Abstract
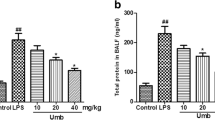
The present study aimed to determine the protective effects and the underlying mechanisms of unfractionated heparin on lipopolysaccharide (LPS)-induced endotoxemia and lung injury in rats. Rats were injected intravenously with LPS at 6 mg/kg. We examined the therapeutic effects of unfractionated heparin (100 or 300 U/kg) on LPS-induced endotoxemia by dosing intravenously simultaneously after LPS challenge. The animal lung edema degree was evaluated by wet/dry weight ratio. The levels of inflammatory mediators including interleukin-1β (IL-1β) and interleukin-6 (IL-6) were assayed by enzyme-linked immunosorbent assay and quantitative real-time RT-PCR. The activation of nuclear factor-κB (NF-κB) was evaluated by Western blotting. The investigations revealed that treatment with unfractionated heparin can attenuate inflammatory responses in a rat model of LPS-induced acute lung injury, and the effect was much better in 300 U/kg group. The mechanisms by which unfractionated heparin exerts its anti-inflammatory effect are correlated with inhibition of IL-1β and IL-6 production via inactivation of NF-κB.







Similar content being viewed by others
References
MacLaren, R., and K.A. Stringer. 2007. Emerging role of anticoagulants and fibrinolytics in the treatment of acute respiratory distress syndrome. Pharmacotherapy 27(6): 860–873.
Cepkova, M., and M.A. Matthay. 2006. Pharmacotherapy of acute lung injury and the acute respiratory distress syndrome. Journal of Intensive Care Medicine 21: 119–143.
Frutos-Vivar, F., N.D. Ferguson, and A. Esteban. 2006. Epidemiology of acute lung injury and acute respiratory distress syndrome. Seminars in Respiratory and Critical Care Medicine 27: 327–336.
Rubenfeld, G.D., E. Caldwell, E. Peabody, et al. 2005. Incidence and outcomes of acute lung injury. The New England Journal of Medicine 353: 1685–1693.
Ware, L.B., E. Camerer, K.E. Welty-Wolf, et al. 2006. Bench to bedside: targeting coagulation and fibrinolysis in acute lung injury. American Journal of Physiology. Lung Cellular and Molecular Physiology 291(3): L307–L311.
Bastarache, J.A., L.B. Ware, and G.R. Bernard. 2006. The role of the coagulation cascade in the continuum of sepsis and acute lung injury and acute respiratory distress syndrome. Seminars in Respiratory and Critical Care Medicine 27: 365–376.
Schultz, M.J., J.J. Haitsma, H. Zhang, et al. 2006. Pulmonary coagulopathy as a new target in therapeutic studies of acute lung injury or pneumonia: a review. Critical Care Medicine 34: 871–877.
Sapru, A., J.L. Wiemels, J.S. Witte, et al. 2006. Acute lung injury and the coagulation pathway: potential role of gene polymorphisms in the protein C and fibrinolytic pathways. Intensive Care Medicine 32(9): 1293–1303.
Welty-Wolf, K.E., M.S. Carraway, T.L. Ortel, et al. 2006. Blockade of tissue factor–factor X binding attenuates sepsis-induced respiratory and renal failure. American Journal of Physiology. Lung Cellular and Molecular Physiology 290: L21–L31.
Maybauer, M.O., D.M. Maybauer, J.F. Fraser, et al. 2006. Recombinant human activated protein C improves pulmonary function in ovine acute lung injury resulting from smoke inhalation and sepsis. Critical Care Medicine 34(9): 2432–2438.
Yasui, H., E.C. Gabazza, S. Tamaki, et al. 2001. Intratracheal administration of activated protein C inhibits bleomycin-induced lung fibrosis in the mouse. American Journal of Respiratory and Critical Care Medicine 163: 1660–1668.
Uchiba, M., K. Okajima, K. Murakami, et al. 1996. Recombinant thrombomodulin prevents endotoxin-induced lung injury in rats by inhibiting leukocyte activation. American Journal of Physiology 271: L470–L475.
