Abstract
Purpose
We examined whether diabetes and diabetes treatment are associated with MD in a cohort study of Danish women above age of 50 years.
Methods
Study cohort consisted of 5,644 women (4,500 postmenopausal) who participated in the Danish Diet, Cancer, and Health cohort (1993–1997) and subsequently attended mammographic screening in Copenhagen (1993–2001). We used MD assessed at the first screening after the cohort entry, defined as mixed/dense or fatty. Diabetes diagnoses and diabetes treatments (diet, insulin, or oral antidiabetic agents) were self-reported at the time of recruitment (1993–1997). The association between MD and diabetes was analyzed by logistic regression adjusted for potential confounders. Effect modification by menopausal status and body mass index (BMI) was performed by introducing an interaction term into the model and tested by Wald test.
Results
Of 5,644 women with mean age of 56 years, 137 (2.4%) had diabetes and 3,180 (56.3%) had mixed/dense breasts. Having diabetes was significantly inversely associated with having mixed/dense breasts, in both, the crude model (odds ratio; 95% confidence interval: 0.33; 0.23–0.48), and after adjustment for adiposity and other risk factors (0.61; 0.40–0.92). Similar inverse associations were observed for 44 women who controlled diabetes by diet only and did not receive any medication (0.56; 0.27–1.14), and 62 who took oral antidiabetic agents only for diabetes (0.59; 0.32–1.09), while women taking insulin had increased odds of mixed/dense breasts (2.08; 0.68–6.35). There was no effect modification of these associations by menopausal status or BMI.
Conclusions
Having diabetes controlled by diet or oral antidiabetic agents is associated with a decrease in MD, whereas taking insulin is associated with an increase in MD.
Similar content being viewed by others
Introduction
Numerous studies have demonstrated an association between type 2 diabetes and breast cancer [1–3]. A meta-analysis found a 27% increase in breast cancer risk in women with type 2 diabetes, which attenuated to 13% when adjusting for body mass index (BMI) [3]. Type 1 diabetes patients have no increased risk of breast cancer [4]. Exact biological mechanisms behind possible association between type 2 diabetes and breast cancer are unknown, and the relationship is complicated since diabetes and breast cancer share many risk factors including physical inactivity and obesity. Possible mechanisms include direct effects of hyperinsulinemia or the insulin-like growth factor (IGF) system on stimulating cell proliferation, as well as indirect effects mediated through altered levels of sex hormones [3]. Treatments which elevate circulating insulin levels in people with diabetes may increase cancer risk, and insulin analog glargine has been associated with higher risk of breast cancer than human insulin [5]. On the other hand, metformin, commonly prescribed used oral antidiabetic regimen, which increases insulin sensitivity and improves glycemic control, has been found to reduce breast cancer risk [6]. However, a large European study found no overall increase in breast cancer for type two diabetic patients, irrespective of type of treatment: sulfonylurea (hazard ratio (HR): 0.98), metformin (HR: 0.90), or insulin (HR: 1.07) [7].
One possible pathway from type 2 diabetes or diabetes treatment to breast cancer could be via an intermediary such as mammographic density (MD), one of the strongest risk factors for breast cancer [8]. MD refers to the amount of radiologically dense breast consisting of epithelial or stromal tissue that appears light on a mammogram [9]. Women with more than 75% density in the breast have a four to six times greater risk of breast cancer than women with little density, or fatty breasts [10]. Known determinants of MD include age at first birth, parity, age at menopause, hormone therapy (HT), all of which are estrogen-related, having a proliferative effect on fibroglandular tissue in the breast, increasing MD [10]. Use of chemopreventive agents, such as tamoxifen, can reduce MD [10]. Obesity, on the other hand, which increases the risk of postmenopausal breast cancer, likely via insulin as a mediator, decreases MD [10]. Only four studies examined the association between self-reported diabetes and MD [11–14], of which three reported slightly lower percent MD (PMD) in diabetic as compared to non-diabetic women [11–13], while a single study found statistically significant inverse association between diabetes and MD in premenopausal, but not in postmenopausal women [14]. No study to date had examined whether effect of diabetes on MD is differential by the type of treatment for diabetes.
Here we examined whether diabetes and diabetes treatment are associated with MD in a prospective cohort study of Danish women above age of 50 years.
Methods
Study population
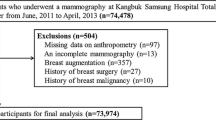
The study population consists of 5,703 women above age 50 who participated in the Danish Diet, Cancer, and Health (DCH) cohort between 1993 and 1997 and subsequently attended the Copenhagen mammography screening program between 1993 and 2001.
