Abstract
Background
Several techniques have been used to repair mid-penile hypospadias; however, high failure rates and major complications have been reported. In this study, we describe a novel technique using a well-vascularized flap of the inner and outer preputial skin.
Methods
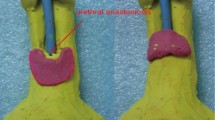
A total of 110 male children with hypospadias underwent repair by our technique between 2008 and 2015. The inclusion criteria were children with mid-penile or slightly more proximal hypospadias, with or without ventral chordae, and an intact prepuce of the cobra eyes variety. Recurrent cases, patients with other preputial types, and circumcised children were excluded from this study. The prepared flap was sutured in its natural longitudinal orientation to the created urethral plate strip to form a neo-urethra over a urethral catheter. Outcome measures included surgical success without the formation of a urethra-cutaneous fistula, no ischaemia of the flaps, glans dehiscence or infection and functional outcome and cosmetic appearance.
Results
The median follow-up duration was 3.3 years. There were 63 cases of mid-penile hypospadias (57.3 %), and in 47 cases (42.7 %), the meatus was slightly more proximal. The age of the patients ranged from 1.1 to 8.0 years, with a mean age of 4.6 ± 1.2 years. Surgery was successful in 106 (96.4 %) cases. Minor complications occurred in 11 patients (10 %) and included oedema of glans in ten patients and bluish discoloration on the ventral aspect of the glans close to the suture line in three patients. All patients improved within 2 weeks after surgery. Long-term follow-up revealed a properly functioning urethra with a forward, projectile, single, compact, and rifled urinary stream of adequate calibre and cosmetically acceptable repair. No cases of meatal retraction, meatal stenosis, urethral stricture, or acquired urethral diverticulum occurred.
Discussion
Our technique is different from the split prepuce in situ technique. We create a narrow strip of the urethral plate that facilitates glanular closure, and we use the inner and adjacent outer skin in a vertical manner to preserve excess skin for penile coverage. Prepuce is split at midline to preserve more preputial skin with favourable dartos tissue for penile skin coverage. The glans is closed using a stitch-by-stitch method that has not been described previously.
Conclusion
This study presents a novel technique for mid-penile hypospadias repair using a preputial skin flap with excellent results in terms of short- and long-term outcomes.








Similar content being viewed by others
References
Radojicic ZI, Perovic SV (2004) Classification of prepuce in hypospadias according to morphological abnormalities and their impact on hypospadias repair. J Urol 172(1):301–304
Duplay S (1874) De l’hypospadias perineo-scrotal et de son traitement chirurgical. Arch Gen Med 23:513
Santangelo K, Rushton HG, Belman AB (2003) Outcome analysis of simple and complex urethrocutaneous fistula closure using a de-epithelialized or full-thickness skin advancement flap for coverage. J Urol 170:1589
Gonazlez R, Smith C, Denes ED (1996) Double onlay preputial flap for proximal hypospadias repair. J Urol 156:832–835
Jayanthi V (2003) The modified Snodgrass hypospadias repair: reducing the risk of fistula and meatal stenosis. J Urol 170:1603
Snodgrass W, Yucel S (2007) Tubularized incised plate for midshaft and proximal hypospadias repair. J Urol 177:698
Braga LHP, Pippi Salle JL, Lorenzo AJ, Skeldon S, Dave S, Farhat WA, Khoury AE, Bagli DJ (2007) Comparative analysis of tubularized incised plate versus onlay island flap urethroplasty for penoscrotal hypospadias. J Urol 178:1451–1457
Xiao D, Nie X, Wang W, Zhou J, Zhang M, Zhou Z et al (2014) Comparison of transverse island flap onlay and tubularized incised-plate urethroplasties for primary proximal hypospadias: a systematic review and meta-analysis. PLoS ONE 9:e106917
