Abstract
Introduction
Prolactinomas are the most common functioning pituitary adenomas. Dopamine agonists (DA) are generally very effective in treating prolactinomas by inducing tumor volume regression and endocrine remission. A minority of patients do not respond to DA or are intolerant because of side-effects. Microsurgical resection when possible is the next treatment option, but cavernous sinus, dural, or bone involvement may not allow for complete resection.
Objective
We reviewed the outcome of patients with medically and surgically refractory prolactinomas treated with Gamma Knife radiosurgery (GKRS) during a 22 years follow-up period.
Methods
We reviewed the patient database at the University of Virginia Gamma Knife center during a 25-year period (1989–2014), identifying 38 patients having neurosurgical, radiological and endocrine follow-up.
Results
Median age at GKRS treatment was 43 years. Median follow-up was 42.3 months (range 6–207.9). 55.3 % (n = 21) were taking a dopamine agonist at time of GKRS. 63.2 % (n = 24) had cavernous sinus tumor invasion. Endocrine remission (normal serum prolactin off of a dopamine agonist) was achieved in 50 % (n = 19). GKRS induced hypopituitarism occurred in 30.3 % (n = 10). Cavernous sinus involvement was shown to be a significant negative prognosticator of endocrine remission. Taking a dopamine agonist drug at the time of GKRS showed a tendency to decrease the probability for endocrine remission.
Conclusion
GKRS for refractory prolactinomas can lead to endocrine remission in many patients. Hypopituitarism is the most common side effect of GKRS.


Similar content being viewed by others
References
Mindermann T, Wilson CB (1994) Age-related and gender-related occurrence of pituitary adenomas. Clin Endocrinol 41(3):359–364
Weiss MH, Wycoff RR, Yadley R, Gott P, Feldon S (1983) Bromocriptine treatment of prolactin-secreting tumors: surgical implications. Neurosurgery 12(6):640–642
Wu ZB, Yu CJ, Su ZP, Zhuge QC, Wu JS, Zheng WM (2006) Bromocriptine treatment of invasive giant prolactinomas involving the cavernous sinus: results of a long-term follow up. J Neurosurg 104(1):54–61
Molitch ME (2005) Pharmacologic resistance in prolactinoma patients. Pituitary 8(1):43–52
Molitch ME (2014) Management of medically refractory prolactinoma. J Neurooncol 117(3):421–428
Oh MC, Aghi MK (2011) Dopamine agonist-resistant prolactinomas. J Neurosurg 114(5):1369–1379
Brue T, Pellegrini I et al (1992) Prolactinomas and resistance to dopamine agonists. Horm Res 38(1–2):84–89
Morange I, Barlier A, Pellegrini I et al (1996) Prolactinomas resistant to bromocriptine: long-term efficacy of quinagolide and outcome of pregnancy. Eur J Endocrinol 135(4):413–420
Pellegrini I, Rasolonjanahary R, Gunz G et al (1989) Resistance to bromocriptine in prolactinomas. J Clin Endocrinol Metab 69(3):500–509
Delgrange E, Daems T, Verhelst J et al (2009) Characterization of resistance to the prolactin-lowering effects of cabergoline in macroprolactinomas: a study in 122 patients. Eur J Endocrinol 160(5):747–752
Di Sarno A, Landi ML, Cappabianca P et al (2001) Resistance to cabergoline as compared with bromocriptine in hyperprolactinemia: prevalence, clinical definition, and therapeutic strategy. J Clin Endocrinol Metab 86(11):5256–5261
Oh MC, Kunwar S, Blevins L, Aghi MK (2012) Medical versus surgical management of prolactinomas. Neurosurg Clin N Am 23:669–678
Delgrange E, Duprez T, Maiter D (2006) Influence of parasellar extension of macroprolactinomas defined by magnetic resonance imaging on their responsiveness to dopamine agonist therapy. Clin Endocrinol 64(4):456–462
