Abstract
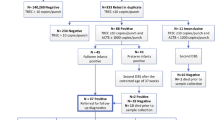
In 2002, the U.S. Health Resources and Services Administration (HRSA) commissioned the American College of Medical Genetics (ACMG) to recommend a uniform newborn screening (NBS) panel. The ACMG sent out a survey to stakeholders to evaluate 80 metabolic and genetic conditions and 3 infectious diseases (Human Immunodeficiency Virus (HIV), Toxoplasmosis (Toxo), and Cytomegalovirus (CMV)). In March 2005, the ACMG/HRSA report recommended a panel including 29 metabolic and genetic conditions and 25 secondary targets. This panel was endorsed by the newly-formed U.S. Advisory Committee on Heritable Disorders and Genetic Diseases in Newborns and Children (Advisory Committee). Decisions about infectious diseases were deferred by the ACMG/HRSA committee due to limited survey responses and lack of expertise of surveyed stakeholders and committee members. The Advisory Committee has not pursued these conditions further. In this manuscript, we examine the attitudes of U.S. pediatricians toward targeted and universal screening of newborns for these three infectious diseases. Members of the American Academy of Pediatrics (AAP) sections of infectious disease (n = 150) and community pediatrics (n = 150) plus 13 contributors to the AAP Red Book were surveyed by email or fax. Of eligible pediatricians, 113 of 297 (38%) returned surveys. Seventy-four percent supported either targeted or universal NBS for HIV, 57% for Toxo, but only 42% for CMV. The majority of respondents support screening newborns for HIV and Toxo. The Advisory Committee ought to solicit a systematic evaluation of these conditions to determine whether they should be included in the uniform panel.

Similar content being viewed by others
Abbreviations
- AAP:
-
American Academy of Pediatrics
- ACMG:
-
American College of Medical Genetics
- Advisory Committee:
-
Advisory Committee on Heritable Disorders and Genetic Diseases in Newborns and Children
- CMV:
-
Cytomegalovirus
- HAART:
-
Highly Active AntiRetroviral Therapy
- HIV:
-
Human Immunodeficiency Virus
- HRSA:
-
(U.S.) Health Resources and Services Administration
- ID:
-
Infectious Diseases
- NBS:
-
Newborn screening
- PKU:
-
Phenylketonuria
- Toxo:
-
Toxoplasmosis
References
Committee for the Study of Inborn Errors of Metabolism, Division of Medical Sciences, Assembly of Life Sciences, National Research Council. (1975). Genetic screening: Programs, principles, and research. Washington, DC: National Academy of Sciences.
National Newborn Screening and Genetics Resource. National newborn screening status report. Updated 22 Oct 2008. Retrieved Oct 30, 2008 from http://genes-r-us.uthscsa.edu/nbsdisorders.pdf.
American College of Medical Genetics (ACMG). Health Resources and Services Administration (HRSA). Newborn screening: Toward a uniform screening panel and system. Retrieved 30 Oct 2008 from ftp://ftp.hrsa.gov/mchb/genetics/screeningdraftforcomment.pdf.
National Newborn Screening and Genetics Resource. National newborn screening status report. Updated 7 Aug 2008. http://genes-r-us.uthscsa.edu/nbsdisorders.pdf.
Cameron, T. (2002). Mandatory HIV testing of newborns in New York State: What are the implications? Journal of Health & Social Policy, 14(3), 59–78. doi:10.1300/J045v14n03_04.
(1999). Connecticut will test newborns if mother isn’t tested first. AIDS Policy & Law, 14(13), 7.
Anonymous. (2006). Testing. Illinois passes law requiring HIV tests for newborns. AIDS Policy & Law, 21(14), 2.
Hsu, H. W., Grady, G. F., Maguire, J. H., Weiblen, B. J., & Hoff, R. (1992). Newborn screening for congenital Toxoplasmosis infection: Five years experience in Massachusetts USA. Scandinavian Journal of Infectious Diseases. Supplementum, 84, 59–64.
