Abstract
Chromosomal instability is a hallmark of human cancers and is closely linked to tumorigenesis. The prognostic value of molecular signatures of chromosomal instability (CIN) has been validated in various cancers. However, few studies have examined the relationship between CIN and glioma. Histone deacetylases (HDACs) regulate chromosome structure and are linked to the loss of genomic integrity in cancer cells. In this study, the prognostic value of HDAC4 expression and its association with markers of CIN were investigated by analyzing data from our own and four other large sample databases. The results showed that HDAC4 expression is downregulated in high- as compared to low-grade glioma and is associated with a favorable clinical outcome. HDAC4 expression and CIN were closely related in glioma from both functional and statistical standpoints. Moreover, the predictive value of the O-6-methylguanine-DNA methyltransferase (MGMT) promoter methylation status—a widely used glioma marker—was refined by HDAC4 expression level, which was significantly related to CIN in our study. In conclusion, we propose that HDAC4 expression, a prognostic and CIN marker, enhances the predictive value of MGMT promoter methylation status for identifying patients who will most benefit from radiochemotherapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Glioma is the most common type of primary central nervous system (CNS) tumor and a leading cause of tumor-related mortality. Despite major advances in therapy over the past decades, the clinical outcome for most patients remains poor. This is especially true for glioblastoma (GBM), the most malignant grade of glioma, which has a median survival of 14.6 months and a 2-year survival rate of 5–10 % even after aggressive therapy [1]. As a major form of genomic instability, chromosomal instability (CIN) is a critical event in early stages of tumorigenesis and, when compounded, leads to the transformation of normal cells into cancer cells [2]. Various types of CIN have been detected in glioma, including mutations, loss of heterozygosity, and copy number aberrations [3–6]. Several studies have reported that CIN can affect sensitivity to chemotherapy and consequently the prognosis of glioma patients [7, 8].
A close association between CIN and histone acetylation has been demonstrated [9–11]. Central to histone acetylation are histone deacetylases (HDACs), which maintain genomic integrity by targeting histone and non-histone proteins and thereby regulating DNA repair mechanisms [12]. A total of 18 human HDACs, classified into four groups, have been identified. As a member of group II HDACs, HDAC4 is closely linked to many disease processes—including cancer, leukemia, diabetes, infection, and cardiac disease [13–18]—and is also highly expressed in the brain where it plays an important role in brain functioning [19–22].
Epigenetic silencing of the O-6-methylguanine-DNA methyltransferase (MGMT) gene by promoter methylation is associated with prolonged survival and sensitivity to chemotherapeutic alkylating agents in GBM patients undergoing standard treatment [23, 24]. The beneficial effects of combined radiochemotherapy vary significantly between GBM patients, even for those with a methylated MGMT promoter [25]. This suggests that while important, MGMT promoter methylation is not the sole factor determining clinical outcome, and highlights the need for evaluating patients based on other factors; for instance, CIN combined with MGMT promoter methylation status may provide more accurate information for predicting disease outcome.
CIN is defined as the gain or loss of whole or fractions of chromosomes, and is associated with tumorigenesis, disease prognosis, and acquisition of multi-drug resistance in various cancers, including breast cancer, melanoma, and lymphoma [26–32]. High throughput gene expression profiling approaches have established a reasonable link between the expression of specific genes and the degree of CIN in multiple cancers. Carter et al. developed computational methods to measure the “CIN score” for 10,151 genes, which indicates the correlation between each gene and the CIN degree in tumor samples [30]. Based on the “CIN score”, the top ranked genes are chosen for forming the CIN signature, which was represented by CIN25 score (Further backgrounds of CIN signature and CIN25 score are shown in the Supplementary Text) [30]. The CIN signature, comprising a specific set of genes that are critical for maintaining genomic integrity, is significantly higher in metastatic foci, and stratifies patients according to clinical outcome in various cancers, suggesting that these genes are responsible for a more aggressive cancer phenotype [30, 33]. However, as it consists of multiple genes, the CIN signature is too complex to be suitable for routine clinical application. The present study investigated whether HDAC4 expression can serve as an alternative marker for assessing the degree of CIN and, in combination with MGMT promoter status, predict the outcome of patients.
Materials and methods
Patients and samples
A total of 539 glioma specimens from the Chinese Glioma Genome Atlas (CGGA) that were contiguously collected at multiple centers were used in this study. Tumor tissue samples were obtained by surgical resection prior to radio and/or chemotherapy, flash-frozen in liquid nitrogen, and stored at −80 °C until nucleic acid extraction. The study protocol was approved by the ethics committees of participating hospitals. Each sample was diagnosed and independently confirmed histopathologically at the Department of Pathology according to the 2007 WHO classification system of CNS tumors by two experienced neuropathologists. Clinical data, including age, sex, preoperative KPS score, adjuvant radiation and chemotherapy, and the recorded date of disease progression or death were obtained from medical records.
