Abstract
SB3 is a biosimilar of trastuzumab that has been approved for use in the treatment of human epidermal growth factor 2-positive breast cancer and human epidermal growth factor 2-positive gastric cancer. Antibody-dependent cellular cytotoxicity is one of several critical quality attributes of trastuzumab. Data from the development of SB3 support the hypothesis of a relationship between antibody-dependent cellular cytotoxicity activity and clinical outcomes in terms of the response rate and long-term survival. Current analytic methods utilizing advanced technology allow the detection of small changes in other quality attributes that influence antibody-dependent cellular cytotoxicity, such as glycosylation and FcγRIIIa binding. Use of such methods to monitor batch-to-batch consistency enables production of trastuzumab biosimilars with consistent quality. Trastuzumab biosimilars such as SB3 therefore have the potential to increase accessibility to trastuzumab-based therapy without compromising efficacy or safety.
Similar content being viewed by others
Patterns of change were detected in certain quality attributes of the trastuzumab reference product that may affect clinical outcomes. |
In a clinical study of SB3 vs the trastuzumab reference product in patients with human epidermal growth factor 2-positive breast cancer, relatively high rates of breast pathologic complete response rates and long-term patient survival after SB3 treatment lend support to the hypothesis that critical quality attributes can influence clinical outcomes in terms of response rate and long-term survival. |
1 Introduction
Biologic drugs targeting human epidermal growth factor 2 (HER2), such as the anti-HER2 monoclonal antibody trastuzumab, have revolutionized the treatment of HER2-positive (HER2 +) breast cancer [1]. Trastuzumab-containing regimens are the standard of care for patients with early or metastatic HER2 + breast cancer and have considerably improved outcomes in these indications [2,3,4,5,6]. However, biologic drugs like trastuzumab are also expensive and account for much of the rising cost of cancer care [7, 8], placing enormous financial pressure on healthcare budgets and patients. Moreover, cost alone may prohibit access to biologic therapy, meaning that not all patients with HER2 + breast cancer receive trastuzumab as indicated with devastating consequences [9,10,11].
Patents for the trastuzumab reference product recently expired in the European Union (EU) and USA (2014 and 2019, respectively) [12], and several trastuzumab biosimilars have been approved for use in the treatment of HER2 + breast cancer, including SB3 (Ontruzant; Samsung Bioepis), PF-05280014 (Trazimera; Pfizer), MYL-1401O (Ogivri; Mylan), CT-P6 (Herzuma; Celltrion), and ABP 980 (Kanjinti; Amgen) [13,14,15]. These lower cost trastuzumab biosimilars, which are now being integrated into the latest European and North American breast cancer clinical practice guidelines [3, 6], have the potential to help contain rising healthcare expenditure and provide sustainable access to trastuzumab-based therapies in breast cancer care [10, 13, 16,17,18,19]. However, this may be undermined if oncologists are unsure of the quality of trastuzumab biosimilars and are reluctant to use them [7, 16]. Unlike chemically synthesized small-molecule medicines, which can be easily characterized and identically copied as generic drugs, biologic drugs are structurally complex, intrinsically variable molecules produced in living systems using complex manufacturing processes, and cannot be identically replicated [20,21,22]. A biosimilar is a biologic drug containing a similar version of the active substance of an already approved reference product with no clinically meaningful differences in quality, safety, or efficacy relative to the reference biologic drug [23,24,25]. The quality profiles of biosimilar and reference biologic drugs depend on physicochemical and functional critical quality attributes (CQAs).
In contrast to generic medications, for which European Medicines Agency and US Food and Drug Administration (FDA) approval is mainly based on the demonstration of bioequivalence with the original product in pharmacokinetic studies, the approval of biosimilars is a highly regulated and a uniquely detailed process [13, 20, 21, 26]. Biosimilars undergo a rigorous comprehensive comparability exercise that involves a step-wise approach to building a body of evidence (the totality of evidence) demonstrating biosimilarity with the reference product. Compared with the development process for reference products, there is more emphasis on the characterization of biosimilars in relation to quality, and less emphasis on clinical testing [21, 23, 25]. As is the case for all biologic drugs, once a biosimilar is approved, collection of post-marketing data and a risk management plan are required for pharmacovigilance purposes [16, 17, 21, 25]. Quality data that may affect the clinical safety and efficacy of trastuzumab (reference product and biosimilars) in patients with HER2 + breast cancer are reviewed in this article. In relation to this, we discuss the first published clinical results to support the hypothesis of a relationship between quality drifts in the trastuzumab reference product and long-term outcomes in patients with HER2 + breast cancer [27]. These results were observed during the development of the first European Medicines Agency-approved trastuzumab biosimilar, SB3.
2 Importance of Biologics Quality in Clinical Practice
The quality profiles of biosimilar and reference biologic drugs depend on quality attributes (QAs), which are the physicochemical and functional characteristics of a biologic drug that might affect its clinical profile [26]. Critical quality attributes are the foundation of the quality-by-design approach to drug development, which is dependent on a thorough understanding of the relationship between CQAs and the immunogenicity, safety, pharmacokinetics, and efficacy of the product [28, 29].