DCH cohort
Between 1993 and 1997, a total of 160,725 persons (72,729 women), 50–64 years of age, born in Denmark, living in Copenhagen or Aarhus (the two largest cities in Denmark), and free of cancer, were invited to participate in the DCH cohort study. A total of 57,053 people, of whom 29,875 were women (37% of invited women and 7% of entire Danish female population in this age group), accepted the invitation and participated in the study, answering a comprehensive questionnaire on diet, health, education, occupation, lifestyle, and reproductive factors. Height and weight were measured at the time of recruitment by a trained professional staff. Women were defined as premenopausal if they reported no HT use and at least 1 instance of menstruation ≤12 months before the time of recruitment, and postmenopausal otherwise. A detailed description of the DCH cohort has been published previously [15].
Diabetes definition
Diabetes diagnosis (yes/no), age at diagnoses (years), and form of treatment for diabetes (diet regulated, insulin, or oral antidiabetic agents) were self-reported at the time of recruitment (1993-1997) in the DCH cohort. We defined diabetes as indicator (yes/no) of either having a diagnosis of diabetes or being treated for diabetes (diet, insulin or oral antidiabetic agents). Furthermore, we defined the three indicators of treatment for diabetes: diabetes controlled by diet only, insulin only, or oral antidiabetic agents only. We could not distinguish between type 1 and type 2 diabetes.
Danish Copenhagen mammography register
The Copenhagen mammography screening program started in 1991 [16] and targeted approximately 40,000 women aged 50–69 years at the start of each biennial invitation round. We used data from the first five screening rounds between 1991 and 2001 [17]. Cases in which breast cancer was detected at the first screening were excluded from our final analytic data set, as these women lacked MD data.
MD definition
One radiologist was in charge of the Copenhagen mammography screening program between 1991 and 2001 which took place at a single Copenhagen hospital, Rigshospitalet. All screens were taken by the radiographers or X-ray nurses, and were evaluated independently by two radiologists, who did not meet the attending women. A two-view mammography, craniocaudal and oblique, was performed at the initial screening. MD was dichotomized into fatty breast, equivalent to Breast Imaging Reporting and Data System (BI-RADS, Atlas, 2008) density code one and part of code two, and mixed/dense breast, equivalent to part of BI-RADS code two, and BI-RADS code three or four. Women with a negative screening test and fatty breasts were scheduled to have only an oblique view at their next screening, whereas women with a negative screening test and mixed/dense breasts were scheduled for another two-view mammogram. MD was not coded for positive screening mammograms. The dichotomous outcome for MD has been successfully utilized in earlier studies, showing the expected associations with breast cancer risk [17] and validated against BI-RADS density scores, with good agreement [18]. Using the personal identification number (CPR) of the Danish Civil Registration System [19], we linked the Copenhagen mammography register to the DCH cohort. We used MD assessed at the first screening after the cohort baseline (1993–1997).
Statistical methods
We used logistic regression to investigate the association between diabetes and the three possible diabetes treatments (diet regulated/insulin/oral antidiabetic agents) and MD in separate models, and in four steps: crude model (Model 1); a model adjusted for age (Model 2); a Model 2 additionally adjusted for BMI (kg/m2) and waist circumference (cm) (Model 3), and Model 3 additionally adjusted for education (≤7 years/8–10 years/> 10 years), alcohol use (yes/no), alcohol intake (g/day), smoking (current/ever/never), physical activity in leisure time (yes/no), number of children, benign breast tumor (yes/no), and HT use (ever/never) (Model 4). We did not have data on chemopreventive agents in this cohort and did not include age at first birth and menopausal status in the model, as large number of women had missing data for these variables, 1,325 and 996, respectively. Analyses were stratified by menopausal status, overweight (BMI ≥ 25) and obesity (BMI ≥ 30). Effect modification of an association of MD with diabetes by menopausal status, overweight (BMI ≥ 25), and obesity (BMI ≥ 30) was analyzed by introducing an interaction term into the model and tested by Wald test. Logistic procedure in Stata 12.0 was used to conduct the analyses. Results are presented as odds ratios (ORs) with 95% confidence intervals (95% CI). We have run an additional model with diabetes defined as diabetes with onset after age 30 years, which could considered likely to be type two diabetics (excluding likely type 1 diabetes patients who typically are diagnosed before age 30 years).