Data on mRNA expression were obtained by whole transcriptome sequencing (N = 325) and whole-genome mRNA expression microarray (N = 299) from the CGGA, and the following four datasets were used for validation: the Cancer Genome Atlas (http://cancergenome.nih.gov); Repository for Molecular Brain Neoplasis Data (REMBRANDT, http://caintegrator.nci.nih.gov/rembrandt); GSE16011 (http://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE16011); and GSE4290 (http://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE4290).
Evaluation of MGMT promoter methylation by DNA pyrosequencing
MGMT promoter methylation status was detected by DNA pyrosequencing as previously described [34, 35]. Bisulfite DNA modification was performed using the EpiTect Kit (Qiagen). The following primers were used to amplify the MGMT promoter region: 5′-GTTTYGGATATGTTGGGATA-3′ (forward) and 5′-biotin-ACCCAAACACTCACCAAATC-3′ (reverse). The PCR analysis was performed in duplicate in a 40-μl reaction volume containing 0.5 μl each primer (using a 10-μM working solution), 4 μl 10 × buffer, 3.2 μl of 2.5 μM dNTP, 2.5 U hotstart Taq (Takara Bio, Madison, WI, USA), and 2 μl of 10 μM bisulphite-treated DNA. The reaction conditions were: 95 °C for 3 min; 40 cycles of 95 °C for 15 s, 52 °C for 30 s, and 72 °C for 30 s; and 72 °C for 5 min (ABI 9700; Applied Biosystems, Foster City, CA, USA). DNA was purified from total PCR products using QIAamp DNA Mini Kit (Qiagen, Valencia, CA, USA) and subjected to pyrosequencing (PyroMark Q96 ID System; Qiagen) using the primer 5′-GGATATGTTGGGATAGT-3′ in accordance with the manufacturer’s instructions. The obtained methylation values were averaged across the seven tested CpG loci within the MGMT promoter. Samples were considered as having a methylated MGMT promoter if the average methylation was ≥10 %.
Survival analysis
To assess the prognostic value of HDAC4 expression in glioma, a survival analysis for each tumor grade was performed based on expression level. The combined effect of MGMT promoter methylation status and HDAC4 expression was then assessed in GBM. Patients receiving radiochemotherapy were stratified into two groups according to MGMT status, and further classified into four subgroups based on HDAC4 expression level; the statistical significance was determined by the log-rank test.
CIN25 score based on 25 genes was calculated as the sum of the expression levels of each signature gene in a patient [30]. Dichotomization was performed for each tumor grade to classify patients into two groups based on the median signature score. Patients who received radiochemotherapy were then stratified into four subgroups based on MGMT status and CIN25 score to study the combined effect of these parameters in GBM, and a survival analysis was carried out.
Gene ontology (GO) analysis and gene set enrichment analysis (GSEA)
A Pearson correlation analysis was performed across glioma grades to identify genes that are significantly related to HDAC4. GO analysis was performed using the DAVID (http://david.abcc.ncifcrf.gov/home.jsp) [36]. To obtain more information about the relationship between CIN25 score and HDAC4, GSEA (http://www.broadinstitute.org/gsea/index.jsp) was performed as previously described to determine whether the identified set of genes showed statistically significant differences between the two biological states [37].
Statistical analysis
SPSS software and GraphPad Prism 6 were used for statistical analyses. The differences in HDAC4 expression and CIN25 score between groups were compared using Student’s t and χ2 tests. A dichotomization based on the median HDAC4 expression level and CIN25 score was carried out for the survival analysis. Overall survival (OS) was calculated from the date of diagnosis until death or the end of follow-up. Progression-free survival (PFS) was defined as the time between the diagnosis and the first unequivocal clinical or radiological sign of disease progress. Kaplan–Meier survival analyses for OS and PFS were performed and compared with the log-rank test. A Pearson correlation analysis was used to test the correlation between CIN25 score and HDAC4 expression. Statistical significance was defined as a two-tailed P value < 0.05.
Results
HDAC4 expression is significantly associated with progressive malignancy in glioma
To test the relationship between HDAC4 expression and tumor grade, patients were stratified into low or high expression groups according to the median value for HDAC4 expression in each database. The percentage of samples with low expression increased with progressive malignancy (P < 0.001; χ2 test) (Table S1). This correlation between HDAC4 expression and tumor grade was studied in CGGA and three validation sets (Fig. 1a–d) showing that HDAC4 expression differed among various grades and was downregulated for higher grades. Based on these results, we propose that low HDAC4 expression is a characteristic of high-grade glioma.
