Abstract
Conflicting data exist about the effects of cardiac resynchronization therapy (CRT) on diastolic function (DF). Aim of the study was to assess if and how CRT affects DF in systolic heart failure patients. We also investigated potential relations between CRT-induced left ventricular changes and the composite clinical endpoint of progressive heart failure and cardiac death over 3 years follow-up. 119 CRT patients underwent clinical evaluation and echocardiography before CRT and 4 months later. DF was quantified by transmitral velocities [E/A waves, deceleration time (DT), E/DT], early diastolic mitral annulus velocity (E′), E/E′ ratio and 2-D speckle tracking strain rate during isovolumetric relaxation (IVR, SRivr). End-diastolic pressure–volume relationship (EDPVR) was also assessed noninvasively using a single-beat method. Overall stiffness was quantified by ventricular stiffness (Klv) normalized to end-diastolic volume (EDV). New York Heart Association class improved at 4 months (from 2.7 ± 0.7 to 1.9 ± 0.6, p < 0.001) as did ventricular filling (E/DT from 0.48 ± 0.29 to 0.39 ± 0.31 cm/s2, p = 0.01). In contrast, relaxation (E′, SRivr) and filling pressures (E/E′, E/SRivr) did not change. Slope of EDPVR did not change with CRT. Such finding, together with an unmodified Klv/EDV and a 7 ± 18 % reduction in EDV (p = 0.001), suggested reverse remodelling towards a smaller equilibrium volume. Finally, end-systolic LV volume decreased from 147 ± 59 to 125 ± 52 ml and ejection fraction increased from 0.26 ± 0.07 to 0.32 ± 0.09 (both p < 0.001). Using a Cox regression model we found that only changes (Δ) in diastolic, but not systolic indexes, correlated with the composite clinical endpoint, with increments in ΔEDV20 and ΔE/DT, single or combined, greatly increasing risk of heart failure and/or cardiac death (p = 0.003). Ventricular reverse remodelling, together with improvement in ventricular filling, rather than improvements of systolic function, predict clinical prognosis long-term post-CRT.
Similar content being viewed by others
Introduction
Cardiac resynchronization therapy (CRT) improves functional capacity, left ventricular systolic function and survival in patients with chronic heart failure and left bundle branch block [1]. Not much, however, is known about the effects of CRT on diastolic function (DF) in these patients. This is surprising given that the increase in left ventricular filling pressure highly correlates with the degree of exercise limitation in patients with chronic heart failure, independent of the severity of systolic dysfunction [2]. Furthermore, the few previous studies of the impact of CRT on DF have presented variable and contrasting results [3–5].
Thus, the aim of the present study was to assess if and how CRT impacted DF in systolic heart failure patients. DF was assessed using echocardiographic load-dependent as well as relatively load-independent parameters. In addition, we analyzed the passive phase of ventricular diastole by the end-diastolic pressure–volume relationship (EDPVR) using a single-beat approach that uses noninvasively-estimated diastolic pressure and volume data [6, 7]. Since CRT can induce significant ventricular reverse remodelling [8], a non load-dependent index of EDPVR such as operative ventricular stiffness (Klv) [9] normalized to end-diastolic volume (EDV) was also used. Finally, we investigated potential relations between CRT-induced changes in diastolic parameters and clinical recurrence of heart failure and/or cardiac death over a follow-up of 3 years.
Methods
Population
One hundred eight five (185) patients with systolic heart failure (ejection fraction ≤35 %) and a clinical indication for CRT were retrospectively identified from our clinic. In all patients, informed consent had been previously obtained in accordance with institutional human studies committee guidelines. From this initial group we excluded patients with biological or mechanical mitral valves, atrial fibrillation or high heart rates that precluded a clear separation of E versus A waves on mitral inflow velocity acquisitions. No statistical differences in clinical and echocardiographic parameters between included and excluded patients were observed, apart from the proportion of AICDs versus pacemakers, which was higher in the included patients (p = 0.001) (Table 1).
Thus, our final population (Table 2) included 119 patients (mean age 69.8 ± 8.9 years, 81 % males) suffering from heart failure due to various aetiologies, who were candidates for CRT according to latest ESC guidelines (ejection fraction ≤35 %, QRS ≥120 ms and NYHA functional class II–III despite optimized medical therapy) [1]. Ischemic cardiomyopathy was defined as a documented previous myocardial infarction or significant coronary artery disease (luminal narrowing >50 %) at coronary arteriography. Optimal revascularization had been performed in these patients. Nonischemic aetiology was defined only in the presence of angiographically normal coronary arteries or a negative stress-rest thallium scan.