Results
Of 5,703 women in the study, we excluded 59 with missing data on one or more covariates, leaving 5,644 women for final analyses. Of these, 137 (2.4%) women had reported having diabetes at cohort baseline, 44 did not receive any medication and controlled diabetes by diet only, 62 took oral antidiabetic agents only, and 20 took insulin only, while 11 women answered that they used two regimens for treating diabetes, and were thus not included in the specific regimen analyses. The majority of women (56.3%) had mixed/dense breasts at their mammogram, which was taken at screening on average 1.1 years after the cohort baseline (93% had their mammogram within 2 years after baseline).
Mean age at baseline was 56 years, and 4,500 (79.7%) women were postmenopausal (Table 1). Mean BMI at baseline was 25.9 kg/m2, half (51.1%) of the women were overweight (BMI ≥ 25 kg/m2), and 16.7% were obese (BMI ≥ 30 kg/m2). Women with mixed/dense breasts were younger and had lower BMI than women with fatty breasts (Table 1). Mean age at diabetes diagnoses was 52.8 years, 59.5 years for women regulating diabetes by diet, 53.6 years for women taking oral antidiabetic agents, and 41.2 years for women taking insulin (Table 2). A total of 121 women received a diagnosis after age 30, which is considered to be most likely type 2 diabetes (Table 2), and in this group, age of onset of diabetes was 51.3 years for those taking insulin. Diabetic women taking insulin had lower BMI (24.0 kg/m2) than women regulating diabetes by diet (31.0 kg/m2) or taking oral antidiabetic agents (30.6 kg/m2). Of 16 who were diagnosed with diabetes before age 30 and had likely type 1 diabetes, seven had mixed/dense and five had fatty breasts (results not shown).
We found statistically significant inverse association between having diabetes and MD in a crude model (OR; 95% CI: 0.33; 0.23–0.48), which attenuated after adjustment for risk factors, especially adiposity, but remained statistically significant (0.61; 0.40–0.92) (Table 3). Similar inverse associations, although not statistically significant, were observed for women with diabetes controlled by diet only (0.56; 0.27–1.14), and for women taking oral antidiabetic agents only (0.59; 0.32–1.09) in the fully adjusted model. For women with diabetes taking insulin, we found a positive association with MD in all models, although statistically non-significant, due to small numbers (2.08; 0.68–6.35). Associations between diabetes and MD were slightly enhanced when limiting analyses to women with diabetes onset after age 30 (0.55; 0.35–0.87), mostly for women controlling diabetes by diet only (0.36; 0.15–0.86), while they remained unchanged for women taking oral antidiabetic agents (0.59; 0.31–1.13), and were slightly reduced for women taking insulin (2.01; 0.55–7.44), but there was no statically significant difference with estimates for all diabetes, regardless of age at onset (Table 3).
In stratified analyses, we found that there was no difference in association between diabetes and MD by menopausal status, or BMI (Table 4).
Discussion
In this study, we present novel results of the differential association between diabetes and MD by diabetes treatment. Inverse associations between diabetes and MD were observed for women who controlled diabetes with diet or oral antidiabetic agents, while women taking insulin showed a positive association with having mixed/dense breasts, though statistically non-significant.
Our results generally agree with four studies on diabetes prevalence and MD, although differences in study design, study populations, and MD assessment preclude direct comparisons. The study by Tehranifar et al. [11] is a cross-sectional study from the New York Multiethnic Breast Cancer Project based on 124 pre- and 67 postmenopausal women with data on PMD, of whom 16 reported having type 2 diabetes. Mammograms were collected on the same date or 14 days after the interview. Diabetic women had slightly lower PMD than non-diabetic women, but the difference was not statistically significant [11]. Sellers et al. [12] utilized data from the Minnesota Breast Cancer Family Study Cohort to examine the association of PMD assessed shortly after interview in 2,530 women above age 40, where 161 reported diabetes, and found no statistically significant association, although mean PMD was slightly lower in diabetic women than in women without diabetes. Sanderson et al. [13] has in 476 black American women recruited at Meharry Medical College detected a lower percent breast density in 373 women with diabetes than in those without diabetes, but only in premenopausal women and without statistical significance, and no difference in postmenopausal women. Finally, Roubidoux et al. investigated the association between self-reported diabetes (n = 152) with MD available as BIRADS density scores among 144 pre- and 311 postmenopausal Southwestern Native American women, and found that diabetes was statistically significantly associated with lower BIRADS density in premenopausal women only, but found no association in postmenopausal women [14]. We found inverse, statistically significant associations between having diabetes and MD, in both pre- and postmenopausal women, although with slightly stronger associations in premenopausal women, in agreement with Sanderson et al. [13] and Roubidoux et al. [14]. Overall, evidence seems consistent that women with diabetes have less dense breasts than women without diabetes, in studies that control for BMI and adiposity. Diabetes reduces breast density, which is one of the strongest risk factors for breast cancer [10], but it, independently of breast density, increases the risk of breast cancer. The mechanisms by which type 2 diabetes increases the risk of breast cancer are not known, but several pathways are possible. Type 2 diabetes causes hyperglycemia, hyperinsulinemia, and increased inflammation, all of which may increase risk of breast cancer [1–3]. In addition, type 2 diabetes and breast cancer share many risk factors, including age, physical inactivity, overweight, and obesity, which may separately or together, increase risk of breast cancer in postmenopausal women with diabetes [1–3]. Overweight and obesity, for example, as type 2 diabetes, are associated with decrease in breast density [10], but increase in breast cancer risk in postmenopausal women.