Highly expressed HDAC4 prolongs survival and strengthens the predictive value of MGMT promoter methylation
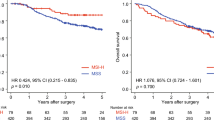
To evaluate the prognostic value of HDAC4 expression in glioma, dichotomization was applied in every grade to separate samples into two groups based on HDAC4 expression level. Kaplan–Meier survival curves in CGGA and three validation sets showed that HDAC4 overexpression conferred longer OS (Fig. 2a–j) and PFS (Fig. S1a–c) in each grade. When both radiochemotherapy and MGMT promoter methylation status were considered, 55 GBM patients were included in the assessment of the prognostic value of HDAC4 expression combined with MGMT promoter methylation status. Patients were assigned to four subgroups according to their MGMT status and HDAC4 expression level, as described above. Notably, OS varied significantly among the four subgroups (P = 0.027; Fig. 2k). Among patients with a methylated MGMT promoter, those with higher HDAC4 expression had a median OS of 669 days, which was significantly longer than that of patients with low HDAC4 expression or with a non-methylated MGMT promoter (Fig. 2k). There were no other differences among the three subgroups. A similar analysis was carried out in GBM patients who had received standard radiation combined chemotherapy in the TCGA database, and the results confirmed that patients with MGMT promoter methylation and high HDAC4 expression had a significantly longer OS than other patients (Fig. 2l).
Higher HDAC4 expression is associated with longer OS in the CGGA, REMBRANDT, GSE16011, and TCGA databases (a–j). Survival analysis according to MGMT promoter status combined with HDAC4 expression was performed with data from the CGGA (k) and TCGA (l). Patients whose tumors had a methylated MGMT promoter and a higher expression of HDAC4 had the best prognosis
HDAC4 expression is closely correlated with chromatin structure
A Pearson correlation analysis was conducted to identify genes whose expression is correlated with that of HDAC4. A total of 4,794 genes were significantly correlated (3,262 genes with R < − 0.3 and 1,532 genes with R > 0.3; P < 0.001). Positively correlated genes with a P value < 1e−10 were used for the GO analysis, which revealed ten processes mostly related to chromatin organization and histone modification. These results confirm that HDAC4 is critical for regulating chromosome structure (Table 1).
A high CIN25 score is associated with progressive malignancy, poor prognosis, and chemotherapy resistance in glioma
The CIN25 score was used as a marker of CIN. Based on the median score across tumor grades, patients were stratified into low and high score groups. Patients with high scores has greater representation among higher tumor grades (P < 0.001; χ2 test) (Table S2). Analysis of data from the CGGA and two validation databases (Student’s t test) (Fig. 3a–c) showed that CIN25 scores increased as a function of glioma grade and was highest in the most malignant GBM, indicating that CIN is tightly associated with glioma progression.
Correlation between CIN25 score and glioma malignancy. CIN, as measured by the CIN25 score, was analyzed with respect to tumor grade (II–IV) in the CGGA (a) and two validation sets (b, c). A high CIN25 score was associated with shorter OS (d–f) in the CGGA. A survival analysis for MGMT promoter status combined with CIN25 score was performed in the CGGA (g). Sensitivity to chemotherapy was assessed in GBM patients. Patients with a low CIN25 score receiving radiochemotherapy had better OS than those receiving radiotherapy alone (h); no differences between treatment groups were observed among patients with a high CIN25 score (i)
The prognostic value of the CIN25 score in glioma was next evaluated across three independent databases. The OS and PFS showed a notable reduction for patients with a high as compared to a low CIN25 score (Fig. 3d–f, Fig. S2, S3). In 52 GBM patients who received post-operative radiochemotherapy, MGMT promoter methylation status and CIN25 score were incorporated into the stratification; in this case, the OS differed significantly among subgroups (P = 0.025; Fig. 3g). Patients with MGMT promoter methylation and lower CIN25 score had a longer OS than the other three subgroups. A significant difference in clinical outcome was detected in the MGMT promoter methylation group, demonstrating that a low CIN25 score was associated with better prognosis than a high CIN25 score (P = 0.046; Fig. 3g). When the relationship between CIN25 score and response to chemotherapy in GBM was analyzed, patients with a lower CIN25 score who received radiochemotherapy had longer survival times than those who received radiotherapy alone (P < 0.001, Fig. 3h). However, there was no difference between these two treatment conditions among patients with high CIN25 scores (Fig. 3i), suggesting that the poor prognosis observed in these patients may be due to the acquisition of chemotherapy resistance.