Patients were subjected to a transthoracic echocardiographic examination using standard equipment (Vivid 7 or Vivid E9, GE Medical System, Horten, Norway). Cardiac cycles were stored in digital format and then subjected to an off-line analysis using dedicated software (EchoPAC PC version BT10, GE Healthcare). Patients were imaged before implantation (29 ± 46 days) and after 4 months (125 ± 73 days). We evaluated left ventricular end-systolic and end-diastolic volumes and ejection fraction. In addition, we acquired extensive evaluation of diastolic echocardiographic parameters to quantify ventricular relaxation, filling pressures and left ventricular stiffness by continuous-Doppler, pulsed and tissue Doppler according to published guidelines [10]. Furthermore, we quantified ventricular dyssynchrony using Temporal Uniformity of Strain (TUS) Index applied to longitudinal strains from 2D speckle-tracking echocardiographic images. [11].
Patients also underwent a clinical evaluation at baseline and after 4 months to assess NYHA functional class, to complete a Minnesota Living with Heart Failure Questionnaire (MLWHFQ) and perform a 6 min walk test. During subsequent long-term clinical follow-up (980 ± 667 days) exacerbations of heart failure causing hospitalization or activation of “OPTIVOL”, available in 39 patients, requiring additional diuretic administration or death were recorded.
Echocardiographic measurements
Ventricular volumes were calculated in biplane mode using Simpson’s method applied to images obtained in the apical 4- and 2-chamber views. The degree of mitral regurgitation was assessed calculating the area of the regurgitant jet on colour-Doppler images (4- and 2-chambers) and expressed as a percentage of the left atrium area.
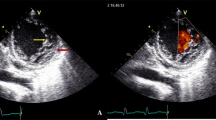
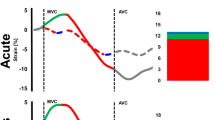
Diastolic function was characterized by classical load-dependent and relatively load-independent parameters. Classical load-dependent parameters included: transmitral early and late diastolic velocity (E and A waves), E-wave deceleration time (DT), E/A and E/DT ratio assessed using pulsed Doppler in 4-chamber view. Relatively load-independent parameters included: early diastolic mitral annulus velocity (average of septal-lateral-front and posterior annulus E′) obtained using pulsed tissue Doppler in the apical 2- and 4-chamber views. E′ can be considered as a ventricular relaxation index [10], while the E/E′ ratio represents a noninvasive estimation of ventricular filling pressures [12]. Colour M-mode Doppler mitral flow propagation velocity (Vp) was also obtained in a 4-chamber projection [13]. We were able to calculate this parameter in 53 patients only. We also assessed longitudinal strain rates during isovolumetric relaxation (IVR) and in the early phase of diastolic filling [14]. Such parameters were obtained applying a speckle-tracking algorithm to 4- and 2-chambers apical projections, with the endocardium manually traced and software automatically drawing epicardial edges in order to identify the region of interest and to derive a strain curve. The first derivative of the strain curve presents two diastolic peaks: the first peak (after aortic valve closure) represents global peak strain rate during isovolumetric relaxation (SRivr) and is an index of relaxation rate [15] (Fig. 1). The second peak represents strain rate during early ventricular filling (SRe) and it is affected by the final balance between ventricular relaxation and atrial pressure [14]. Finally we identified the IVR interval by taking into account the aortic and mitral valve openings and closings with pulsed wave Doppler. IVR interval was reported on the strain graph in order to identify SRivr. E/SRivr ratio was also computed and taken as a measure of ventricular filling pressures.
Strain rate analysis using spleckle-tracking echocardiography applied to a 4-chamber view in a patient. The mean derivative curve of strain (white, dotted line) shows two diastolic peaks. The first peak represents the global peak strain rate during isovolumetric relaxation (SRivr), while the second peak represents strain rate during early ventricular filling (SRe). AVC aortic valve closure valve closure, MVO mitral valve opening
Ventricular dyssynchrony was indexed pre and 4 months post CRT by TUS, whereby a time plot of regional strains, arranged for ventricular location, is subjected to a Fourier analysis. If segments shorten simultaneously (synchronously), the plot appears as a straight line, with power only in the zero-order Fourier term, whereas regionally clustered dyssynchrony generates an undulating plot with higher power in the first-order term. TUS index reflects zero-order relative to first-order plus zero-order power [11]. We and others have shown that baseline asynchrony and coincidence between the latest mechanical activation site and left ventricular lead position predict favourable prognosis after CRT [11, 16, 17].