Jones, C. A. (2003). Congenital Cytomegalovirus Infection. Current Problems in Pediatric and Adolescent Health Care, 33, 65–93. doi:10.1016/S1538-5442(03)90007-1.
Barbi, M., Binda, S., Caroppo, S., Ambrosetti, U., Corbetta, C., & Sergi, P. (2003). A wider role for congenital cytomegalovirus infection in sensorineural hearing loss. The Pediatric Infectious Disease Journal, 22, 39–42. doi:10.1097/00006454-200301000-00012.
Fowler, K. B., Dahle, A. J., Boppana, S. B., & Pass, R. F. (1999). Newborn hearing screening: Will children with hearing loss caused by congenital cytomegalovirus infection be missed? The Journal of Pediatrics, 135, 60–64. doi:10.1016/S0022-3476(99)70328-8.
Shafer, F. E., Lorey, F., Cunningham, G. C., Klumpp, C., Vichinsky, E., & Lubin, B. (1996). Newborn screening for sickle cell disease: 4 years of experience from California’s newborn screening program. Journal of Pediatric Hematology and Oncology, 18, 36–41.
Panepinto, J. A., Magid, D., Rewers, M. J., & Lane, P. A. (2000). Universal versus targeted screening of infants for sickle cell disease: A cost-effectiveness analysis. The Journal of Pediatrics, 136, 201–208.
Grosse, S. D., Olney, R. S., & Baily, M. A. (2005). The cost effectiveness of universal versus selective newborn screening for sickle cell disease in the US and the UK: A critique. Applied Health Economics and Health Policy, 4, 239–247.
Nelson, H. D., Bougatsos, C., & Nygren, P. (2008). 2001 US preventive services task force. Universal newborn hearing screening: Systematic review to update the 2001 US preventive services task force recommendation. Pediatrics, 122(1), e266–e276. doi:10.1542/peds.2007-1422.
Kemper, A. R., & Downs, S. M. (2000). A cost-effectiveness analysis of newborn hearing screening strategies. Archives of Pediatrics & Adolescent Medicine, 154, 484–488.
Gilbert, F., Schoelkopf, J., Li, Z., Arzimanoglou, I. I., Shaham, M., Udey, J., et al. (1995). Ethnic intermarriage and its consequences for cystic fibrosis carrier screening. American Journal of Preventive Medicine, 11, 251–255.
Morgan, M. A., Driscoll, D. A., Mennuti, M. T., & Schulkin, J. (2004). Practice patterns of obstetrician-gynecologists regarding preconception and prenatal screening for cystic fibrosis. Genetics in Medicine, 6, 450–455. doi:10.1097/01.GIM.0000139509.04177.4B.
Marteau, T., & Dormandy, E. (2005). Haemoglobinopathy screening: An end to institutional racism? The British Journal of General Practice, 55, 419–420.
Acharya, K., Ackerman, P. D., & Ross, L. F. (2005). Pediatricians’ attitudes toward expanding newborn screening. Pediatrics, 116, e476–e484. Retrieved Oct 30, 2008 from http://pediatrics.aappublications.org/cgi/reprint/116/4/e476?maxtoshow=&HITS=10&hits=10&RESULTFORMAT=1&author1=acharya+k&andorexacttitle=and&andorexacttitleabs=and&andorexactfulltext=and&searchid=1&FIRSTINDEX=0&sortspec=relevance&resourcetype=HWCIT.
Koopmans, J., & Ross, L. F. (2006). Does familiarity breed acceptance? The influence of policy on physicians’ attitudes toward newborn screening programs. Pediatrics, 17, 1477–1484. doi:10.1542/peds.2005-1990.
Committee on Infectious Diseases American Academy of Pediatrics. (2005). Contributors. In L. K. Pickering (Ed.), Red Book: 2005 Report of the Committee on Infectious Diseases (27th ed.). Elk Grove Village IL: American Academy of Pediatrics.