CIN signature is strongly associated with HDAC4 expression in glioma
A correlation analysis revealed that HDAC4 expression was significantly correlated with CIN25 score (Fig. 4a, P < 0.001, R = − 0.366), which was confirmed by data from the REMBRANDT and GSE16011 datasets (P < 0.001, R = − 0.461 and P < 0.001, R = − 0.309, respectively; Fig. 4b, c). This suggests a significant relationship between HDAC4 expression and CIN in glioma. The GSEA was used to test whether HDAC4 expression is correlated with genes contributing to the CIN25 score. Samples were listed in order of increasing HDAC4 expression. The results indicate that CIN25 genes were significantly enriched in samples with low HDAC4 expression, whereas high HDAC4 expression was not correlated with any of these genes (NES = 1.5306281, P = 0.027; Fig. 4d).
Association between HDAC4 expression and CIN25 in glioma. HDAC4 expression level was closely correlated with CIN25 score in the CGGA (a) and other validation sets (b, c). The GSEA showed that CIN25 genes were significantly enriched in samples with low HDAC4 expression (d). The horizontal bar in graded color from red to blue represents the rank ordering of patients based on increasing HDAC4 expression. The vertical black lines represent the projection of individual genes constituting the CIN25 score. Genes on the left (red) correlated most strongly with downregulated HDAC4 expression. NES normalized enrichment score
Discussion
The high prevalence, mortality, and risk of post-treatment complications associated with glioma make it one of most challenging diseases affecting humans. Moreover, patients with the same diagnosis may experience vastly different clinical outcomes even after undergoing the same treatment. This heterogeneity highlights the limitations of a grading system based purely on pathological characterization. As a feature of most human cancers, CIN—which has a high degree of heterogeneity among tumor cells and involves a complex network of molecular interactions rather than a single signaling pathway [38]—may better reflect glioma severity and offer a more accurate measure for predicting disease prognosis.
HDACs are the main regulators of histone acetylation, which has been implicated in CIN. As a member of group II HDACs, HDAC4 is highly expressed in the brain and involved in various functions including learning and memory, behavior, and neuronal survival [19–21, 39, 40]. We propose that HDAC4 expression is closely associated with glioma grade and prognosis, with a lower HDAC4 expression significantly associated with progressive malignancy and unfavorable disease outcome, similar to what is observed in other cancers [41]. The GO analysis indicated that HDAC4 expression is functionally related to the maintenance of chromosome structure. Meanwhile, several previous studies have demonstrated various roles for HDAC4 in cancer cells. In chondrosarcoma, a decrease in HDAC4 expression leads to the upregulation of vascular endothelial growth factor expression, thereby stimulating angiogenesis [42]; in prostate cancer cells, HDAC4 downregulation was associated with a high level of androgen receptor expression, which promoted cell growth [43]. The results of the present study reveal that HDAC4 is a strong prognostic factor in glioma and likely determines patient outcome via modulation of genomic integrity.
The most widely used marker of genomic instability is the CIN signature, which embodies aberrations in chromosome number as well as structure [44]. There was considerable overlap in the CIN25 score across tumor grades, and patients with the same grade had significantly different CIN25 scores. The overlap between grades was normalized by restricting the analysis of CIN25 score to each grade in the glioma databases; as in the case of other cancers, a higher score was linked to high pathological grade and unfavorable prognosis, confirming that a loss of genomic integrity plays an important role in tumorigenesis and impacts patient prognosis. The strongly negative correlation between HDAC4 expression and CIN which determined by statistical analyses of GO results and by GSEA confirmed the utility of HDAC4 as a more convenient, alternative marker of genomic instability.
Previous studies have reported that cancer cells with a high degree of CIN acquire multi-drug resistance at higher rates as compared to diploid cells with stable chromosomes. This is true in the case of colorectal cancer, regardless of somatic mutation status [45]. A similar relationship to drug sensitivity was found in soft tissue sarcoma and ovarian cancer [32, 46]. In this study, GBM patients with a low CIN25 score were more sensitive to radiochemotherapy and lived longer than those receiving radiotherapy alone, but there were no differences observed between the two treatment groups for patients with a high CIN25 score. The relationship between CIN and multi-drug resistance can be explained by the increased heterogeneity in malignant cancers resulting from CIN, which increases the probability of a drug-resistant subclone arising in the tumor [47].