Finally we assessed ventricular passive properties according to a single-beat end-diastolic elastance algorithm which allows noninvasive estimation of the EDPVR from EDV and end-diastolic pressure (EDP) [6, 7]. According to this algorithm the EDPVR of any healthy or sick heart can be estimated by a nonlinear analytical expression: EDP = α.EDV^β where EDP is obtained from E/E′ according to the following equation [EDP = 1.91 + (1.24·E/E′)] [12]. Values obtained in this manner were then normalized to fixed values of EDP (10, 20, 30 mm Hg) in order to compare subjects and make comparisons; [EDV10, EDV20, EDV30 = (EDP/α)^1/β, with EDP = 10, 20, or 30 mmHg, respectively].
It is recognized, indeed, that there are limitations in E/E′-based measurements of filling pressures in patients with conduction abnormalities or undergoing pacing [18]. Thus, passive ventricular properties were also quantified by Klv, which was determined from DT according to the following equation (Klv = 1.28exp[−0.008DT]); this approach has been validated by invasive methods in a group of comparable cardiomyopathic patients [9]. Values were then normalized to EDV (Klv/EDV).
Device implantation
All patients received a biventricular pacemaker (10 CRT-P, 109 CRT-D) with lead positions in conventional locations (right atrium, right ventricle and the coronary sinus). Implanted devices were: 18 GUIDANT (Renewal®), 38 MEDTRONIC (12 Concerto HF®, 17 Consulta CRT®, 5 Insync®, 4 Sentry®), 38 SAINT JUDE (20 Atlas HF®, 11 Promote Accel®, 2 Epic HF®, 2 Frontier 2®, 2 Unify®, 1 Anthem®), 9 BIOTRONIK (Lumax HF®), 6 SORIN-ELA (4 Paradyn CRT®, 1 Newliving CHF®, 1 Ovatio CRT®) 10 BOSTON SCIENTIFIC (Cognis®). All subjects underwent echocardiographic-guided atrioventricular optimization 2–3 days after implantation (mean atrioventricular interval 133 ± 30 ms). Interventricular delay was set fixed at 0 ms.
Statistical analysis
Data are expressed as mean ± standard deviation. Differences between means were assessed using t tests for paired data. Signed rank tests were used if data were not normally distributed. Chi square test was used to compare proportions. Univariate and multivariate Cox regression analyses were used to evaluate the relationship between echocardiographic parameters with significant variations pre- and post-CRT (with the exception of age, gender, aetiology of cardiac disease and QRS duration) versus recurrence of heart failure or death (whichever came first) during a 3 year follow-up period. Survival analysis was performed by Kaplan–Meier survival analysis with significance testing using log-rank statistics and a post hoc Holm–Sidak test. A two-way repeated-measures ANOVA was finally used to assess the effects of CRT on time changes in Vp, with the attribution to responder versus nonresponder group as a between-patient factor. A p value <0.05 was considered as statistically significant. Analyses were performed using Sigmaplot (version 12.5 for Windows, Jandel; San Rafael, CA) statistical software.
Variability of analysis
Inter-observer variability of echo-Doppler parameters was determined from 30 randomly selected patients and assessed as absolute mean difference ± the percentage coefficient of variation (SD/mean). Reproducibility was: 6.6 mL ± 0.93 % for EDV, 0.04 cm/s2 ± 1.1 % for E/DT, 0.92 ± 0.75 % for E/E′, 0.02 s ± 1.2 % for IVR, 0.06 s−1 ± 9.4 % for SRivrt, 0.09 s−1 ± 1.55 % for SRe and 0.15 ± 1.2 % for TUS longitudinal index.