Koopmans, J., Hiraki, S., & Ross, L. F. (2006). Comparative analysis of the attitudes of pediatricians and genetic counselors regarding testing and screening for CF and G6PD: Implications for counseling and policy. American Journal of Medical Genetics, 140A, 2305–2311. doi:10.1002/ajmg.a.31463.
Baily, M. A., & Murray, T. H. (2008). Ethics, evidence, and cost in newborn screening. The Hastings Center Report, 38, 23–31.
Grosse, S. D. (2005). Does newborn screening save money? The difference between cost-effective and cost-saving interventions. The Journal of Pediatrics, 146, 168–170.
Grosse, S. D., Teutsch, S. M., & Haddix, A. C. (2007). Lessons from cost-effectiveness research for United States public health policy. Annual Review of Public Health, 28, 365–391. doi:10.1146/annurev.publhealth.28.021406.144046.
Advisory Committee on Heritable Disorders and Genetic Diseases in Newborns and Children. Retrieved Oct 30, 2008 from http://www.mchb.hrsa.gov/programs/genetics/committee/charter.htm.
Wilson, J. M. G., Jungner, F., & Principles and Practice of Screening for Disease. (1968). Public Health Papers, no. 34. Geneva: World Health Organization.
National Screening Committee. First Report of the National Screening Committee. Health Departments of the United Kingdom. April 1998. Retrieved Oct 30, 2008 from http://www.nsc.nhs.uk/pdfs/nsc_firstreport.pdf.
National Institutes of Health Consensus Development Panel. (2001). National Institutes of Health Consensus Development Conference Statement: Phenylketonuria: Screening and management, October 16–18, 2000. Pediatrics, 108, 972–982. doi:10.1542/peds.108.4.972.
Lord, J., Thomason, M. J., Littlejohns, P., Chalmers, R. A., Bain, M. D., Addison, G. M., et al. (1999). Secondary analysis of economic data: A review of cost-benefit studies of neonatal screening for phenylketonuria. Journal of Epidemiology and Community Health, 53, 179–186.
Pandor, A., Eastham, J., Beverley, C., Chilcott, J., Paisley, S. (2004). Clinical effectiveness and cost-effectiveness of neonatal screening for inborn errors of metabolism using tandem mass spectrometry: A systematic review. Health Technology Assessment (Winchester, England), 8(12), iii, 1–121.
Lindegren, M. L., Byers, R. H., Thomas, P., David, S. F., Caldwell, B., Rogers, M., et al. (1999). Trends in perinatal transmission of HIV/AIDS in the United States. Journal of the American Medical Association, 282, 531–538. doi:10.1001/jama.282.6.531.
Wilfert, C. M., & Stringer, J. S. A. (2004). Prevention of Pediatric Human Immunodeficiency Virus. Seminars in Pediatric Infectious Diseases, 15, 190–198. doi:10.1053/j.spid.2004.05.003.
Meleski, M. E., & Damato, E. G. (2003). HIV exposure: Neonatal considerations. Journal of Obstetric, Gynecologic, and Neonatal Nursing, 32, 109–116. doi:10.1177/0884217502239808.
Kline, M. W. (2003). Human immunodeficiency virus protease inhibitors. The Pediatric Infectious Disease Journal, 22, 1085–1087. doi:10.1097/01.inf.0000103949.24130.45.
Boyer, K. M., Holfels, E., Roizen, N., Swisher, C., Mack, D., Remington, J., et al. (2005). Risk factors for Toxoplasma gondii infection in mothers of infants with congenital Toxoplasmosis: Implications for prenatal management and screening. American Journal of Obstetrics and Gynecology, 192(56), 4–71.
Ricci, M., Pentimalli, H., Thaller, R., Rava, L., & Di Ciommo, V. (2003). Screening and prevention of congenital Toxoplasmosis: an effectiveness study in a population with a high infection rate. The Journal of Maternal-Fetal & Neonatal Medicine, 14, 398–403. doi:10.1080/14767050412331312250.