Liu X, Kano H, Kondziolka D, Park K-J, Iyer A, Niranjan SSA, Flickinger JC, Lunsford LD (2013) Gamma knife stereotactic radiosurgery for drug resistant or intolerant invasive prolactinomas. Pituitary 16:68–75
Casanueva FF, Molitch ME, Schlechte JA, Abs R, Bonert V, Bronstein MD, Brue T, Cappabianca P, Colao A, Fahlbusch R, Fideleff H, Hadani M, Kelly P, Kleinberg D, Laws E, Marek J, Scanlon M, Sobrinho LG, Wass JA, Giustina A (2006) Guidelines of the Pituitary Society for the diagnosis and management of prolactinomas. Clin Endocrinol 65:265–273
Esposito V, Santoro A, Minniti G, Salvati M, Innocenzi G, Lanzetta G, Cantore G (2004) Transsphenoidal adenomectomy for GH-, PRL- and ACTH-secreting pituitary tumours: outcome analysis in a series of 125 patients. Neurol Sci 25:251–256
Santoro A, Minniti G, Ruggeri A, Esposito V, Jaffrain-Rea ML, Delfini R (2007) Biochemical remission and recurrence rate of secreting pituitary adenomas after transsphenoidal adenomectomy: long-term endocrinologic follow-up results. Surg Neurol 68:513–518
Ciric I, Ragin A, Baumgartner C, Pierce D (1997) Complications of transsphenoidal surgery: results of a national survey, review of the literature, and personal experience. Neurosurgery 40(2):225–236 (discussion 236–227)
Pan L, Zhang N, Wang EM, Wang BJ, Dai JZ, Cai PW (2000) Gamma knife radiosurgery as a primary treatment for prolactinomas. J Neurosurg 93(Suppl 3):10–13
Pollock BE, Brown PD, Nippoldt TB, Young WF Jr (2008) Pituitary tumor type affects the chance of biochemical remission after radiosurgery of hormone-secreting pituitary adenomas. Neurosurgery 62(6):1271–1276
Castinetti F, Nagai M, Morange I, Dufour H, Caron P, Chanson P, Cortet-Rudelli C, Kuhn JM, Conte-Devolx B, Regis J, Brue T (2009) Long-term results of stereotactic radiosurgery in secretory pituitary adenomas. J Clin Endocrinol Metab 94(9):3400–3407
Pouratian N, Sheehan J, Jagannathan J, Laws ER Jr, Steiner L, Vance ML (2006) Gamma knife radiosurgery for medically and surgically refractory prolactinomas. Neurosurgery 59(2):255–266 discussion 255-66
Jezkova J, Hana V, Krsek M, Weiss V, Vladyka V, Liscak R, Vymazal J, Pecen L, Marek J (2009) Use of the Leksell gamma knife in the treatment of prolactinoma patients. Clin Endocrinol 70(5):732–741
Kong DS, Lee JI, Lim DH, Kim KW, Shin HJ, Nam DH, Park K, Kim JH (2007) The efficacy of fractionated radiotherapy and stereotactic radiosurgery for pituitary adenomas: long-term results of 125 consecutive patients treated in a single institution. Cancer 110:854–860
Landolt AM, Haller D, Lomax N, Scheib S, Schubiger O, Siegfried J, Wellis G (1998) Stereotactic radiosurgery for recurrent surgically treated acromegaly: comparison with fractionated radiotherapy. J Neurosurg 88:1002–1008
Breen P, Flickinger JC, Kondziolka D, Martinez AJ (1998) Radiotherapy for nonfunctional pituitary adenoma: analysis of long-term tumor control. J Neurosurg 89:933–938
Minniti G, Traish D, Ashley S, Gonsalves A, Brada M (2005) Risk of second brain tumor after conservative surgery and radiotherapy for pituitary adenoma: update after an additional 10 years. J Clin Endocrinol Metab 90:800–804
Rowe J, Grainger A, Walton L, Silcocks P, Radatz M, Kemeny A (2007) Risk of malignancy after gamma knife stereotactic radiosurgery. Neurosurgery 60:60–65 [discussion 65-6]
Swords FM, Monson JP, Besser GM, Chew SL, Drake WM, Grossman AB, Plowman PN (2009) Gamma knife radiosurgery: a safe and effective salvage treatment for pituitary tumours not controlled despite conventional radiotherapy. Eur J Endocrinol 161(6):819–828
Kuo JS, Chen JC, Yu C, Zelman V, Giannotta SL, Petrovich Z, MacPherson D, Apuzzo ML (2004) Gamma knife radiosurgery for benign cavernous sinus tumors: quantitative analysis of treatment outcomes. Neurosurgery 54(6):1385–1393 (discussion 1393–1384)