We present the novel results that the association between diabetes and MD is differential with respect to type of treatment for diabetes. We found that women who take insulin have likely increased, whereas women taking oral antidiabetic agents or not taking any mediation have strongly decreased breast density, compared to women without diabetes. The exact biological mechanism behind these novel findings are not known, but some plausibility for the findings comes from existing evidence on associations between different diabetes treatment and breast cancer. Earlier studies have shown that insulin, a debated risk factor for breast cancer [4, 20], can stimulate cell proliferation in human breast cancer cell lines [21] and also in normal breast tissue [22, 23]. Thus, it is plausible that insulin can increase the amount of fibroglandular tissue in the breast, hence increasing MD [3, 20]. Several small studies examined association between fasting circulating insulin plasma levels and MD and found none, but have typically included healthy women without diabetes [24, 25]. Metformin, a biguanide, is the most commonly used oral medication for first-line treatment of diabetes. Metformin has multiple biological effects which can contribute to anticancer effects, including either direct antiproliferative effects or through indirect mechanisms, such as lowering of circulating insulin levels and improving glycemic control in diabetes patients [26]. In line with these physiological effects, metformin was found to lower postmenopausal breast cancer risk in some [6, 27] but not all studies [7]. Furthermore, metformin can reduce circulating androgen and estrogen levels [28]. Thus, it is plausible that metformin, by reducing levels of endogenous estrogen and cell proliferating insulin, can reduce MD. However, we found similar effect of decreased MD on both groups of women taking oral antidiabetic agents and regulating diabetes by diet only, precluding the conclusion that metformin alone can decrease MD, but rather suggesting that some other factor or characteristic common to both groups of diabetic women who did not take insulin contributes to lower MD.
This study benefited from having access to a large cohort of women with self-reported diabetes at recruitment in 1993–1999 as well as subsequent and independent collection of data on MD at breast cancer screening, facilitating the prospective design and limiting the possibility of recall or information bias. We had data and were able to adjust for all major diabetes and breast cancer risk factors and determinants of MD. Unlike any study before [11–14], we had objectively measured data on height and weight (BMI) and waist circumference, and were thus able to extensively adjust for adiposity, which is an important risk factor for diabetes and very important determinant for MD, as shown in Table 2. A major strength of this study is also the availability of information on diabetes treatment regiments, enabling us to examine the effect of diabetes regiments on MD for the first time. Furthermore, this is one of the largest studies to date on diabetes and MD, and perhaps the first study with enough power to detect statistically significant inverse associations between diabetes and MD, in contrast to earlier, smaller studies of typically few hundred patients [11–14]. Still, based on 137 diabetes cases, we still had limited power in the effect modification analyses. The main limitation is the possible misclassification of diabetes treatment, which is self-reported, as well as the small number of diabetes cases, limiting the power in analyses of diabetes treatment. Furthermore, we could not distinguish between type one and type 2 diabetes, but we found consistent results in a subset of women who most likely had type 2 diabetes (those with onset of diabetes above age 30 years). We also lacked the data on the specific type of insulin or oral antidiabetic agent regiments, although most of the patients in Denmark are prescribed metformin as oral diabetic agent. Recent report based on national data in Denmark between 2005 and 2012 showed that 81% of type 2 diabetes patients received metformin as their first antidiabetic medication, 13% started with sulfonylurea, and 6% with insulin [29]. We excluded women with positive outcome at the initial breast cancer screening, as they were not assigned MD, but instead referred to additional testing, by which we have likely excluded women with high MD, which is associated with breast cancer and low screening sensitivity. Another weakness is that DCH cohort participants are likely healthier than the general Danish population, implying some healthy worker effect, as it was shown that they are better educated and had higher income than non-participants [15]. Another limitation is that diabetes is self-reported, and likely underreported. However, self-reported diabetes prevalence in this cohort of 2.4% corresponds well to diabetes prevalence data for entire Denmark, based on Danish Diabetes register, which ranged from 1995 (first data in register) to 1997, in women, from 1.9 to 2.4%, [30].