Results
All clinical parameters improved significantly after CRT (NYHA from 2.7 ± 0.7 to 1.9 ± 0.6, quality of life score from 27.3 ± 21.5 to 17.6 ± 19.9, 6 min walking test from 350 ± 114 min to 393 ± 107 min, p < 0.001 for all). QRS and heart rate decreased (−4.4 ± 20.8 and −2.4 ± 19.4 %, p = 0.005 and p = 0.01, respectively). At 4 months (Table 3) echocardiographic derived findings improved as well, showing decreases in ventricular volumes, better ejection fraction and reduced mitral regurgitation. TUS index, measured in the longitudinal axis, increased after CRT (+12 ± 40 %, p = 0.035, Table 3), suggesting amelioration of baseline dyssynchrony.
Load-dependent left ventricular filling parameters improved too: E wave velocity decreased (−9.8 ± 28.6 cm/s, p < 0.001), as did the E/A ratio (−0.4 ± 1.2, p = 0.045). Due to an increment in DT, the E/DT ratio decreased significantly (−0.09 ± 0.33 cm/s2, p = 0.01) suggesting improved filling characteristics.
Noninvasive left ventricular filling pressure measurements tended to decrease, but insignificantly (E/E′ −1.4 ± 9.9 cm/s; SRe +0.0026 ± 0.22 s−1; E/SRivr −592 ± 3,384; estimated EDP from 22.4 ± 12.6 mmHg to 20.1 ± 12.9 mmHg; ns for all). Furthermore, no significant changes could be detected for the diastolic relaxation indices E′ and SRivr (Table 3). IVR increased post-CRT (+0.014 ± 0.05 s, p = 0.014).
As far as the diastolic passive properties were concerned (Fig. 2), at 4 months follow-up there were significant (p < 0.05) reductions in EDV10 EDV20 and EDV30, with no change in slope coefficients of EDPVR, consistent with an unmodified Klv/EDV. As shown in the figure and Table 3, there was a significant shift of the estimated EDPVR to smaller volumes, indicative of reverse remodeling.
Clinical outcomes
Follow-up data, obtained from hospital records and/or telephone interviews with patients or their relatives, were available for all but 1 subject, who was lost at follow-up. Three more patients died for unknown reasons before any information about their clinical status prior to death could be acquired and were thus excluded from survival analysis There were 44 patients that reached the end-point (13 deaths, 26 patients with heart failure hospitalizations, 5 patients with “OPTIVOL” alarm activations followed by additional diuretic administration).
According to the univariate results (accepted level p < 0.1) of the Cox regression analysis ΔE/DT (p = 0.013), taken as a cumulative descriptor of ventricular filling, ΔEDV20 (p = 0.021), expression of the amount of CRT-induced ventricular reverse remodeling [19], and changes in end-systolic volume (ΔESV, p = 0.002), used as an index of ventricular performance, were included, as continuous covariates expressed as a percent change, in the multivariate analysis. Gender and etiology of ventricular dysfunction (ischemic/nonischemic) were also included as categorical covariates together with age and duration of QRS, gender acting as a stratum [20]. The analysis showed that progressive ventricular remodeling (ΔEDV20% p = 0.053) and worsening in left ventricular filling characteristics (ΔE/DT % p = 0.053) predicted heart failure exacerbations or death during the follow-up. Patients’ age (p = 0.015) and ischemic etiology (p = 0.013) contributed too. There was no significant contribution from ΔESV % or QRS duration (p = 0.609 and p = 0.682, respectively).
In order to confirm that ΔEDV20 and ΔE/DT (both measurements available in 84 patients) affected survival after CRT, we performed a Kaplan–Mayer analysis classifying the CRT population on a ΔEDV20 [−7.47 ml (−4.34 % relative to pre CRT)] plus an ΔE/DT [−0.05 cm/s2 (−18 % relative to pre CRT)] entire population median basis. Thus, 3 groups were created according to the values of ΔEDV20 and ΔE/DT compared to the related medians (group 1, n = 22: ΔEDV20 <5 % and ΔE/DT <18 %; group 2, n = 41: ΔEDV20 <5 % and ΔE/DT >18 % or ΔEDV20 >5 % and ΔE/DT <18 %; group 3, n = 21: ΔEDV20 >5 % and ΔE/DT >18 %).