Pamir MN, Kilic T, Belirgen M, Abacioglu U, Karabekiroglu N (2007) Pituitary adenomas treated with gamma knife radiosurgery: volumetric analysis of 100 cases with minimum 3 year follow-up. Neurosurgery 61(2):270–280
Lee C-C, Chen C-J, Yen C-P, Zhiyuan X, Schlesinger D, Fezeu F, Sheehan JP (2014) Whole-sellar stereotactic radiosurgery for functioning pituitary adenomas. Neurosurgery 75(3):227–237 discussion 237
Hamilton DK, Vance ML, Boulos PT, Laws ER Jr (2005) Surgical outcomes in hyporesponsive prolactinomas: analysis of patients with resistance or intolerance to dopamine agonists. Pituitary 8:53–60
Yen CP, Sheehan JP, Schwyzer L, Schlesinger D (2011) Hemorrhage risk of cerebral arteriovenous malformations before and during the latency period after Gamma knife radiosurgery. Stroke 42:1691–1696
Snell JW, Sheehan J, Stroila M, Steiner L (2006) Assessment of imaging studies used with radiosurgery: a volumetric algorithm and an estimation of its error. Technical note. J Neurosurg 104(1):157–162
Mayo C, Martel MK, Marks LB, Flickinger J, Nam J, Kirkpatrick J (2010) Radiation dose–volume effects of optic nerves and chiasm. Int J Radiat Oncol Biol Phys 76(Suppl 3):S28–S35
Lee CC, Chen CJ, Yen CP, Xu Z, Schlesinger D, Fezeu F, Sheehan JP (2014) Whole-sellar stereotactic radiosurgery for functioning pituitary adenomas. Neurosurgery 75(3):227–237
Ma W, Ikeda H, Yoshimoto T (2002) Clinicopathologic study of 123 cases of prolactin-secreting pituitary adenomas with special reference to multihormone production and clonality of the adenomas. Cancer 95(2):258–266
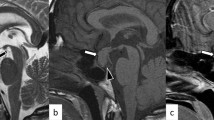
Cottier JP, Destrieux C, Brunereau L, Bertrand P, Moreau L, Jan M, Herbreteau D (2000) Cavernous sinus invasion by pituitary adenoma: MR imaging. Radiology 215(2):463–469
Knosp E, Steiner E, Kitz K, Matula C (1993) Pituitary adenomas with invasion of the cavernous sinus space: a magnetic resonance imaging classification compared with surgical findings. Neurosurgery 33(4):610–617 (discussion 617–618)
Delgrange E, Sassolas G, Perrin G, Jan M, Trouillas J (2005) Clinical and histological correlations in prolactinomas, with special reference to bromocriptine resistance. Acta Neurochirur 147(7):751–757
Dallabonzana D, Liuzzi A, Oppizzi G et al (1986) Chronic treatment of pathological hyperprolactinemia and acromegaly with the new ergot derivate teguride. J Clin Endocrinol Metab 63:1002–1007
Johnston DG, Prescott RV, Kendall-Taylor P et al (1983) Hyperprolactinemia. Long-term effects of bromocriptine. Am J Med 75:868–874
Moriondo P, Travaglini P, Nissim M et al (1985) Bromocriptine treatment of microprolactinomas: evidence of stable prolactin decrease after drug withdrawal. J Clin Endocrinol Metab 60:764–772
Webster J, Piscitelli G, Polli A et al (1994) A comparison of cabergoline and bromocriptine in the treatment of hyper-prolactinemic amenorrhea. Cabergoline comparative study group. N Engl J Med 331:904–909
Muratori M, Arosio M, Gambino G et al (1997) Use of cabergoline in the long-treatment of hyperprolactinemic and acromegalic patients. J Endocrinol Invest 20:537–546
Cannavo S, Curto L, Squadrito S et al (1999) Cabergoline: a first-choice treatment in patients with previously untreated prolactin-secreting pituitary adenoma. J Endocrinol Invest 22:354–359
Ferrari C, Paracchi A, Mattei AM et al (1992) Cabergoline in the long-term therapy of hyperprolactinemic disorders. Acta Endocrinol 126:489–494
Colao A, Di Sarno A, Landi ML et al (2000) Macroprolactinoma shrinkage during cabergoline treatment is greater in naive patients than in patients pretreated with other dopamine agonists: a prospective study in 110 patients. J Clin Endocrinol Metab 85:2247–2252