To guarantee consistent clinical performance, the quality profiles of approved biologic products must be consistently maintained, but biologics are inherently variable and all will demonstrate some degree of variability [28, 30]. Biologic drugs are also highly sensitive to changes in manufacturing conditions, thus even minor modifications to the manufacturing process can lead to drifts in QAs and add to variability [30,31,32]. Variations in QAs among different batches of the marketed biologic drugs etanercept and rituximab have been historically reported, including changes in the glycosylation profile of both products and the antibody-dependent cellular cytotoxicity (ADCC) activity of rituximab [33]. The size and abrupt nature of these changes suggest that they were a result of changes in manufacturing processes such as the production cell line, growth conditions and/or purification sequence, all of which influence the glycosylation profile [33].
Changes in biologic drug manufacturing processes are a common occurrence [34]. For example, the trastuzumab reference product has had more than 25 changes in manufacturing since its approval in the EU in 2000 [34]. In accordance with good pharmacovigilance practice, comparability exercises for pre- and post-change products must be performed to provide analytical evidence that differences in QAs introduced by manufacturing changes will not adversely impact the drug’s clinical profile [31, 34].
2.1 Trastuzumab Quality Attributes
At the time of development of SB3, product-specific QAs were organized into three tiers for statistical testing purposes as outlined by the FDA [23, 26]; this FDA guideline was withdrawn in 2018 [35]. Critical quality attributes were divided into tiers based on a criticality risk assessment of their impact on immunogenicity, safety, pharmacokinetics, and efficacy [26, 36]. High- and moderate-impact CQAs assessed using analytical methods amenable to statistical testing were assigned to tier 1 analysis (equivalence testing) and tier 2 analysis (quality range analysis), respectively [26, 36]. Low-impact QAs or QAs assessed using analytical methods not considered amenable to statistical analysis were assigned to a tier 3 analysis (comparison of raw data or graphical presentation of results) [26, 36]. Inhibition of cell proliferation and ADCC represent the major mechanisms of action of trastuzumab, with anti-proliferation activity mediated by binding of the trastuzumab Fab region to HER2, and ADCC activity mediated by the binding of the Fc region to Fcγ receptors (FcγRs) on immune effector cells [30, 37,38,39]. Anti-proliferation and ADCC activities were classified as tier 1 QAs for SB3 [36, 38]. Tier 2 QAs included HER2 binding, FcγRIIIa binding, and the sum level of afucose plus high mannose, which are glycoforms that have an influence on FcγRIIIa binding and ADCC activity [30, 36, 38]. Tier 3 QAs included FcγRIa, FcγRIIa, FcγRIIb, and FcγRIIb binding, in vitro angiogenesis, and surface HER2 expression [36].
To ensure that there are no clinically meaningful differences between the biosimilar and the reference product, CQAs must be within a pre-specified target range that accounts for expected batch-to-batch variability and is representative of the reference product [26, 28, 40]. For example, the equivalence margin for equivalence testing of SB3 tier 1 QAs was based on 1.5 times the variability of trastuzumab reference product lots [36]. Once approved, it is particularly important that the QAs related to the mechanism of action are consistently maintained over time. Therefore, CQAs such as the HER2-binding assay, anti-proliferation assay, and FcγRIIIa binding assay were included as part of the release specification throughout the product life cycle of SB3 in the USA [36].
2.2 Trastuzumab Reference Product Quality Drifts
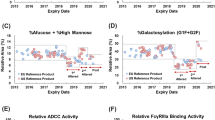
As part of the biosimilar development process, the physicochemical and functional properties of different batches of the reference product should be monitored frequently over a long-term period so that unintended patterns of change in CQAs can be detected and an accurate quality target range based on non-drifted batches can be established [30, 38, 40]. SB3 was developed based on an in-depth understanding of trastuzumab QAs obtained by analyzing up to 154 lots of EU- and US-sourced trastuzumab reference products for up to 8 years using standard and the latest state-of-the-art analytic techniques, including fluorescence resonance energy transfer to assess HER2 binding, Alphascreen™ technology to assess Fc-related biologic activity, and a hydrophilic interaction liquid chromatography-ultra-performance liquid chromatography system for analysis of glycosylation [30, 38]. In relation to glycosylation (determined by hydrophilic interaction liquid chromatography-ultra-performance liquid chromatography), FcγRIIIa binding (assessed using Alphascreen™), and ADCC activity (assessed in the HER2-overexpressing human breast cancer cell line SKBR3 using a CytoTox-Glo® kit), two periods of drift were observed for batches of trastuzumab reference product with expiry dates ranging from mid-2018 to December 2019, as reported by Kim et al. and Lee et al. (Fig. 1) [30, 38]. A marked downward drift in %afucose plus %high mannose, FcγRIIIa binding activity, and ADCC activity during the first drift period was followed by an upward drift in the second drift period [30], with these CQAs returning to pre-change levels in the more recently monitored lots [30, 38]. There was no change in the antiproliferative activity of the trastuzumab reference product, which was assessed using CellTiter-Blue® or BrdU proliferation assay to indicate cell viability in the HER2-overexpressing human breast cancer cell line BT474 [30, 38]. Overall, relative ADCC activity was correlated with the sum of %afucose plus %high-mannose [38]. Drifted lots of the trastuzumab reference product were not included in the CQA target ranges for SB3, and the SB3 used in clinical trials was similar to the pre-drift trastuzumab reference product [38, 41].

