations of fracture types of the 5th metacarpal in the study. We found no significant difference in satisfaction or functional outcome between these types.
The primary aim of this change in process was to improve the patient experience and reduce over medicalisation of an injury with an excellent natural history. There are additional economic benefits. Compared to a traditional system, this avoided 167 initial outpatient fracture clinic attendances along with the potential follow-up appointments. This has freed up clinical resources in clinic, which has allowed us to devote more time to patients with complex needs and develop other services. Indirect savings, such as those incurred outwith the orthopaedic service, are more difficult to quantify but would include administrative and transport savings. Conservative management of metacarpal fractures is four times less expensive to provide than surgical management [19]. It would therefore seem logical that there is even more substantial economical benefit where no follow-up is necessary. Considering that this injury is the most common type of fracture in the hand and classically occurs in the young, active, and employed population, the use of functional bracing to allow rapid return to work is important. Delaying return to work on such a proportion of our working population has a significant impact on our workforce. In addition, patients have higher satisfaction when discharged early and return earlier return to work [2].
This pathway is a safe and cost-effective option when targeted to this carefully selected high volume injury where conservative management provides excellent long-term results. Developing the new system required coordination and agreement between the Orthopaedic and Emergency Departments [23]. This system has now been used in the unit for 4 years, and popularity within the NHS is beginning to grow, with many other units redesigning their care of non-operatively managed fractures. The pathway was introduced to provide patient-centred care and prevent unnecessary medicalisation of simple, stable injuries with excellent natural histories.
A barrier to the implementation of this protocol has been concern that it would place added pressure on emergency department resources. Our unit currently treats a high number of these fractures using this method, and the results of a recent study found that there was no significant increase in workload and representation rates and that redesigning the fracture pathways is good for EDs as well as the orthopaedic unit and patients [23]. A further barrier has been concern that injuries that may require early intervention may be missed (false negative). Patient safety is paramount in the implementation of any new system, and a major fear in its deployment was the possibility of missing potentially serious injuries. A safety net is provided with all emergency department radiographs reviewed within 24 h by a radiologist and any significant discrepancies referred back to a senior clinician.
This study had a response rate of 59 % with a large cohort of 98 patients. This was comparable to other studies of this difficult population. Through the use of the QuickDASH score, we were able to assess functional outcome. Few studies of this fracture have assessed patient satisfaction with the system and outcome, which are key features in a successful management pathway. There were limitations in conducting the follow-up via questionnaire data with none of the patients being examined following their management. We are therefore unable to comment on features including range of movement, grip strength, and presence of extensor lag. We did not assess the radiological outcome. However, in obtaining this, we would have compromised our response rate to assess a parameter that has not been shown to correlate with functional outcome [24]. This study was based on short-term follow-up and, therefore, we are unable to comment on long-term outcomes.
Conclusion
Isolated fifth metacarpal fractures can be managed definitively in the ED without further face to face review, with good patient satisfaction and acceptable functional results. This “self-care” protocol has the potential to reduce unnecessary hospital attendances and inconvenience to patients. The time released from following up these injuries can be used to manage more complex injuries and develop other services.
References
Arafa M, Haines J, Noble J, et al. Immediate mobilization of fractures of the neck of the fifth metacarpal. Injury. 1986;17:277–88.
Bansal R, Craigen MA. Fifth metacarpal neck fractures: is follow-up required? J Hand Surg Br. 2007;32:69–7.
Beaton DE, Wright JG, Katz JN. Development of the QuickDASH: comparison of three item-reduction approaches. J Bone Joint Surg Am. 2005;87:1038–46.
Braakman M, Oderwald EE, Haentjens MH. Functional taping of fractures of the 5th metacarpal results in a quicker recovery. Injury. 1998;29:5–9.
Breddam M, Hansen TB. Subcapital fractures of the fourth and fifth metacarpals treated without splinting and reposition. Scand J Plast Reconstr Surg Hand Surg. 1995;29:269–70.
Ford DJ, Ali MS, Steel WM. Fractures of the fifth metacarpal neck: is reduction or immobilisation necessary? J Hand Surg Br. 1989;14:165–7.