Gilbert, R., Thalib, L., Tan, H., Paul, M., Wallon, M., Petersen, E., et al. (2007). Screening for congenital toxoplasmosis: Accuracy of immunoglobulin M and immunoglobulin A tests after birth. Journal of Medical Screening, 14, 8–13. doi:10.1258/096914107780154440.
Montoya, J. G., & Liesenfeld, O. (2004). Toxoplasmosis. Lancet, 363, 1965–1976. doi:10.1016/S0140-6736(04)16412-X.
McLeod, R., Boyer, K., Karrison, T., Kasza, K., Swisher, C., Roizen, N., et al. (2006). Outcome of treatment for congenital Toxoplasmosis, 1981–2004: the National Collaborative Chicago-Based, Congenital Toxoplasmosis Study. Clinical Infectious Diseases, 42, 1383–1394. doi:10.1086/501360.
Zaric, G. S., Bayoumi, A. M., Brandeau, M. L., & Owens, D. K. (2000). The cost effectiveness of voluntary prenatal and routine newborn HIV screening in the United States. Journal of Acquired Immune Deficiency Syndromes, 25, 403–416. doi:10.1097/00126334-200012150-00004.
Mrus, J. M., Yi, M. S., Eckman, M. H., & Tsevat, J. (2002). The impact of expected HIV transmission rates on the effectiveness and cost of ruling out HIV infection in infants. Medical Decision Making, 22(Suppl 5), S38–S44. doi:10.1177/027298902237710.
Sagmeister, M., Gessner, U., Kind, C., & Horisberger, B. (1995). Cost-benefit analysis of screening for congenital toxoplasmosis. Schweizerische Medizinische Wochenschrift. Supplementum, 65, 103S–112S.
Stray-Pedersen, B., & Jenum, P. (1997). Economic evaluation of preventive programmes against congenital toxoplasmosis. Scandinavian Journal of Infectious Diseases Supplement, 84, 86–96.
U.S. Preventive Services Task Force (USPSTF). Guide to Preventive Services. Retrieved Oct 30, 2008 from http://www.ahrq.gov/clinic/uspstfix.htm.
Demmler, G. (2005). Screening for congenital cytomegalovirus infections: A tapestry of controversies. The Journal of Pediatrics, 146, 162–163. doi:10.1016/j.jpeds.2004.11.020.
Naessens, A., Casteels, A., De Catte, L., & Foulon, W. (2005). A serologic strategy for detecting neonates at risk for congenital cytomegalovirus infection. The Journal of Pediatrics, 146, 194–197. doi:10.1016/j.jpeds.2004.09.025.
McAuley, J., Boyer, K. M., Patel, D., Mets, M., Swisher, C., Roizen, N., et al. (1994). Early and longitudinal evaluations of treated infants and children and untreated historical patients with congenital toxoplasmosis: The Chicago collaborative treatment trial. Clinical Infectious Diseases, 18, 38–72.
Coplan, J., Dye, T. D., Contello, K. A., Cunningham, C. K., Kirkwood, K., & Weiner, L. B. (1995). Failure to identify human immunodeficiency virus-seropositive newborns: Epidemiology and enrollment patterns in a predominantly white, nonurban setting. Pediatrics, 96, 1083–1089.
Hollier, L. M., Hill, J., Sheffield, J. S., & Wendel, G. D., Jr. (2003). State laws regarding prenatal syphilis screening in the United States. American Journal of Obstetrics and Gynecology, 189, 1178–1183. doi:10.1067/S0002-9378(03)00547-7.
Schrag, S. J., Arnold, K. E., Mohle-Boetani, J. C., Lynfield, R., Zell, E. R., Stefonek, K., et al. (2003). Prenatal screening for infectious diseases and opportunities for prevention. Obstetrics and Gynecology, 102, 753–760. doi:10.1016/S0029-7844(03)00671-9.
Jonna, S., Collins, M., Abedin, M., Young, M., Milteer, R., & Beeram, M. (1995). Postneonatal screening for congenital syphilis. The Journal of Family Practice, 41, 286–288.