Adapted from Kim et al. (2017) (Fig. 1c) and 711 (Fig. 5a, b). RP reference product
Changes in a %Afucose plus %high mannose, b FcγRIIIa binding, andc antibody-dependent cell-mediated cytotoxicity (ADCC) activity for multiple lots of European Union (EU)- and US-sourced trastuzumab reference product expiring between March 2015 and December 2019 [30].
Considering that ADCC is one of the main mechanisms of action of trastuzumab, the drift in ADCC activity observed with the trastuzumab reference product may potentially have an impact on clinical efficacy [30, 38, 42]. This was suggested in phase III equivalence studies of SB3 and ABP 980, which were conducted by Pivot et al. and von Minckwitz et al., respectively, in patients with HER2 + early breast cancer using the trastuzumab reference product sourced from a combination of batches with expiry dates within and outside the drift period [41,42,43,44]. In these studies, the upper limits of the confidence intervals (CIs) for pathological complete response (pCR) primary endpoints for neoadjuvant SB3 and ABP 980 vs the trastuzumab reference product exceeded predefined equivalence margins, meaning that potential superiority could not be ruled out [41, 44].
In the SB3 and the ABP 980 equivalence studies, equivalence was assessed on the basis of the risk ratio and risk difference of pCR [41, 44]. The primary pCR endpoint was defined as the absence of histologic evidence of residual invasive tumor cells in the breast (bpCR) in the SB3 study [41], and as the total pCR (tpCR) in the breast tissue and axillary lymph nodes in the ABP 980 study [44]. Total pCR was included as a secondary endpoint in the SB3 study, and bpCR was included as a secondary endpoint in the ABP 980 study. In both studies, the primary pCR analysis was based on local laboratory findings, but the ABP 980 study was the first large, international, multicenter neoadjuvant breast cancer study to conduct a sensitivity analysis based on a central independent laboratory review of tumor samples, which has the potential to reduce inter-pathologist variability [41, 44,45,46]. In the SB3 study, the risk difference was 10.70% (95% CI 4.13–17.26), with a lower upper boundary of the 95% CI within the predefined equivalence margin of ± 13%, and the upper boundary exceeding it, demonstrating non-inferiority but not non-superiority [41]. The bpCR ratio of 1.259 (90% CI 1.112–1.426) was, however, within the predefined 90% CI equivalence margin (0.785–1.546), demonstrating equivalent efficacy [47]. Based on a local laboratory review of tumor samples in the ABP 980 study, the upper bounds of the 90% CI for the tpCR risk difference (7.3%; 90% CI 1.2–13.4) and risk ratio (1.88; 90% CI 1.033–1.366) exceeded the predefined 90% CI equivalence margins of ± 13% and 0.759–1.318, respectively [44]. However, the tpCR risk difference (5.8; 90% CI 0.5 to 12.0) and risk ratio (1.142; 90% CI 0.993–1.312) obtained after central review of tumor samples were contained within the predefined equivalence margins, indicating similar efficacy [44].
A proposed biosimilar cannot be superior to its reference product [23, 40, 46], but in the ABP 980 and SB3 phase III equivalence studies, it was observed that pCR rates were lower in patients treated with drifted batches of the trastuzumab reference product than those treated with the pre-drifted trastuzumab reference product or biosimilar trastuzumab [42, 43]. As described in European Public Assessment Reports for SB3 and ABP 980 [42, 43], it has been acknowledged that the downward drifts in ADCC activity in some of the trastuzumab reference product batches used in these studies could have at least partially confounded the results by contributing to the observed differences in pCR rates between treatment arms and their relatively high upper CI limits [13, 15]. Taking totality of evidence into account, SB3 and ABP 980 were therefore considered comparable, rather than superior, to the reference product, and approved as biosimilars of trastuzumab [15, 42, 43, 45].
3 Confirming Biosimilarity of SB3 Based on Clinical Evidence
There are generally two clinical steps involved in the development of biosimilars: a phase I pharmacokinetic equivalence study in healthy volunteers followed by a pivotal phase III clinical equivalence study in an appropriate patient population [13, 23, 25]. Clinical studies of potential biosimilars are designed to detect clinically meaningful differences between the biosimilar and the reference product [21, 23, 25]. As well as being assessed during the pivotal clinical efficacy study, clinical safety and immunogenicity are initially assessed during clinical pharmacokinetic studies [23, 25].