Event-free survival curves for the three groups, shown in Fig. 3, were significantly different (log-rank test p = 0.001). Group 3 event-free survival was half of that of group 1 at the end of follow-up. Furthermore, group 3 event-free survival rapidly decreased in the first 500 days after CRT. In contrast, group 1 event-free survival was maintained around 90 % until the end of the observation period. The difference, based on a post hoc Holm–Sidak test was statistically significant (p < 0.006). Group 2 exhibited an intermediate trend, with improved event-free survival as compared with group 3 (p < 0.03), but worse relative to group 1, although not at a significant level (p = 0.113, ns). The results could not be explained by differences in the drug distribution among the three groups. The percentage of patients treated with beta-blockers (85, 75, 68 %), diuretics (76, 73, 77 %) and ACE inhibitors/AT1 antagonists (86, 85, 86 %) was not dissimilar among the 3 groups (p = 0.995).
Survival curves obtained dividing patients into three groups according to values of ΔEDV20 and ΔE/DT compared to the related medians. Group 1: ΔEDV20 <5 % and ΔE/DT <18 %, group 2: ΔEDV20 <5 % and ΔE/DT >18 % or ΔEDV20 >5 % and ΔE/DT <18 %, group 3 ΔEDV20 >5 % and ΔE/DT >18 %. Group 3 survival is half of that of group 1 at the end of follow-up. Furthermore, group 3 survival rapidly decreases in the first 500 days after CRT. In group 1 instead, survival from heart failure and cardiac death is maintained around 90 % until the end of the observation. The difference is statistically significant (p < 0.006). Group 2 exhibits an intermediate trend, with an improved survival as compared with group 3 (p < 0.03) but worse than group 1, although not at a significant level (p = 0.113, ns)
Discussion
Our study demonstrates that CRT does not significantly affect relaxation phase (E′ and SRivr), nor filling pressures (E/E′ and E/SRivr) in patients affected by dilated cardiomyopathy and systolic heart failure at 4-month follow-up. CRT, however, induces left ventricular reverse remodelling, resulting in a smaller ventricle with improved filling characteristics. Both dyssynchrony and systolic function improve after CRT, as demonstrated by TUS index and ejection fraction increments versus systolic volume decrements, but such changes do not seem to influence patients’ outcome long-term in a significant way.
Previous studies have demonstrated that CRT improves DF only in patients with an associated improvement in systolic function [3, 4]. However, data regarding CRT effects on diastole are controversial. Waggoner et al. [4] evaluated DF in a cohort of 50 heart failure patients receiving CRT using conventional echocardiographic measurements before and after 4-month follow-up. They defined as “responders” patients with an >5 % increase in ejection fraction at 4-month. Transmitral parameters (E, E/A, DT) and E/E′ ratio showed significant improvements only in responders. E′, an indirect index of relaxation, did not change in either group. The authors concluded that CRT exerts a beneficial effect on LV filling pressures but does not affect relaxation properties.
Jansen et al. [3] evaluated DF after up to 12 months of CRT. Both diastolic load-dependent and relatively load-independent measurements (respectively E, E/A, DT, E′ and E/E′) were significantly improved only in responders, defined as patients with a reduction >15 % in LV systolic volume at 12-month follow-up. In contrast to Waggoner et al., they concluded that reverse remodelling induced by CRT was associated with an improvement in both relaxation and filling pressures. Along the same line of thinking, Aksoy et al. [21] documented an improvement in filling pressures, estimated using the E/E′ ratio, only in responders defined as patients with a reduction ≥10 % in LV systolic volume at 6-month follow-up after CRT.
Porciani et al. [22] classified 65 patients according to the transmitral profile in restrictive and non restrictive filling patterns (25 vs. 40 patients). At 12-month follow-up after CRT implantation E/A ratio increased and DT decreased in the non-restrictive filling pattern group. In the restrictive group, instead, 13 patients showed a reduction in E/A and an increase in DT, while in the remaining patients the restrictive filling pattern did not vary. All cause mortality rate was 5 % in non restrictive filling pattern group, 15 % in patients with reversible restrictive filling pattern and 42 % in patients with persistent restrictive filling profile. These authors concluded that CRT improves DF in a considerable number of patients with filling restriction at implantation, but persistence of the restriction pattern after CRT is associated with worse outcome.
Shanks et al. [15] evaluated DF using speckle-tracking imaging, in addition to conventional methods. One hundred eighty-eight heart failure patients were evaluated before CRT implantation and at 6-month follow-up. Responders were defined as patients with a decrease in LV systolic volume ≥15 % 6 months after implantation. Among conventional echocardiographic parameters only DT showed an improvement in both responders and non responders. All the remaining parameters, such as E, E/A, E′ and E/E′, did not show any significant changes. SRivr and E/SRivr ratios, obtained with speckle-tracking analysis, improved only in responders, suggesting that CRT has beneficial effects on both relaxation and filling pressures.