Combined radiochemotherapy, rather than radiotherapy or chemotherapy alone, is a standard treatment for GBM. MGMT promoter methylation status is a clinical predictor of the extent to which GBM patients will benefit from chemotherapy [25]. Several studies have shown that MGMT deficiency resulting from MGMT promoter methylation may confer increased sensitivity to alkylating agents, yet some glioma patients with MGMT promoter methylation still exhibit resistance to these drugs [25, 48]. Thus, evaluating genomic integrity in combination with MGMT promoter methylation status may provide additional insight into the mechanism underlying the acquisition of drug resistance [49]. The current analysis of GBM patients with MGMT promoter methylation receiving combined radiochemotherapy revealed that survival was prolonged in patients with a low CIN25 score (indicating a more stable genome) than those with a high score; in the latter group, the poor outcome was likely due in part to chemotherapy resistance arising from increased CIN. These results indicate that the sensitivity to chemotherapy conferred by MGMT methylation depends on a stable genome, and that the degree of genomic instability further stratifies patients with MGMT methylation. The CIN25 score encompasses the status of 25 different genes, and as such, is difficult to incorporate into routine clinical practice as a diagnostic tool. Based on the strong association between HDAC4 expression and CIN, we examined whether the combination of MGMT promoter methylation status and HDAC4 expression level could instead be used to predict patient outcome. Interestingly, for the highly malignant GBM, combined radiochemotherapy had the greatest benefit for patients with MGMT promoter methylation and high HDAC4 expression (indicating a lesser degree of CIN). Thus, these two factors combined can identify patients with the best prognosis who are suitable candidates for more aggressive therapy, even the underlying mechanisms needed further experimental methods for interpretation.
Such an analysis helped us gain a novel perspective for understanding the chemotherapy resistance in GBM patients. The mechanisms of chemotherapy resistance resulted from CIN needed further experimental methods for interpretation. In addition, whether the CIN degree was a determining factor in gliomagenesis of different subtypes and further tightly associated with the appearance of MGMT promoter methylation in GBM patients were pertinent questions as well. With immunohistochemistry being widely used in both routine clinical practice and research, the role of HDAC4 in glioma could be further validated from protein level in the near future. Clinically, our next major goal is to verify its role in the guidance of glioma diagnosis and treatment.
In conclusion, in present study, HDAC4 expression was found to be closely related to tumor grade and patient prognosis, and functional and statistical analyses identified a correlation between HDAC4 expression and CIN signature in glioma. Taken together, the results indicate that HDAC4 can serve as a marker of CIN and, when combined with MGMT promoter methylation status, may be used to identify GBM patients who would benefit most from combined radiochemotherapy.
References
Stupp R, Mason WP, Van den Bent MJ, Weller M, Fisher B, Taphoorn MJ, Belanger K, Brandes AA, Marosi C, Bogdahn U, Curschmann J, Janzer RC, Ludwin SK, Gorlia T, Allgeier A, Lacombe D, Cairncross JG, Eisenhauer E, Mirimanoff RO, European Organisation for R, Treatment of Cancer Brain T, Radiotherapy G, National Cancer Institute of Canada Clinical Trials G (2005) Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med 352:987–996. doi:10.1056/NEJMoa043330
Loeb LA (1991) Mutator phenotype may be required for multistage carcinogenesis. Cancer Res 51:3075–3079
Ichimura K, Pearson DM, Kocialkowski S, Backlund LM, Chan R, Jones DT, Collins VP (2009) IDH1 mutations are present in the majority of common adult gliomas but rare in primary glioblastomas. Neuro-oncology 11:341–347. doi:10.1215/15228517-2009-025