3.1 Phase I Studies
The primary aim of the phase I study is to demonstrate pharmacokinetic equivalence of a biosimilar candidate and its reference product, usually in healthy volunteers [13, 25]. Compared with patients who may have disease-related factors and take concomitant medications that influence pharmacokinetic profiles, healthy volunteers represent a relatively homogenous group in which to detect clinically meaningful drug-related pharmacokinetic differences between the biosimilar and reference products [13, 25]. Although a single-dose crossover study design can reduce pharmacokinetic variability, a parallel study design is most appropriate for monoclonal antibodies with long half-lives because of the risk of immune response after repeated exposures. [13, 25].
Pharmacokinetic equivalence was observed for SB3 and US- and EU-sourced trastuzumab reference products in a randomized, parallel, single-dose pharmacokinetic study in 108 healthy male volunteers, with 90% CIs for the primary area under the curve and maximum concentration pharmacokinetic parameters falling within the pre-specified 0.8–1.25 equivalence margin [48]. In addition, a pharmacokinetic analysis was performed as a secondary endpoint in a subset of patients with HER2 + breast cancer in the phase III clinical study comparing SB3 and the trastuzumab reference product. Mean trough concentration profiles were similar and within predefined equivalence margins in cycles 3–8 for SB3 and for the trastuzumab reference product [41].
3.2 Phase III Studies
The aim of phase III biosimilarity clinical trials is not to independently establish safety and efficacy of the biosimilar, which has already been established in clinical trials conducted with the reference product, but to demonstrate comparable clinical performance of the biosimilar in relation to the reference product and to resolve residual uncertainty [21, 25, 26]. The statistical design, patient population, and primary endpoints of the study are therefore selected to facilitate the detection of differences between the two products [21, 23, 25]. In general, a phase III equivalence design with a pre-specified equivalence margin is recommended to rule out inferiority or superiority of the biosimilar candidate to its reference product in the most sensitive and homogenous patient population possible using practical and sensitive endpoints [23, 25, 49]. A recommended approach for deriving equivalence margins relies on preserving 50‒60% of the reference treatment effect based on major historic studies [50, 51].
Phase III studies of trastuzumab biosimilar candidates are often conducted in patients with early breast cancer, which, compared with metastatic disease, represents a relatively homogenous population with fewer confounding factors, such as metastatic burden and previous therapies, to influence efficacy and safety evaluations [13, 22, 49]. Long-term survival endpoints, which are the preferred primary efficacy endpoints in cancer indications, may not be feasible or sufficiently sensitive to demonstrate comparability, thus shorter term surrogate endpoints can be used, including pCR, which is correlated with long-term survival in the neoadjuvant breast cancer setting [13, 22, 47, 49, 52, 53]. Pathological complete response may be assessed as bpCR or tpCR. Although tpCR has a stronger correlation with long-term survival, bpCR avoids confounding factors related to axillary lymph node status and assessment [41, 50]. Initial use of a surrogate endpoint like pCR does not obviate the need to assess survival during a longer term follow-up [13, 22].
As previously mentioned in this review, a large randomized double-blind study of SB3 vs the trastuzumab reference product was conducted in women with early or locally advanced HER2 + breast cancer (n = 875) using bpCR assessed after neoadjuvant treatment as the primary endpoint [41]. In relation to predefined equivalence margins, the 10.7% risk difference in bpCR rates observed in this equivalence study (51.7% with SB3 and 42.0% with the trastuzumab reference product) ruled out inferiority but not superiority of SB3, whereas the risk ratio of bpCR rates demonstrated equivalence. After surgery, patients received adjuvant treatment with SB3 or the trastuzumab reference product to complete 1 year of treatment [41]. Event-free survival (EFS) was included as a secondary endpoint [41]. After completion of neoadjuvant and adjuvant therapy, Pivot et al. reported that there was no difference in EFS between SB3 and the trastuzumab reference product and bpCR and tpCR were shown to be significantly related to EFS, supporting their validity as surrogate markers for survival [47]. Safety profiles of SB3 and the trastuzumab reference product were similar throughout the study, with no unexpected safety issues, and the overall incidence of anti-drug antibody was low (0.7%) [41, 47].
3.3 SB3 Extension Study
A 5-year treatment-free extension of the phase III study is ongoing to assess the cardiac safety of SB3 (ClinicalTrials.gov identifier: NCT02771795) [27], reflecting a cautious pharmacovigilance approach. In addition to cardiac and other safety outcomes, EFS and overall survival (OS) are being assessed. Demographic and baseline disease characteristics of patients participating in the extension study (n = 367) reflect the composition of the main study, with no apparent differences between the SB3 and trastuzumab reference product treatment arms [27, 41]. Patients in the extension study had no symptomatic cardiac events during the main study and had no early breast cancer recurrence during adjuvant therapy [27]. Pivot et al. have reported 3-year follow-up data from the extension study [27]. During the 3-year follow-up after the completion of adjuvant treatment, cardiac events were very rare [27]. Asymptomatic significant decreases in left ventricular ejection fraction were reported in one (0.5%) patient treated with SB3 and two (1.1%) patients treated with the trastuzumab reference product [27]. No other cardiac-related events were reported [27]. Unlike the comparable EFS rates obtained in the two treatment arms at the end of the main study [44], the 3-year EFS rate was higher with SB3 (91.9%) than with the trastuzumab reference product (85.2%), with events occurring in 17 (9.1%) and 31 (17.1%) patients, respectively, resulting in a hazard ratio of 0.47 (95% CI 0.26‒0.87) [27]. The 3-year OS rate was 97.0% with SB3 and 92.9% with the trastuzumab reference product [27].