Retracing Shanks’ study, our aim was to evaluate DF in patients with dilated cardiomyopathy and to verify if and how improvements after CRT, if any, affect patients’ outcomes. In line with previous studies, we documented an improvement in transmitral flow parameters, which are load-dependent. In contrast with data in literature, however, neither relaxation parameters (E′ and SRivr) nor indirect filling pressure descriptors (E/E′ and E/SRivr) showed statistically significant improvements. Only IVR increased significantly.
As mentioned before, ventricular diastolic relaxation is influenced by both myocardial inactivation and asynchrony [23]. Since asynchrony decreased after CRT, as documented by the improvements in TUS index, it is difficult to substantiate why this improvement does not affect relaxation parameters. A first interpretation may be that although CRT reduces asynchrony, it does not modify intracellular factors (such as SERCA quantity) involved in the process of pressure decay during IVR, in contrast with other experimental studies [24]. This conclusion is consistent with prior animal studies showing no change in the rate of relaxation despite large changes in the degree of ventricular synchrony [25]. In a more realistic scenario the modifications induced by CRT are minor and not easily inferable from noninvasive indices, with limited reliability in quantification of ventricular relaxation.
Effects of CRT on ventricular passive properties
In contrast to previous noninvasive studies, we evaluated ventricular passive properties and how they were affected by CRT. After having computed EDV10, EDV20 EDV30 and Klv/EDV we can conclude that CRT induces reverse remodelling with no change in slope of EDPVR (Table 3). Such shift towards a smaller equilibrium volume, with no significant change in diastolic curve profile, would substantiate previous invasive studies performed in a smaller study reporting a simple reduction in ventricular volume post-CRT, with no change in stiffness [26].
In our study, the reverse remodelling effect of CRT was associated with no statistically significant change in filling pressures, but with an improvement in the filling profile that seems to have prognostic relevance. Survival analysis, in fact, proves that patients with reduction in ΔE/DT greater than 18 % post-CRT exhibit better survival based on the composite clinical endpoint of worsening heart failure or cardiac death (Fig. 3). The combination of improved filling and reverse remodelling could possibly be related to a reduction in convective deceleration due to decrement in turbulent forces associated with cardiomegaly [27, 28]. Unfortunately, there was no difference in Vp (available before and after CRT in 53 patients only) between the two groups created by dividing the population according to ΔEDV20 <>5 %, although overall Vp increased in both groups after CRT (+4.9 ± 12.8 vs. + 5.8 ± 17.9 cm/s, interaction p = ns). There was, instead, a significant interaction (p = 0.002) between time changes in Vp and CRT when ΔE/DT <>18 % was used as a grouping criterion (−2.4 ± 15.2 vs. +10.3 ± 11.2 cm/s). Such findings are compatible with ventricular overfilling in patients doing badly after CRT and do not conflict with the hypothesis of a modest increment in apical gradient in those improving after CRT [29, 30].
Limitations
Operator-dependency of all the measured echocardiographic measurements is an unavoidable limitation. In practical terms, this limits the reliability of the data acquisition process. In this regard NMR data would have been more reliable, but difficult to obtain in this patients’ population.
The experimental data were partly biased by not calculating SRivr in those patients with an inadequate apical 4-chamber and/or 2-chamber view. Thirdly, DF was not evaluated via invasive measurements of pressure and volume but exclusively inferred from echocardiographic parameters. It should be considered, however, that the estimate of EDPVR from a single beat has demonstrated a good correlation with EDPVR measured with invasive techniques, as reported by Klotz et al. [6, 7]. Thus, EDV10–20–30 can be considered as a reliable parameter for describing the ventricular passive properties and can be used to describe the process of reverse remodeling after CRT as long as the original input is correct. Given the limitations of E/E′-based measurements of filling pressures in patients with conduction abnormalities or undergoing pacing [18], we used Klv/EDV as another parameter, beyond single-beat EDPVR, in order to confirm the changes in ventricular characteristics post-CRT.
Another limitation to be taken into consideration is the relatively small sample size and short follow-up time at which echocardiographic data were obtained. Expansion of the patients’ population and another echocardiographic assessment, after 6 or 12 months, would have allowed verification of the positive trend in the filling profile and echocardiographic parameters of relaxation. In this regard it has to be underlined that the use of the E–E′ time interval, instead of the indexes here considered, could have been better descriptor of the relaxation behavior pre/post-CRT [31]. Unfortunately, in our data, the nonsimultaneous acquisition of the 2 peaks precluded any reliable time-interval computation [32].