Cai J, Yang P, Zhang C, Zhang W, Liu Y, Bao Z, Liu X, Du W, Wang H, Jiang T, Jiang C (2014) ATRX mRNA expression combined with IDH1/2 mutational status and Ki-67 expression refines the molecular classification of astrocytic tumors: evidence from the whole transcriptome sequencing of 169 samples samples. Oncotarget 5:2551–2561
Research Cancer Genome Atlas, N, (2008) Comprehensive genomic characterization defines human glioblastoma genes and core pathways. Nature 455:1061–1068. doi:10.1038/nature07385
Yan H, Parsons DW, Jin G, McLendon R, Rasheed BA, Yuan W, Kos I, Batinic-Haberle I, Jones S, Riggins GJ, Friedman H, Friedman A, Reardon D, Herndon J, Kinzler KW, Velculescu VE, Vogelstein B, Bigner DD (2009) IDH1 and IDH2 mutations in gliomas. N Engl J Med 360:765–773. doi:10.1056/NEJMoa0808710
Cairncross JG, Ueki K, Zlatescu MC, Lisle DK, Finkelstein DM, Hammond RR, Silver JS, Stark PC, Macdonald DR, Ino Y, Ramsay DA, Louis DN (1998) Specific genetic predictors of chemotherapeutic response and survival in patients with anaplastic oligodendrogliomas. J Natl Cancer Inst 90:1473–1479
Smith JS, Perry A, Borell TJ, Lee HK, O’Fallon J, Hosek SM, Kimmel D, Yates A, Burger PC, Scheithauer BW, Jenkins RB (2000) Alterations of chromosome arms 1p and 19q as predictors of survival in oligodendrogliomas, astrocytomas, and mixed oligoastrocytomas. J Clin Oncol 18:636–645
Nagarajan P, Ge Z, Sirbu B, Doughty C, Agudelo Garcia PA, Schlederer M, Annunziato AT, Cortez D, Kenner L, Parthun MR (2013) Histone acetyl transferase 1 is essential for mammalian development, genome stability, and the processing of newly synthesized histones H3 and H4. PLoS Genet 9:e1003518. doi:10.1371/journal.pgen.1003518
Thompson LL, Guppy BJ, Sawchuk L, Davie JR, McManus KJ (2013) Regulation of chromatin structure via histone post-translational modification and the link to carcinogenesis. Cancer Metastasis Rev 32:363–376. doi:10.1007/s10555-013-9434-8
Dovey OM, Foster CT, Conte N, Edwards SA, Edwards JM, Singh R, Vassiliou G, Bradley A, Cowley SM (2013) Histone deacetylase 1 and 2 are essential for normal T-cell development and genomic stability in mice. Blood 121:1335–1344. doi:10.1182/blood-2012-07-441949
Lahue RS, Frizzell A (2012) Histone deacetylase complexes as caretakers of genome stability. Epigenetics 7:806–810. doi:10.4161/epi.20922
Stronach EA, Alfraidi A, Rama N, Datler C, Studd JB, Agarwal R, Guney TG, Gourley C, Hennessy BT, Mills GB, Mai A, Brown R, Dina R, Gabra H (2011) HDAC4-regulated STAT1 activation mediates platinum resistance in ovarian cancer. Cancer Res 71:4412–4422. doi:10.1158/0008-5472.CAN-10-4111
Isaacs JT, Antony L, Dalrymple SL, Brennen WN, Gerber S, Hammers H, Wissing M, Kachhap S, Luo J, Xing L, Bjork P, Olsson A, Bjork A, Leanderson T (2013) Tasquinimod is an allosteric modulator of HDAC4 survival signaling within the compromised cancer microenvironment. Cancer Res 73:1386–1399. doi:10.1158/0008-5472.CAN-12-2730
Gruhn B, Naumann T, Gruner D, Walther M, Wittig S, Becker S, Beck JF, Sonnemann J (2013) The expression of histone deacetylase 4 is associated with prednisone poor-response in childhood acute lymphoblastic leukemia. Leuk Res 37:1200–1207. doi:10.1016/j.leukres.2013.07.016
Lenoir O, Flosseau K, Ma FX, Blondeau B, Mai A, Bassel-Duby R, Ravassard P, Olson EN, Haumaitre C, Scharfmann R (2011) Specific control of pancreatic endocrine beta- and delta-cell mass by class IIa histone deacetylases HDAC4, HDAC5, and HDAC9. Diabetes 60:2861–2871. doi:10.2337/db11-0440
Goodwin MM, Molleston JM, Canny S, Abou El Hassan M, Willert EK, Bremner R, Virgin HW (2010) Histone deacetylases and the nuclear receptor corepressor regulate lytic-latent switch gene 50 in murine gammaherpesvirus 68-infected macrophages. J Virol 84:12039–12047. doi:10.1128/JVI.00396-10
Usui T, Morita T, Okada M, Yamawaki H (2014) Histone deacetylase 4 controls neointimal hyperplasia via stimulating proliferation and migration of vascular smooth muscle cells. Hypertension 63:397–403. doi:10.1161/HYPERTENSIONAHA.113.01843