Pivot et al. performed a post hoc analysis of the 3-year follow-up data from the extension study to identify factors contributing to the surprising difference in EFS observed between the SB3 and trastuzumab reference product treatment arms [27]. Among the covariates analyzed, ADCC activity and bpCR (or tpCR) were the only factors associated with EFS (Fig. 2) [27]. Antibody-dependent cellular cytotoxicity activity was designated according to whether patients treated with the trastuzumab reference product were exposed to a trastuzumab lot with drifted ADCC activity during neoadjuvant treatment (n = 126 and 55, respectively) [27]. Among the 25 lots of trastuzumab reference product used during the neoadjuvant period in the main study, the ADCC activities of 12 lots were analyzed directly [27]. Antibody-dependent cellular cytotoxicity activity for the remaining 13 lots was assumed based on their expiry dates and drifts in ADCC activity previously reported by Kim et al. [30], thus lots with expiry dates from August 2018 to December 2019 were assumed to have drifted ADCC activity [27]. Overall, 13 trastuzumab reference product lots were classified as having a drift in ADCC activity (eight based on available analyses and five based on expiry dates), and the remainder 12 lots were considered to have non-drifted ADCC activity (four based on available analysis and eight based on expiry dates) [27]. There was insufficient power to test the hypothesis of a relationship between ADCC activity and EFS, but the 3-year EFS rate was higher in patients not exposed to the drifted trastuzumab reference product (92.7%) than in those exposed to the drifted product (81.7%), whereas, as a result of comparable events rates (hazard ratio 0.93; 95% CI, 0.31‒2.85), EFS curves for SB3 and the non-drifted trastuzumab reference product appeared superimposable (Fig. 3) [27]. Similar trends were observed for OS, but a longer follow-up is required to analyze the effect of ADCC status on OS [27].
Factors influencing event-free survival (using breast pathologic complete response [bpCR] status as a covariate) in patients with human epidermal growth factor 2-positive breast cancer randomized to neoadjuvant plus the adjuvant trastuzumab reference product (TRZ)- or SB3-based therapy during a phase III study and followed for 3 years thereafter during an extension study [27]. Adapted from Pivot et al. (2019) (Fig. 4a). Drifted = patients who were exposed to at least one vial from a drifted TRZ lot during the neoadjuvant period. Non-drifted = patients who were never exposed to any vials from a drifted TRZ lot during the neoadjuvant period. Positive = estrogen receptor and/or progesterone receptor positive. Negative = estrogen receptor and progesterone receptor negative. ADCC antibody-dependent cell-mediated cytotoxicity, CI confidence interval, HR hazard ratio
Kaplan–Meier curve for event-free survival for SB3, non-drifted trastuzumab reference product (TRZ), and drifted TRZ in patients with human epidermal growth factor 2-positive breast cancer randomized to neoadjuvant plus adjuvant TRZ- or SB3-based therapy during a phase III study and followed for 3 years thereafter during an extension study [27]. Adapted from Pivot et al. (2019) (Fig. 3a). Non-drifted TRZ = patients who were never exposed to any vials from a drifted TRZ lot during the neoadjuvant period. Drifted TRZ = patients who were exposed to at least one vial from a drifted TRZ lot during the neoadjuvant period. CI confidence interval, HR hazard ratio
4 Conclusions
Technology has advanced enormously since the first approval of the original trastuzumab product over 20 years ago, with current analytic methods allowing the detection of small changes in QAs such as FcγRIIIa binding and glycosylation and enabling sensitive monitoring of batch-to-batch consistency [30, 38, 54]. This is very important as small changes in FcγRIIIa binding and the level of fucose and mannose affect trastuzumab ADCC activity and potentially impact clinical outcomes, including long-term survival. Biosimilar companies are at the forefront of technology and are therefore able to produce trastuzumab biosimilars at the most technologically advanced capacity, with CQAs that are consistently within target range. Going forward, all drug companies manufacturing biosimilar or reference biologic drugs should release frequent quality data to assure that efficacy and safety demonstrated in clinical trials will be maintained in clinical practice.