Also the time of first evaluation and diagnosis of heart failure and patient’s comorbidity (Table 2) may be of importance in the recurrence of hospitalization and death. So we decided to include diabetes and/or renal failure (defined as creatinine clearance <60 ml/min) as categorical covariates in the Cox analysis. There were no substantial changes in the final results, with age (p = 0.017), ischemic etiology (p = 0.007) and worsening in LV filling characteristics (ΔE/DT% p = 0.033) predicting HF exacerbations or death during follow-up. The statistical weight of ΔEDV20% decreased slightly (p = 0.068), There was no contribution at all from ΔESV% (p = 0.658), QRS duration (p = 0.533) and presence of diabetes and/or chronic renal insufficiency (p = 0.138).
Conclusions
Our study demonstrates that CRT improves systolic function and ventricular dyssynchrony and in particular it positively affects DF through a reverse remodeling process due to a left shifting towards a smaller equilibrium volume, with no change in the slope of EDPVR. Such evolution is associated with a favorable impact on the filling profile, although direct indexes of improved active relaxation are not significantly affected.
Finally, short-term changes in DF, together with ventricular volume shrinkage, rather than improvement in systolic function, predict clinical prognosis long-term post-CRT. Such a combination (improved filling coupled with reverse remodelling), rather than amelioration in systolic pump performance, seems to modulate long-term follow-up in these patients.
References
Dickstein K, Vardas PE, Auricchio A et al (2010) 2010 Focused update of ESC guidelines on device therapy in heart failure: an update of the 2008 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure and the 2007 ESC Guidelines for cardiac and resynchronization therapy. Eur Heart J 31:2677–2687
Packer M (1990) Abnormalities of diastolic function as a potential cause of exercise intolerance in chronic heart failure. Circulation 81(2 Suppl):III78–III86
Jansen AH, van Dantzig JM, Bracke F et al (2007) Improvement in diastolic function and left ventricular filling pressure induced by cardiac resynchronization therapy. Am Heart J 153:843–849
Waggoner AD, Faddis MN, Gleva MJ, de las Fuentes L, Dávila-Román VG (2005) Improvements in left ventricular diastolic function after cardiac resynchronization therapy are coupled to response in systolic performance. J Am Coll Cardiol 46:2244–2249
Yu CM, Zhang Q, Yip GW et al (2006) Are left ventricular diastolic function and diastolic asynchrony important determinants of response to cardiac resynchronization therapy? Am J Cardiol 98:1083–1087
Klotz S, Hay I, Dickstein ML et al (2006) Single-beat estimation of end-diastolic pressure–volume relationship: a novel method with potential for noninvasive application. Am J Physiol Heart Circ Physiol 291:H403–H412
Klotz S, Dickstein ML, Burkhoff D (2007) A computational method of prediction of the end-diastolic pressure–volume relationship by single beat. Nat Protoc 2:2152–2158
St John SM, Keane MG (2007) Reverse remodelling in heart failure with cardiac resynchronisation therapy. Heart 93:167–171
Marino P, Little WC, Rossi A et al (2002) Can left ventricular diastolic stiffness be measured noninvasively ? J Am Soc Echocardiogr 15:935–943
Nagueh SF, Appleton CP, Gillebert TC et al (2009) Recommendations for the evaluation of left ventricular diastolic function by echocardiography. Eur J Echocardiogr 10:165–193
Bertola B, Rondano E, Sulis M et al (2009) Cardiac dyssynchrony quantitated by time-to-peak or temporal uniformity of strain at longitudinal, circumferential and radial level: implications for resynchronization therapy. J Am Soc Echocardiogr 22:665–671
Nagueh SF, Middleton KJ, Kopelen HA, Zoghbi WA, Quiñones MA (1997) Doppler tissue imaging: a noninvasive technique for evaluation of left ventricular relaxation and estimation of filling pressures. J Am Coll Cardiol 30:1527–1533
Garcia MJ, Palac RT, Malenka DJ, Terrell P, Plehn JF (1999) Color M-mode Doppler flow propagation velocity is a relatively preload-independent index of left ventricular filling. J Am Soc Echocardiogr 12:129–137