Lewensohn-Fuchs, I., Osterwall, P., Forsgren, M., & Malm, G. (2003). Detection of herpes simplex virus DNA in dried blood spots making a retrospective diagnosis possible. Journal of Clinical Virology, 26, 39–41. doi:10.1016/S1386-6532(02)00019-7.
Barbi, M., Binda, S., Primache, V., Tettamanti, A., Negri, C., & Brambilla, C. (1998). Use of Guthrie cards for the early diagnosis of neonatal herpes simplex virus disease. The Pediatric Infectious Disease Journal, 17, 251–252. doi:10.1097/00006454-199803000-00017.
Neto, E. C., Rubin, R., Schulte, J., & Giugliani, R. (2004). Newborn screening for congenital infectious diseases. Emerging Infectious Diseases, 10, 1069–1073.
Robinson, J., Lee, B. E., Preiksaitis, J. K., Plitt, S., & Tipples, G. A. (2006). Prevention of congenital rubella syndrome—what makes sense in 2006? Epidemiologic Reviews, 28, 81–87. doi:10.1093/epirev/mxj007.
Asch, D. A., Jedrziewski, M. K., & Christakis, N. A. (1997). Response rates to mail surveys published in medical journals. Journal of Clinical Epidemiology, 50, 1129–1136. doi:10.1016/S0895-4356(97)00126-1.
Kellerman, S. E., & Herold, J. (2001). Physician response to surveys. A review of the literature. American Journal of Preventive Medicine, 20, 61–67. doi:10.1016/S0749-3797(00)00258-0.
Mayer, M. L., & Preisser, J. S. (2005). The changing composition of the pediatric medical subspecialty workforce. Pediatrics, 116, 833–840. doi:10.1542/peds.2004-2446.
Natowicz, M. (2005). Newborn screening—setting evidence-based policy for protection. The New England Journal of Medicine, 353, 867–870. doi:10.1056/NEJMp058060.
Botkin, J. R., Clayton, E. W., Fost, N. C., Burke, W., Murray, T. H., Baily, M. A., et al. (2006). Newborn screening technology: Proceed with caution. Pediatrics, 117, 1793–1799. doi:10.1542/peds.2005-2547.
Lin, L. S., Yager, J., & Leake, B. (1990). Professional vs. personal factors related to physicians’ attitudes toward drug testing. Journal of Drug Education, 20(95), 109.
Kinsella, T. D., & Verhoef, M. J. (1999). Determinants of Canadian physicians’ opinions about legalized physician-assisted suicide: A national survey. Annals of the Royal College of Physicians and Surgeons of Canada, 32, 211–215.
Schoenberger, N. E., Matheis, R. J., Shiflett, S. C., & Cotter, A. C. (2002). Opinions and practices of medical rehabilitation professionals regarding prayer and meditation. Journal of Alternative and Complementary Medicine, 8, 59–69. doi:10.1089/107555302753507186.
Abramson, S., Stein, J., Schaufele, M., Frates, E., & Rogan, S. (2000). Personal exercise habits and counseling practices of primary care physicians: A national survey. Clinical Journal of Sport Medicine, 10, 40–48. doi:10.1097/00042752-200001000-00008.
May, J. A., Warltier, D. C., & Pagel, P. S. (2002). Attitudes of anesthesiologists about addition and its treatment: a survey of Illinois and Wisconsin members of the American Society of Anesthesiologists. Journal of Clinical Anesthesia, 14, 284–289. doi:10.1016/S0952-8180(02)00359-8.
Acknowledgments
This research was done under the auspices of the Pritzker Summer Research Program which receives support from the University of Chicago Office of Medical Education and the National Institutes of Health. This research project was undertaken as part of a summer research program funded by the University of Iowa Carver College of Medicine.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schittek, H., Koopmans, J. & Ross, L.F. Pediatricians’ Attitudes About Screening Newborns for Infectious Diseases. Matern Child Health J 14, 174–183 (2010). https://doi.org/10.1007/s10995-008-0431-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-008-0431-4