Based on the totality of the evidence, which includes sophisticated analytic and clinical assessments, approved biosimilars of trastuzumab, such as SB3, have the potential to increase accessibility to trastuzumab-based therapy without compromising efficacy or safety [13, 15, 27, 30, 38, 41, 44]. Furthermore, although the phase III study of SB3 in patients with early HER2 + breast cancer was not designed to detect a relationship between ADCC and clinical outcomes, and survival results by exposure to ADCC drift were derived from a post hoc analysis, the SB3 development process has provided some evidence to support the hypothesis of a relationship between ADCC activity and long-term survival [27]. At the very least, it highlights an underlying need to consistently provide patients with the best quality trastuzumab. Well characterized European Medicines Agency- and/or FDA-approved trastuzumab biosimilars have fulfilled this need.
Change history
20 October 2020
The article Biologic Drug Quality Assurance to Optimize HER2+���Breast Cancer Treatment: Insights from Development of the Trastuzumab Biosimilar SB3,
References
Loibl S, Gianni L. HER2-positive breast cancer. Lancet. 2017;389:2415–29.
Cardoso F, Kyriakides S, Ohno S, Penault-Llorca F, Poortmans P, Rubio IT, et al. Early breast cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up†. Ann Oncol. 2019;30:1194–220.
Cardoso F, Senkus E, Costa A, Papadopoulos E, Aapro M, André F, et al. 4th ESO-ESMO international consensus guidelines for advanced breast cancer (ABC 4)†. Ann Oncol. 2018;29:1634–57.
Denduluri N, Chavez-MacGregor M, Telli ML, Eisen A, Graff SL, Hassett MJ, et al. Selection of optimal adjuvant chemotherapy and targeted therapy for early breast cancer: ASCO clinical practice guideline focused update. J Clin Oncol. 2018;36:2433–43.
Giordano SH, Temin S, Chandarlapaty S, Crews JR, Esteva FJ, Kirshner JJ, et al. Systemic therapy for patients with advanced human epidermal growth factor receptor 2-positive breast cancer: ASCO clinical practice guideline update. J Clin Oncol. 2018;36:2736–40.
National Comprehensive Cancer Network. NCCN Clinical practice guidelines in oncology: breast cancer. Version 3. 2019. https://www.nccn.org/professionals/physician_gls/default.aspx#site. Accessed 16 Jun 2020.
Lyman GH, Zon R, Harvey RD. Rationale, opportunities, and reality of biosimilar medications. N Engl J Med. 2018;379:694–5.
Nixon NA, Hannouf MB, Verma S. The evolution of biosimilars in oncology, with a focus on trastuzumab. Curr Oncol. 2018;25:S171–9.
Bazargani YT, de Boer A, Schellens JHM, Leufkens HGM, Mantel-Teeuwisse AK. Essential medicines for breast cancer in low and middle income countries. BMC Cancer. 2015;15:591.
Lammers P, Criscitiello C, Curigliano G, Jacobs I. Barriers to the use of trastuzumab for HER2 + breast cancer and the potential impact of biosimilars: a physician survey in the United States and emerging markets. Pharmaceuticals (Basel). 2014;7:943–53.
Jackisch C, Lammers P, Jacobs I. Evolving landscape of human epidermal growth factor receptor 2-positive breast cancer treatment and the future of biosimilars. Breast. 2017;32:199–216.
GaBi Online. US$67 billion worth of biosimilar patents expiring before 2020. 2014. http://www.gabionline.net/Biosimilars/General/US-67-billion-worth-of-biosimilar-patents-expiring-before-2020. Accessed 16 Jun 2020.
Barbier L, Declerck P, Simoens S, Neven P, Vulto AG, Huys I. The arrival of biosimilar monoclonal antibodies in oncology: clinical studies for trastuzumab biosimilars. Br J Cancer. 2019;121:199–210.
US Food and Drug Administration. Biosimilar product information. 2019. https://www.fda.gov/drugs/biosimilars/biosimilar-product-information. Accessed 16 Jun 2020.
Stebbing J, Mainwaring PN, Curigliano G, Pegram M, Latymer M, Bair AH, et al. Understanding the role of comparative clinical studies in the development of oncology biosimilars. J Clin Oncol. 2020;38:1070–80.
Lyman GH, Balaban E, Diaz M, Ferris A, Tsao A, Voest E, et al. American Society of Clinical Oncology statement: biosimilars in oncology. J Clin Oncol. 2018;36:1260–5.
Tabernero J, Vyas M, Giuliani R, Arnold D, Cardoso F, Casali PG, et al. Biosimilars: a position paper of the European Society for Medical Oncology, with particular reference to oncology prescribers. ESMO Open. 2016;1:e000142.
Zelenetz AD, Ahmed I, Braud EL, Cross JD, Davenport-Ennis N, Dickinson BD, et al. NCCN biosimilars white paper: regulatory, scientific, and patient safety perspectives. J Natl Compr Cancer Netw. 2011;9(Suppl. 4):S1–22.
Liedtke C, Jackisch C, Thill M, Thomssen C, Müller V, Janni W, et al. Recommendations for the diagnosis and treatment of patients with early breast cancer: update 2018. Breast Care (Basel). 2018;13:196–208.
Declerck PJ. Biologicals and biosimilars: a review of the science and its implications. GaBI J. 2012;1:13–6.