Harding IJ, Parry D, Barrington RL. The use of a moulded metacarpal brace versus neighbour strapping for fractures of the little finger metacarpal neck. J Hand Surg Br. 2001;26:261–3.
Hunter JM, Cowen NJ. Fifth metacarpal fractures in a compensation clinic population. A report on one hundred and thirty-three cases. J Bone Joint Surg Am. 1970;52:1159–65.
Jayram PR, Bahattacharyya R, Jenkins PJ, et al. Patient satisfaction following management of radial head and neck fractures in a virtual fracture clinic. J Shoulder Elbow Surg. 2014;23:297–301.
Konradsen L, Nielsen PT, Albrecht-Beste E. Functional treatment of metacarpal fractures 100 randomized cases with or without fixation. Acta Orthop Scand. 1990;61:531–4.
Kuokkanen HO, Mulari-Keranen SK, Niskanen RO, et al. Treatment of subcapital fractures of the fifth metacarpal bone: a prospective randomised comparison between functional treatment and reposition and splinting. Scand J Plast Reconstr Surg Hand Surg. 1999;33:315–7.
Lowdon IM. Fractures of the metacarpal neck of the little finger. Injury. 1986;17:189–92.
McKerrell J, Bowen V, Johnston G, et al. Boxer’s fractures—conservative or operative management? J Trauma. 1987;27:486–90.
Poolman RW, Goslings JC, Lee JB, et al. Conservative treatment for closed fifth (small finger) metacarpal neck fractures. Cochrane Database Syst Rev. 2005;3:CD003210-CD003210.
Porter ML, Hodgkinson JP, Hirst P, et al. The boxer’s fracture: a prospective study of functional recovery. Arch Emerg Med. 1988;5:212–5.
Rabin R, De Charro F. EQ-5D: a measure of health status from the EuroQol Group. Ann Med. 2001;33(5):337–43.
Sorensen JS, Freund KG, Kejla G. Functional fracture bracing in metacarpal fractures: the Galveston metacarpal brace versus a plaster-of-Paris bandage in a prospective study. J Hand Ther. 1993;6:263–5.
Statius Muller MG, Poolman RW, van Hoogstraten MJ, et al. Immediate mobilization gives good results in boxer’s fractures with volar angulation up to 70 degrees: a prospective randomized trial comparing immediate mobilization with cast immobilization. Arch Orthop Trauma Surg. 2003;123:534–7.
TARMED Suisse, volume 2006. Bern: TARMED Suisse; 2006.
ten Berg PW, Ring D. Patients lost to follow-up after metacarpal fractures. J Hand Surg Am. 2012;37(1):42–6.
Theeuwen GA, Lemmens JA, van Niekerk JL. Conservative treatment of boxer’s fracture: a retrospective analysis. Injury. 1991;22:394–6.
Van Aaken J, Kampfen S, Berli M, et al. Outcome of boxer’s fractures treated by a soft wrap and buddy taping: a prospective study. Hand (N Y). 2007;2(4):212–7.
Vardy J, Jenkins PJ, Clark K, et al. Effect of a redesigned fracture management pathway and “virtual” fracture clinic on ED performance. BMJ Open. 2014;4:e005282. doi:10.1136/bmjopen-2014-005282.
Westbrook AP, Davis TR, Armstrong D, et al. The clinical significance of malunion of fractures of the neck and shaft of the little finger metacarpal. J Hand Surg Eur. 2008;33:732–9.
Conflicts of Interest
The Scottish Government Quality and Efficiency Support team provided a grant to our institution to support the audit of our change in practice.
The authors declare no other conflicts of interest.
Statement of Human and Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Deceleration of 1975, as revised in 2008. Informed consent was obtained from all patients for being included in the study.
Statement of Informed Consent
This study does not present patient identifying information. As such, patient consent was not obtained for the presentation of results in this manuscript. No additional individuals provided writing assistance for this manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
We received a Scottish Government grant to support the audit of our change in practice.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
ESM 1
(PDF 76 kb)
About this article
Cite this article
Gamble, D., Jenkins, P.J., Edge, M.J. et al. Satisfaction and functional outcome with “self-care” for the management of fifth metacarpal fractures. HAND 10, 607–612 (2015). https://doi.org/10.1007/s11552-015-9749-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11552-015-9749-8