Wang J, Khoury D, Trohan V, Torre-Amione G, Nagueh SF (2007) Global diastolic strain rate for the assessment of left ventricular relaxation and filling pressures. Circulation 115:1376–1383
Shanks M, Antoni ML, Hoke U et al (2011) The effect of cardiac resynchronization therapy on left ventricular diastolic function assessed with speckle-tracking echocardiography. Eur J Heart Fail 13:1133–1139
Cavallino C, Rondano E, Magnani A et al (2012) Baseline asynchrony, assessed circumferentially using temporal uniformity of strain, besides coincidence between site of latest mechanical activation and presumed left ventricular lead position, predicts favourable prognosis after resynchronization therapy. Int J Cardiovasc Imaging 28:1011–1021
Ypenburg C, van Bommel RJ, Delgado V et al (2008) Optimal left ventricular lead position predicts reverse remodeling and survival after cardiac resynchronization therapy. J Am Coll Cardiol 52:1402–1409
Mullens W, Borowski AG, Curtin RJ, Thomas JD, Tang WH (2009) Tissue Doppler imaging in the estimation of intracardiac filling pressure in decompensated patients with advanced systolic heart failure. Circulation 119:62–70
Burkhoff D (2013) Pressure–volume loops in clinical research. A contemporary view. J Am Coll Cardiol 62:1173–1176
Arshad A, Moss AJ, Foster E et al (2011) Cardiac resynchronization therapy is more effective in women than in man. The MADIT-CRT (Multicenter automatic defibrillator implantation trial with cardiac resynchronization therapy) trial. J Am Coll Cardiol 57:813–820
Aksoy H, Okutucu S, Kaya EB et al (2010) Clinical and echocardiographic correlates of improvement in left ventricular diastolic function after cardiac resynchronization therapy. Europace 12:1256–1261
Porciani MC, Valsecchi S, Demarchi G et al (2006) Evolution and prognostic significance of diastolic filling pattern in cardiac resynchronization therapy. Int J Cardiol 112:322–328
Leite-Moreira AF (2006) Current perspectives in diastolic dysfunction and diastolic heart failure. Heart 92:712–718
Aiba T, Hesketh GG, Barth AS et al (2009) Electrophysiological consequences of dyssynchronous heart failure and its restoration by resynchronization therapy. Circulation 119:1220–1230
Burkhoff D, Oikawa RY, Sagawa K (1986) Influence of pacing site on canine left ventricular contraction. Am J Physiol 251:H428–H435
Steendijk P, Tulner SA, Bax JJ et al (2006) Hemodynamic effects of long-term cardiac resynchronization therapy. Analysis by pressure–volume loops. Circulation 113:1295–1304
Yotti R, Bermejo J, Antoranz JC et al (2005) A noninvasive method for assessing impaired diastolic suction in patients with dilated cardiomyopathy. Circulation 112:2921–2929
Little WC (2005) Diastolic disfunction beyond distensibility. Adverse effects of ventricular dilatation. Circulation 112:2888–2890
Lamia B, Tanabe M, Tanaka H, Kim HK, Gorcsan J III, Pinsky MR (2011) Left ventricular systolic torsion correlates global cardiac performance during dyssynchrony and cardiac resynchronization therapy. Am J Physiol Heart Circ Physiol 300:H853–H858
Russel IK, Gotte MJW, De Roest GJ et al (2009) Loss of opposite left ventricular basal and apical rotation predicts acute response to cardiac resynchronization therapy and is associated with long-term reversed remodelling. J Cardiac Fail 15:717–725
Hasegawa H, Little WC, Ohno M, Brucks S, Morimoto A, Cheng HJ (2003) Diastolic mitral annular velocity during the development of heart failure. J Am Coll Cardiol 41:1590–1597
Kusunose K, Yamada H, Nishio S et al (2009) Clinical utility of single-beat E/e’ obtained by simultaneous recording of flow and tissue Doppler velocities in atrial fibrillation with preserved systolic function. J Am Coll Cardiol Img 2:1147–1156
Conflict of interest
There are no disclosures to be listed.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Facchini, E., Varalda, M., Sartori, C. et al. Systolic heart failure and cardiac resynchronization therapy: a focus on diastole. Int J Cardiovasc Imaging 30, 897–905 (2014). https://doi.org/10.1007/s10554-014-0412-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-014-0412-1