European Medicines Agency, European Commission. Biosimilars in the EU: information guide for healthcare professionals. 2019. https://www.ema.europa.eu/en/human-regulatory/overview/biosimilar-medicines-overview. Accessed 16 Jun 2020.
Pivot X, Aulagner G, Blay JY, Fumoleau P, Kaliski A, Sarkozy F, et al. Challenges in the implementation of trastuzumab biosimilars: an expert panel’s recommendations. Anticancer Drugs. 2015;26:1009–16.
US Food and Drug Administration, Center for Drug Evaluation and Research, Center for Biologics Evaluation and Research. Scientific considerations in demonstrating biosimilarity to a reference product: guidance for industry. 2015. https://www.fda.gov/downloads/drugs/guidancecomplianceregulatoryinformation/guidances/ucm291128.pdf. Accessed 16 Jun 2020.
World Health Organization. Expert Committee on Biological Standardization: guidelines on evaluation of similar biotherapeutic products (SBPs). 2009. https://www.who.int/biologicals/areas/biological_therapeutics/BIOTHERAPEUTICS_FOR_WEB_22APRIL2010.pdf. Accessed 16 Jun 2020.
European Medicines Agency. Guideline on similar biological medicinal products containing biotechnology-derived proteins as active substance: non-clinical and clinical issues. 2014. http://www.ema.europa.eu/docs/en_GB/document_library/Scientific_guideline/2015/01/WC500180219.pdf. Accessed 16 Jun 2020.
Kirchhoff CF, Wang X-ZM, Conlon HD, Anderson S, Ryan AM, Bose A. Biosimilars: key regulatory considerations and similarity assessment tools. Biotechnol Bioeng. 2017;114:2696–705.
Pivot X, Pegram M, Cortes J, Lüftner D, Lyman GH, Curigliano G, et al. Three-year follow-up from a phase 3 study of SB3 (a trastuzumab biosimilar) versus reference trastuzumab in the neoadjuvant setting for human epidermal growth factor receptor 2-positive breast cancer. Eur J Cancer. 2019;120:1–9.
Gonçalves J, Araújo F, Cutolo M, Fonseca JE. Biosimilar monoclonal antibodies: preclinical and clinical development aspects. Clin Exp Rheumatol. 2016;34:698–705.
Rathore AS. Roadmap for implementation of quality by design (QbD) for biotechnology products. Trends Biotechnol. 2009;27:546–53.
Kim S, Song J, Park S, Ham S, Paek K, Kang M, et al. Drifts in ADCC-related quality attributes of Herceptin®: impact on development of a trastuzumab biosimilar. MAbs. 2017;9:704–14.
European Medicines Agency. Guideline on good pharmacovigilance practices (GVP): product- or population-specific considerations II: biological medicinal products. 2016. http://www.ema.europa.eu/docs/en_GB/document_library/Scientific_guideline/2016/08/WC500211728.pdf. Accessed 16 Jun 2020.
Ramanan S, Grampp G. Drift, evolution, and divergence in biologics and biosimilars manufacturing. BioDrugs. 2014;28:363–72.
Schiestl M, Stangler T, Torella C, Cepeljnik T, Toll H, Grau R. Acceptable changes in quality attributes of glycosylated biopharmaceuticals. Nat Biotechnol. 2011;29:310–2.
Vezér B, Buzás Z, Sebeszta M, Zrubka Z. Authorized manufacturing changes for therapeutic monoclonal antibodies (mAbs) in European Public Assessment Report (EPAR) documents. Curr Med Res Opin. 2016;32:829–34.
US Food and Drug Administration. FDA withdraws draft guidance for industry: statistical approaches to evaluate analytical similarity. 2018. https://www.fda.gov/drugs/drug-safety-and-availability/fda-withdraws-draft-guidance-industry-statistical-approaches-evaluate-analytical-similarity. Accessed 16 Jun 2020.
US Food and Drug Administration, Center for Drug Evaluation and Research. Product quality review(s), 761100Orig1s000. Trastuzumab-dttb. 2018. https://www.accessdata.fda.gov/drugsatfda_docs/nda/2019/761100Orig1s000ChemR.pdf. Accessed 16 Jun 2020.
Clynes RA, Towers TL, Presta LG, Ravetch JV. Inhibitory Fc receptors modulate in vivo cytotoxicity against tumor targets. Nat Med. 2000;6:443–6.
Lee JH, Paek K, Moon JH, Ham S, Song J, Kim S. Biological characterization of SB3, a trastuzumab biosimilar, and the influence of changes in reference product characteristics on the similarity assessment. BioDrugs. 2019;33:411–22.
Hudis CA. Trastuzumab: mechanism of action and use in clinical practice. N Engl J Med. 2007;357:39–51.
European Medicines Agency. Guideline on similar biological medicinal products containing biotechnology-derived proteins as active substances: quality issues (revision 1). 2014. http://www.ema.europa.eu/docs/en_GB/document_library/Scientific_guideline/2014/06/WC500167838.pdf. Accessed 16 Jun 2020.