Darcy MJ, Calvin K, Cavnar K, Ouimet CC (2010) Regional and subcellular distribution of HDAC4 in mouse brain. J Comp Neurol 518:722–740. doi:10.1002/cne.22241
Kim MS, Akhtar MW, Adachi M, Mahgoub M, Bassel-Duby R, Kavalali ET, Olson EN, Monteggia LM (2012) An essential role for histone deacetylase 4 in synaptic plasticity and memory formation. J Neurosci 32:10879–10886. doi:10.1523/JNEUROSCI.2089-12.2012
Haberland M, Montgomery RL, Olson EN (2009) The many roles of histone deacetylases in development and physiology: implications for disease and therapy. Nat Rev Genet 10:32–42. doi:10.1038/nrg2485
Bao ZS, Li MY, Wang JY, Zhang CB, Wang HJ, Yan W, Liu YW, Zhang W, Chen L, Jiang T (2014) Prognostic value of a nine-gene signature in glioma patients based on mRNA expression profiling. CNS Neurosci Ther 20:112–118. doi:10.1111/cns.12171
Wen PY, Kesari S (2008) Malignant gliomas in adults. N Engl J Med 359:492–507. doi:10.1056/NEJMra0708126
Stupp R, Brada M, van den Bent MJ, Tonn JC, Pentheroudakis G, on behalf of the EGWG (2014) High-grade glioma: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. doi:10.1093/annonc/mdu050
Hegi ME, Diserens AC, Gorlia T, Hamou MF, de Tribolet N, Weller M, Kros JM, Hainfellner JA, Mason W, Mariani L, Bromberg JE, Hau P, Mirimanoff RO, Cairncross JG, Janzer RC, Stupp R (2005) MGMT gene silencing and benefit from temozolomide in glioblastoma. N Engl J Med 352:997–1003. doi:10.1056/NEJMoa043331
Sansregret L, Nepveu A (2011) Gene signatures of genomic instability as prognostic tools for breast cancer. Futur Oncol 7:591–594. doi:10.2217/fon.11.34
Decaux O, Lode L, Magrangeas F, Charbonnel C, Gouraud W, Jezequel P, Attal M, Harousseau JL, Moreau P, Bataille R, Campion L, Avet-Loiseau H, Minvielle S, Intergroupe Francophone du M (2008) Prediction of survival in multiple myeloma based on gene expression profiles reveals cell cycle and chromosomal instability signatures in high-risk patients and hyperdiploid signatures in low-risk patients: a study of the Intergroupe Francophone du Myelome. J Clin Oncol 26:4798–4805. doi:10.1200/JCO.2007.13.8545
Bakhoum SF, Danilova OV, Kaur P, Levy NB, Compton DA (2011) Chromosomal instability substantiates poor prognosis in patients with diffuse large B-cell lymphoma. Clin Cancer Res 17:7704–7711. doi:10.1158/1078-0432.CCR-11-2049
Watanabe T, Kobunai T, Yamamoto Y, Matsuda K, Ishihara S, Nozawa K, Yamada H, Hayama T, Inoue E, Tamura J, Iinuma H, Akiyoshi T, Muto T (2012) Chromosomal instability (CIN) phenotype, CIN high or CIN low, predicts survival for colorectal cancer. J Clin Oncol 30:2256–2264. doi:10.1200/JCO.2011.38.6490
Carter SL, Eklund AC, Kohane IS, Harris LN, Szallasi Z (2006) A signature of chromosomal instability inferred from gene expression profiles predicts clinical outcome in multiple human cancers. Nat Genet 38:1043–1048. doi:10.1038/ng1861
Lee AJ, Endesfelder D, Rowan AJ, Walther A, Birkbak NJ, Futreal PA, Downward J, Szallasi Z, Tomlinson IP, Howell M, Kschischo M, Swanton C (2011) Chromosomal instability confers intrinsic multidrug resistance. Cancer Res 71:1858–1870. doi:10.1158/0008-5472.CAN-10-3604
Bertucci F, Finetti P, Sabatier R, Birnbaum D (2010) The CINSARC signature: prognostic and predictive of response to chemotherapy? Cell Cycle 9:4025–4027
Chibon F, Lagarde P, Salas S, Perot G, Brouste V, Tirode F, Lucchesi C, de Reynies A, Kauffmann A, Bui B, Terrier P, Bonvalot S, Le Cesne A, Vince-Ranchere D, Blay JY, Collin F, Guillou L, Leroux A, Coindre JM, Aurias A (2010) Validated prediction of clinical outcome in sarcomas and multiple types of cancer on the basis of a gene expression signature related to genome complexity. Nat Med 16:781–787. doi:10.1038/nm.2174
Yan W, Zhang W, You G, Bao Z, Wang Y, Liu Y, Kang C, You Y, Wang L, Jiang T (2012) Correlation of IDH1 mutation with clinicopathologic factors and prognosis in primary glioblastoma: a report of 118 patients from China. PLoS ONE 7:e30339. doi:10.1371/journal.pone.0030339