Holland AJA, Smith GHH (2000) Effect of the depth and width of the urethral plate on tubularized incised plate urethroplasty. J Urol 164:489
Standoli L (1982) One-stage repair of hypospadias: preputial island flap technique. Ann Plast Surg 9(1):81–88
Snodgrass W (1994) Tubularized, incised plate urethroplasty for distal hypospadias. J Urol 151(2):464–465
Duckett JW; DuckettJW (1981) The island flap technique for hypospadias repair. Urol Clin N Am 8(3):503–511
Turner-Warwick R (1979) Observations upon techniques for reconstruction of the urethral meatus, the hypospadiac glans deformity and the penile urethra. Urol Clin N Am 6(3):643–655
Bracka A (2008) The role of two-stage repair in modern hypospadiology. Indian J Urol 24(2):210–218
Metro MJ, Wu HY, Snyder HM III, Zderic SA, Canning DA (2001) Buccal mucosal grafts: lessons learned from an 8-year experience. J Urol 166(4):1459–1461
Ozgök Y, Ozgür Tan M, Kilciler M, Tahmaz L, Erduran D (2000) Use of bladder mucosal graft for urethral reconstruction. Int J Urol 7(10):355–360
Schnapka J, Mildenberger H (1991) Urethral reconstruction using anautologous bladder mucosal graft. Eur J Pediatr Surg 1(3):180–182
Rushton HG, Belman AB (1998) The split prepuce in situ onlay hypospadias repair. J Urol 160(3 Pt 2):11346
Subramaniam R, Spinoit AF, Hoebeke P (2011) Hypospadias repair: an overview of the actual techniques. Semin Plast Surg 25(3):206–212
Snodgrass WT (2002) Tubularized incised plate (TIP) hypospadias repair. Urol Clin N Am 29(2):285–290
MacGillivray DM, Shankar KR, Rickwood AM (2002) Management of severe hypospadias using Glassberg’s modification of the Duckett repair. BJU Int 89(1):101–102
Valla JS, Takvorian P, Dodat H et al (1991) Single-stage correction of posterior hypospadias (178 cases). Comparison of three techniques: free skin graft, free bladder mucosal graft, transverse pedicle preputial graft. Eur J Pediatr Surg 1(5):287–290
Elbakry A (2001) Management of urethrocutaneous fistula after hypospadias repair: 10 years’ experience. BJU Int 88(6):590–595
Demirbilek S, Kanmaz T, Aydin G, Yücesan S (2001) Outcomes of one-stage techniques for proximal hypospadias repair. Urology 58(2):267–270
Singh BP, Solanki FS, Kapoor R et al (2010) Factors predicting success in hypospadias repair using preputial flap with limited pedicle mobilization (Asopa procedure). Urology 76(1):92–96
Fraumann SA, Stephany HA, Clayton DB, Thomas JC, Adams MC et al (2014) Long-term follow-up of children who underwent severe hypospadias repair using an online survey with validated questionnaires. J Pediatr Urol. 10(3):446–450
Yildiz T, Tahtali IN, Ates Dc, Keles I (2013) age of patient is a risk factor for urethrocutaneous fistula in hypospadias surgery. J Urol 9(6ptA):900–903
Chin TW, Liu CS, Wei CF (2001) Hypospadias repair using a double onlay preputial flap. Pediatr Surg Int 17:496–498
Authors’ contribution
H. Elmoghazy contributed to project development, project preparation, data preparation and collection, manuscript writing and editing. M. M. Hussein contributed to data preparation. Elnisr Mohamed contributed to manuscript editing. A. Badawy contributed to data analysis. Gamal Alsagheer contributed to project preparation. A. M. Abd Elhamed contributed to data preparation, manuscript editing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author guarantees that there is no financial or personal relations with other people or organizations that could influence our work (no conflict of interest).
Ethical standards
Ethics committee approval was obtained.
Rights and permissions
About this article
Cite this article
Elmoghazy, H., Hussein, M.M., Mohamed, E. et al. A novel technique for repair of mid-penile hypospadias using a preputial skin flap: results of 110 patients. Int Urol Nephrol 48, 1943–1949 (2016). https://doi.org/10.1007/s11255-016-1416-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-016-1416-7