Abstract
Purpose
Olivary degeneration is due to many posterior cranial fossa (PCF) lesions affecting the dentato-rubro-olivary pathway, also known as Guillain–Mollaret triangle. Triangle damage results in hyperexcitation and consequently in hypertrophy of the inferior olivary nucleus (ION). The aim of our study was to evaluate the incidence of magnetic resonance (MR) imaging changes in the ION after surgery in a large cohort of paediatric patients and to determine their correlation with tumour grade.
Materials and methods
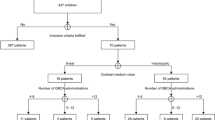
We retrospectively evaluated 58 patients treated surgically for PCF tumours who underwent MR imaging between 2007 and 2014, 1 week to 5 years after surgery. Histopathology revealed 29 medulloblastomas (WHO IV), 6 ependymomas (WHO II), 2 anaplastic ependymomas (WHO III) and 21 pilocytic astrocytomas (WHO I). ION MR imaging changes were correlated with surgery-to-MR interval and with tumour grading.
Results
ION MR imaging changes were observed in 19/64 (33 %), and all consisted of T2 signal alterations, 15 bilateral and four unilateral, with dentate nucleus damage in all cases. Olivary enlargement was observed in few cases only (7/19). ION T2 hyperintensity was always present between 1 and 6 months after surgery with a trend to decrease, becoming faint after 1 year. The Fisher test demonstrated a significant (p = 0.005) correlation between ION MR imaging changes and high tumour grade.
Conclusions
Our results demonstrate that olivary degeneration, with or without hypertrophy, is a relatively frequent consequence of posterior fossa surgery, particularly in children treated for high-grade tumours. Knowledge of this condition can prevent misdiagnoses and unnecessary investigations.





Similar content being viewed by others
References
Guillain G, Mollaret P (1931) Deuxcas de myoclonies synchrones et rhythmes velopharyngo-laryngo-oculo-diaphragmatiques. Rev Neurol 2:545–566
Goto N, Kaneko M (1981) Olivary enlargement: chronological and morphometric analyses. Acta Neuropathol 54:275–282
Birbamer G, Buchberger W, Felber S, Aichner F (1992) MRI appearance of hypertrophic olivary degeneration: temporal relationships. AJNR 13:1501–1503
Salamon-Murayama N, Russel E, Rabin B (1999) Case 17: hypertrophic olivary degeneration secondary to pontine hemorrhage. Radiology 213:814–817
Krings T, Foltys H, Meister IG, Reul J (2003) Hypertrophic olivary degeneration following pontine haemorrhage: hypertensive crisis or cavernous haemangioma bleeding? J Neurol Neurosurg Psychiatry 74:797–799
Arora V, Nijjar IS, Sandhu PS et al (2006) Hypertrophic olivary degeneration following trauma—a case report. Ind J Radiol Imag 16:701–704
Yun JH, Ahn JS, Park JC et al (2013) Hypertrophic olivary degeneration following surgical resection or gamma knife radiosurgery of brain stem cavernous malformations: an 11-case series and a review of literature. Acta Neurochir 155:469–476
Asal N, Yılmaz O, Turan A et al (2012) Hypertrophic olivary degeneration after pontine hemorrhage. Neuroradiology 54:413–415
Goyal M, Versnick E, Tuite P et al (2000) Hypertrophic olivary degeneration: metaanalysis of the temporal evolution of MR findings. AJNR 21:1073–1077
Patay Z, Enterkin J, Harreld JH et al (2014) MR imaging evaluation of inferior olivary nuclei: comparison of postoperative subjects with and without posterior fossa syndrome. AJNR 35:797–802
Kim SJ, Lee JH, Suh DC (1994) Cerebellar MR changes in patients with olivary hypertrophic degeneration. AJNR 15:1715–1719
Aberfeld DC (1996) The hypertrophic degeneration of the olives. Acta Neurol Scand 42:296–306
Uchino A, Hasuo K, Uchida K et al (1993) Olivary degeneration after cerebellar or brain stem haemorrhage: MRI. Neuroradiology 35:335–338
Gay AJ, Silberberg DH (1964) Histochemical correlates of transynaptic degeneration. Studies in the monkey lateral geniculate nucleus. Arch Neurol 10:85–90
Kitajima M, Korogi Y, Shimomura O et al (1994) Hypertrophic olivary degeneration: MR imaging and pathologic findings. Radiology 192:539–543
Sanverdi SE, Oguz KK, Haliloglu G (2012) Hypertrophic olivary degeneration in children: four new cases and a review of the literature with an emphasis on the MRI findings. Br J Radiol 85:511–516
Shinohara Y, Kinoshita T, Kinoshita F et al (2013) Hypertrophic olivary degeneration after surgical resection of brain tumors. Acta Radiol 54:462–466
Vossough A, Ziai P, Chatzkel JA (2012) Red nucleus degeneration in hypertrophic olivary degeneration after pediatric posterior fossa tumor resection: use of susceptibility-weighted imaging (SWI). Pediatr Radiol 42:481–485
Orman G, Bosemani T, Jallo GI et al (2014) Hypertrophic olivary degeneration in a child following midbrain tumor resection: longitudinal diffusor tensor imaging studies. J Neurosurg Pediatr 13:408–413
Gatlin JL, Wineman R, Schlakman B et al (2011) Hypertrophic olivary degeneration after resection of a pontine cavernous malformation: a case report. J Radiol Case Rep 5:24–29
Lim CC, Lim SA (2009) Pendular nystagmus and palatomyoclonus from hypertrophic olivary degeneration. N Engl J Med 360:e12
Shepherd GM, Tauboll E, Bakke SJ, Nyberg-Hansen R (1997) Midbrain tremor and hypertrophic olivary degeneration after pontine hemorrhage. Mov Disord 12:432–437
Harter DH, Davis A (2004) Hypertrophic olivary degeneration after resection of a pontine cavernoma, Case illustration. J Neurosurg 100:717
Phatouros CC, McConachie NS (1998) Hypertrophic olivary degeneration: case report in a child. Pediatr Radiol 28:830–883
Nowak J, Alkonyi B, Rutkowski S et al (2014) Hypertrophic olivary degeneration with gadolinium enhancement after posterior fossa surgery in a child with medulloblastoma. Childs Nerv Syst 30:959–962
Conflict of interest
The authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tartaglione, T., Izzo, G., Alexandre, A. et al. MRI findings of olivary degeneration after surgery for posterior fossa tumours in children: incidence, time course and correlation with tumour grading. Radiol med 120, 474–482 (2015). https://doi.org/10.1007/s11547-014-0477-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-014-0477-x