Zhang C, Bao Z, Zhang W, Jiang T (2013) Progress on molecular biomarkers and classification of malignant gliomas. Front Med 7:150–156. doi:10.1007/s11684-013-0267-1
da Huang W, Sherman BT, Lempicki RA (2009) Systematic and integrative analysis of large gene lists using DAVID bioinformatics resources. Nat Protoc 4:44–57. doi:10.1038/nprot.2008.211
Subramanian A, Tamayo P, Mootha VK, Mukherjee S, Ebert BL, Gillette MA, Paulovich A, Pomeroy SL, Golub TR, Lander ES, Mesirov JP (2005) Gene set enrichment analysis: a knowledge-based approach for interpreting genome-wide expression profiles. Proc Natl Acad Sci USA 102:15545–15550. doi:10.1073/pnas.0506580102
Ng K, Kim R, Kesari S, Carter B, Chen CC (2012) Genomic profiling of glioblastoma: convergence of fundamental biologic tenets and novel insights. J Neurooncol 107:1–12. doi:10.1007/s11060-011-0714-2
Majdzadeh N, Wang L, Morrison BE, Bassel-Duby R, Olson EN, D’Mello SR (2008) HDAC4 inhibits cell-cycle progression and protects neurons from cell death. Dev Neurobiol 68:1076–1092. doi:10.1002/dneu.20637
Chen B, Cepko CL (2009) HDAC4 regulates neuronal survival in normal and diseased retinas. Science 323:256–259. doi:10.1126/science.1166226
Osada H, Tatematsu Y, Saito H, Yatabe Y, Mitsudomi T, Takahashi T (2004) Reduced expression of class II histone deacetylase genes is associated with poor prognosis in lung cancer patients. Int J Cancer 112:26–32. doi:10.1002/ijc.20395
Sun X, Wei L, Chen Q, Terek RM (2009) HDAC4 represses vascular endothelial growth factor expression in chondrosarcoma by modulating RUNX2 activity. J Biol Chem 284:21881–21890. doi:10.1074/jbc.M109.019091
Yang Y, Tse AK, Li P, Ma Q, Xiang S, Nicosia SV, Seto E, Zhang X, Bai W (2011) Inhibition of androgen receptor activity by histone deacetylase 4 through receptor SUMOylation. Oncogene 30:2207–2218. doi:10.1038/onc.2010.600
Negrini S, Gorgoulis VG, Halazonetis TD (2010) Genomic instability—an evolving hallmark of cancer. Nat Rev Mol Cell Biol 11:220–228. doi:10.1038/nrm2858
Watanabe T, Wu TT, Catalano PJ, Ueki T, Satriano R, Haller DG, Benson AB 3rd, Hamilton SR (2001) Molecular predictors of survival after adjuvant chemotherapy for colon cancer. N Engl J Med 344:1196–1206. doi:10.1056/NEJM200104193441603
Swanton C, Nicke B, Schuett M, Eklund AC, Ng C, Li Q, Hardcastle T, Lee A, Roy R, East P, Kschischo M, Endesfelder D, Wylie P, Kim SN, Chen JG, Howell M, Ried T, Habermann JK, Auer G, Brenton JD, Szallasi Z, Downward J (2009) Chromosomal instability determines taxane response. Proc Natl Acad Sci USA 106:8671–8676. doi:10.1073/pnas.0811835106
Cahill DP, Kinzler KW, Vogelstein B, Lengauer C (1999) Genetic instability and darwinian selection in tumours. Trends Cell Biol 9:M57–M60
Esteller M, Garcia-Foncillas J, Andion E, Goodman SN, Hidalgo OF, Vanaclocha V, Baylin SB, Herman JG (2000) Inactivation of the DNA-repair gene MGMT and the clinical response of gliomas to alkylating agents. N Engl J Med 343:1350–1354. doi:10.1056/NEJM200011093431901
Jacinto FV, Esteller M (2007) Mutator pathways unleashed by epigenetic silencing in human cancer. Mutagenesis 22:247–253. doi:10.1093/mutage/gem009
Acknowledgments
This work was supported by grants from the National High Technology Research and Development Program of China (863) (no. 2012AA02A508), National Natural Science Foundation of China (no. 81172409), and the Science and Technology Department of Liaoning Province (no. 2011225034).
Conflict of interest
The authors declare no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Wen Cheng and Mingyang Li have contributed equally to this work.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Cheng, W., Li, M., Cai, J. et al. HDAC4, a prognostic and chromosomal instability marker, refines the predictive value of MGMT promoter methylation. J Neurooncol 122, 303–312 (2015). https://doi.org/10.1007/s11060-014-1709-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-014-1709-6