Harada, N., K. Okajima, and M. Uchiba. 2006. Dalteparin, a low molecular weight heparin, attenuates inflammatory responses and reduces ischemia-reperfusion-induced liver injury in rats. Critical Care Medicine 34: 1883–1891.
Yagmurdur, M.C., E. Turk, G. Moray, et al. 2005. Effect of heparin on bacterial translocation and gut epithelial apoptosis after burn injury in the rat: dose-dependent inhibition of the complement cascade. Burns 31: 603–609.
Matzner, Y., G. Marx, R. Drexler, et al. 1984. The inhibitory effect of heparin and related glycosaminoglycans on neutrophil chemotaxis. Thrombosis and Haemostasis 52: 134–137.
Pahl, H.L. 1999. Activators and target genes of Rel/NF-kappaB transcription factors. Oncogene 18: 6853–6866.
Zingarelli, B. 2005. Nuclear factor-kappaB. Critical Care Medicine 33: S414–S416.
Liu, S.F., and A.B. Malik. 2006. NF-kappa B activation as a pathological mechanism of septic shock and inflammation. American Journal of Physiology. Lung Cellular and Molecular Physiology 290: L622–L645.
Grisham, M.B., L.A. Hernandez, and D.N. Granger. 1986. Xanthine oxidase and neutrophil infiltration in intestinal ischemia. American Journal of Physiology 251: G567–G574.
Smith, K.M., J.D. Mrozek, S.C. Simonton, et al. 1997. Prolonged partial liquid ventilation using conventional and high-frequency ventilatory techniques: gas exchange and lung pathology in an animal model of respiratory distress syndrome. Critical Care Medicine 25: 1888–1897.
Gando, S. 2010. Microvascular thrombosis and multiple organ dysfunction syndrome. Critical Care Medicine 38(2): S35–S42.
Schwartz, M.D., E.E. Moore, F.A. Moore, et al. 1996. Nuclear factor-kappaB is activated in alveolar macrophages from patients with acute respiratory distress syndrome. Critical Care Medicine 24(8): 1285–1292.
Bhatia, M., and S. Moochhala. 2004. Role of inflammatory mediators in the pathophysiology of acute respiratory distress syndrome. The Journal of Pathology 202: 145–156.
Tyrell, D.J., S. Kilfeather, and C.P. Page. 1995. Therapeutic uses of heparin beyond its traditional role as an anticoagulant. Trends in Pharmacological Sciences 16: 198–204.
Morrison, A.M., P. Wang, and I.H. Chaudry. 1996. A novel nonanticoagulant heparin prevents vascular endothelial cell dysfunction during hyperdynamic sepsis. Shock 6: 46–51.
Li, X., Z. Zheng, X. Li, et al. 2012. Unfractionated heparin inhibits lipopolysaccharide-induced inflammatory response through blocking p38 MAPK and NF-κB activation on endothelial cell. Cytokine 60(1): 114–121.
Cinel, I., and R.P. Dellinger. 2007. Advances in pathogenesis and management of sepsis. Current Opinion in Infectious Diseases 20: 345–352.
Li, X., Z. Zheng, Y.R. Mao, et al. 2012. Unfractionated heparin promotes LPS-induced endothelial barrier dysfunction: a preliminary study on the roles of angiopoietin/Tie2 axis. Thrombosis Research 129(5): e223–e228.
Acknowledgments
The authors give special thanks to Dr. Liang Wang (Department of Pathology, China Medical University) for the pathological analysis. The research which discussed unfractionated heparin was supported by the National Natural Science Foundation of China (81101411).
Conflict of Interest
The author declares that there are no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Li, X., Li, Z., Zheng, Z. et al. Unfractionated Heparin Ameliorates Lipopolysaccharide-Induced Lung Inflammation by Downregulating Nuclear Factor-κB Signaling Pathway. Inflammation 36, 1201–1208 (2013). https://doi.org/10.1007/s10753-013-9656-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10753-013-9656-5