Pivot X, Bondarenko I, Nowecki Z, Dvorkin M, Trishkina E, Ahn J-H, et al. Phase III, randomized, double-blind study comparing the efficacy, safety, and immunogenicity of SB3 (trastuzumab biosimilar) and reference trastuzumab in patients treated with neoadjuvant therapy for human epidermal growth factor receptor 2-positive early breast cancer. J Clin Oncol. 2018;36:968–74.
European Medicines Agency. EMA/CHMP/9855/2018: assessment report: ontruzant. 2017. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_Public_assessment_report/human/004323/WC500242488.pdf. Accessed 16 Jun 2020.
European Medicines Agency. EMA/CHMP/261937/2018: assessment report: Kanjinti. 2018. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_Public_assessment_report/human/004361/WC500249709.pdf. Accessed 16 Jun 2020.
von Minckwitz G, Colleoni M, Kolberg H-C, Morales S, Santi P, Tomasevic Z, et al. Efficacy and safety of ABP 980 compared with reference trastuzumab in women with HER2-positive early breast cancer (LILAC study): a randomised, double-blind, phase 3 trial. Lancet Oncol. 2018;19:987–98.
Kolberg H-C, Colleoni M, Santi P, Demetriou GS, Segui-Palmer MA, Fujiwara Y, et al. Totality of scientific evidence in the development of ABP 980, a biosimilar to trastuzumab. Target Oncol. 2019;14:647–56.
Martin M. The LILAC trial and the blooming of anticancer biosimilars. Lancet Oncol. 2018;19:861–3.
Pivot X, Bondarenko I, Nowecki Z, Dvorkin M, Trishkina E, Ahn J-H, et al. A phase III study comparing SB3 (a proposed trastuzumab biosimilar) and trastuzumab reference product in HER2-positive early breast cancer treated with neoadjuvant-adjuvant treatment: final safety, immunogenicity and survival results. Eur J Cancer. 2018;93:19–27.
Pivot X, Curtit E, Lee YJ, Golor G, Gauliard A, Shin D, et al. A randomized phase I pharmacokinetic study comparing biosimilar candidate SB3 and trastuzumab in healthy male subjects. Clin Ther. 2016;38(1665–73):e3.
Jackisch C, Scappaticci FA, Heinzmann D, Bisordi F, Schreitmüller T, von Minckwitz G, et al. Neoadjuvant breast cancer treatment as a sensitive setting for trastuzumab biosimilar development and extrapolation. Future Oncol. 2015;11:61–71.
Pivot X, Petit T. Can we establish a hierarchy among trastuzumab biosimilar candidates? Br J Cancer. 2018;119:263–5.
US Food and Drug Administration, Center for Drug Evaluation and Research, Center for Biologics Evaluation and Research. Non-inferiority clinical trials to establish effectiveness: guidance for industry. 2016. https://www.fda.gov/media/78504/download. Accessed 16 Jun 2020.
Cortazar P, Zhang L, Untch M, Mehta K, Costantino JP, Wolmark N, et al. Pathological complete response and long-term clinical benefit in breast cancer: the CTNeoBC pooled analysis. Lancet. 2014;384:164–72.
Jackisch C, Hegg R, Stroyakovskiy D, Ahn J-S, Melichar B, Chen S-C, et al. HannaH phase III randomised study: association of total pathological complete response with event-free survival in HER2-positive early breast cancer treated with neoadjuvant-adjuvant trastuzumab after 2 years of treatment-free follow-up. Eur J Cancer. 2016;62:62–75.
Xie L, Zhang E, Xu Y, Gao W, Wang L, Xie MH, et al. Demonstrating analytical similarity of trastuzumab biosimilar HLX02 to Herceptin® with a panel of sensitive and orthogonal methods including a novel FcγRIIIa affinity chromatography technology. BioDrugs. 2020;34:363–79.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Author contributions
Not applicable
Availability of data and material
Not applicable
Conflicts of interest/Competing interests
Gary H. Lyman, João Gonçalves, and Xavier Pivot have received consulting fees and/or speaking honoraria from Samsung Bioepis; João Gonçalves has received speaker honoraria and consulting fees from Amgen and Samsung Bioepis; Minji Seo is an employee of Samsung Bioepis. Diana Lüftner has no conflicts of interest that are directly relevant to the content of this article.
Consent to participate
Not applicable
Consent for publication
Not applicable
Code availability
Not applicable
Funding
The authors acknowledge Weber Shandwick Hong Kong for editorial support in the preparation of this manuscript with funding from Samsung Bioepis.
Additional information
The original version of this article was revised due to a retrospective Open Access order.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Lüftner, D., Lyman, G.H., Gonçalves, J. et al. Biologic Drug Quality Assurance to Optimize HER2 + Breast Cancer Treatment: Insights from Development of the Trastuzumab Biosimilar SB3. Targ Oncol 15, 467–475 (2020). https://doi.org/10.1007/s11523-020-00742-w
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11523-020-00742-w