Sheehan JP, Pouratian N, Steiner L, Laws ER, Vance ML (2011) Gamma knife surgery for pituitary adenomas: factors related to radiological and endocrine outcomes. J Neurosurg 114(2):303–309
Landolt AM, Lomax N (2000) Gamma knife radiosurgery for prolactinomas. J Neurosurg 93(Suppl 3):14–18
Tanaka S, Link MJ, Brown PD, Stafford SL, Young WF Jr, Pollock BE (2010) Gamma knife radiosurgery for patients with prolactin-secreting pituitary adenomas. World Neurosurg 74(1):147–152
Kim M, Paeng S, Pyo S, Jeong Y, Lee S, Jung Y (2006) Gamma knife surgery for invasive pituitary macroadenoma. J Neurosurg 105(Suppl):26–30
Castinetti F, Taieb D, Kuhn JM, Chanson P, Tamura M, Jaquet P, Conte-Devolx B, Regis J, Dufour H, Brue T (2005) Outcome of gamma knife radiosurgery in 82 patients with acromegaly: correlation with initial hypersecretion. J Clin Endocrinol Metab 90(8):4483–4488
Pollock BE, Jacob JT, Brown PD, Nippoldt TB (2007) Radiosurgery of growth hormone-Producing pituitary adenomas: factors associated with biochemical remission. J Neurosurg 106(5):833–838
Jagannathan J, Sheehan JP, Pouratian N, Laws ER Jr, Steiner L, Vance ML Jr (2008) Gamma knife radiosurgery for acromegaly: outcomes after failed transsphenoidal surgery. Neurosurgery 62:1262–1269
Landolt AM, Haller D, Lomax N, Scheib S, Schubiger O, Siegfried J, Wellis G (2000) Octreotide may act as a radioprotective agent in acromegaly. J Clin Endocrinol Metab 85(3):1287–1289
Pouratian N, Sheehan J, Jagannathan J, Laws ER Jr, Steiner L, Vance ML (2006) Gamma knife radiosurgery for medically and surgically refractory prolactinomas. Neurosurgery 59(2):255–266
Pollock BE, Nippoldt TB, Stafford SL, Foote RL, Abboud CF (2002) Results of stereotactic radiosurgery in patients with hormone-producing pituitary adenomas: factors associated with endocrine normalization. J Neurosurg 97:525–530
Attanasio R, Epaminonda P, Motti E, Giugni E, Ventrella L, Cozzi R, Farabola M, Loli P, Beck-Peccoz P, Arosio M (2003) Gamma-knife radiosurgery in acromegaly: a 4-year follow-up study. J Clin Endocrinol Metab 88(7):3105–3112
Girkin CA, Comey CH, Lunsford LD, Goodman ML, Kline LB (1997) Radiation optic neuropathy after stereotactic radiosurgery. Ophthalmology 104:1634–1643
Laws ER Jr, Vance ML (1999) Radiosurgery for pituitary tumors and cranipharyngiomas. Neurosurg Clin N Am 72(Suppl 1):119–124
Leber KA, Bergloff J, Pendl G (1998) Dose-response tolerance of the visual pathways and cranial nerves of the cavernous sinus to stereotactic radiosurgery. J Neurosurg 88:43–50
Ove R, Kelman S, Amin PP, Chin LS (2000) Preservation of visual fields after peri-sellar gamma-knife radiosurgery. Int J Cancer 90:343–350
Tishler RB, Loeffler JS, Lunsford LD, Duma C, Alexander E 3rd, Kooy HM, Flickinger JC (1993) Tolerance of cranial nerves of the cavernous sinus to radiosurgery. Int J Radiat Oncol Biol Phys 27:215–221
Acknowledgments
Multiple clinicians have contributed to this radiosurgery experience. We would like to thank Drs. Edward Laws, Edward H. Oldfield, John Jane Jr., Michael Thorner, John Marshall, and Gregory Hong and referring physicians for their efforts in the treatment and follow up of these patients.
Conflict of interest
The authors have no personal or institutional financial interest in drugs or materials in relation to this paper.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cohen-Inbar, O., Xu, Z., Schlesinger, D. et al. Gamma Knife radiosurgery for medically and surgically refractory prolactinomas: long-term results. Pituitary 18, 820–830 (2015). https://doi.org/10.1007/s11102-015-0658-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11102-015-0658-1