In conclusion, we found that diabetic women had lower MD than women without diabetes, but that the association was differential by type of diabetes regimen. Having diabetes controlled by diet or oral antidiabetic agents seems to decrease, whereas taking insulin may increase MD. This information is important for women taking insulin and clinicians working with diabetes and breast cancer screening. Women with type 2 diabetes are at increased risk of breast cancer and have poorer prognosis of breast cancer [31], and as high risk group may have an added benefit from attending breast cancer screening and detecting cancer early. However, women with diabetes participate less in breast cancer screening than women from general population, and seem to miss out on the screening benefits [31]. Furthermore, increase in MD in women taking insulin may reduce the sensitivity of the screening in this group of diabetic women, as breast cancer screening performance decreases with increasing breast density [32]. Thus, diabetic women may benefit from better information on benefits of breast cancer screening, and the effect of their diabetes treatment regimen on breast density and related cancer screening performance, all of which may reduce breast cancer burden in this group of women. More research is needed to reproduce findings of this novel study.
Abbreviations
- MD:
-
mammographic density
- HT:
-
hormone therapy
- CPR:
-
Danish personal identification number
- DCH:
-
Diet, Cancer, and Health cohort
- BI-RADS:
-
Breast Imaging Reporting and Data System
- OR:
-
odds ratio
- CI:
-
confidence interval
- BMI:
-
body mass index
References
De Bruijn KM, Arends LR, Hansen BE, Leeflang S, Ruiter R, van Eijck CH (2013) Systematic review and meta-analysis of the association between diabetes mellitus and incidence and mortality in breast and colorectal cancer. Br J Surg 100:1421–1429
Hardefeldt PJ, Edirimanne S, Eslick GD (2012) Diabetes increases the risk of breast cancer: a meta-analysis. Endocr Relat Cancer 19:793–803
Boyle P, Boniol M, Koechlin A, Robertson C, Valentini F, Coppens K, Fairley LL, Boniol M, Zheng T, Zhang Y, Pasterk M, Smans M, Curado MP, Mullie P, Gandini S, Bota M, Bolli GB, Rosenstock J, Autier P (2012) Diabetes and breast cancer risk: a meta-analysis. Br J Cancer 107:1608–1617
Liaw YP, Ko PC, Jan SR, Huang JY, Nfor ON, Lung CC, Chiang YC, Yeh LT, Chou MC, Tsai HD, Hsiao YH (2015) Implications of type1/2 diabetes mellitus in breast cancer development: a general female population-based cohort study. J Cancer 6:734–739
Karlstad O, Starup-Linde J, Vestergaard P, Hjellvik V, Bazelier MT, Schmidt MK, Andersen M, Auvinen A, Haukka J, Furu K, de Vries F, De Bruin ML (2013) Use of insulin and insulin analogs and risk of cancer: systematic review and meta-analysis of observational studies. Curr Drug Saf 8:333–348
Col NF, Ochs L, Springmann V, Aragaki AK, Chlebowski RT (2012) Metformin and breast cancer risk: a meta-analysis and critical literature review. Breast Cancer Res Treat 135:639–646
Currie CJ, Poole CD, Gale EAM (2009) The influence of glucose-lowering therapies on cancer risk in type 2 diabetes. Diabetologia 52:1766–1777
McCormack VA, dos SS I (2006) Breast density and parenchymal patterns as markers of breast cancer risk: a meta-analysis. Cancer Epidemiol Biomark Prev 15:1159–1169
Boyd NF, Guo H, Martin LJ, Sun L, Stone J, Fishell E, Jong RA, Hislop G, Chiarelli A, Minkin S, Yaffe MJ (2007) Mammographic density and the risk and detection of breast cancer. N Engl J Med 356:227–236
Boyd NF, Martin LJ, Yaffe MJ, Minkin S (2011) Mammographic density and breast cancer risk: current understanding and future prospects. BCR 13:223
Tehranifar P, Reynolds D, Fan X, Boden-Albala B, Engmann NJ, Flom JD, Terry MB (2014) Multiple metabolic risk factors and mammographic breast density. Ann Epidemiol 24:479–483
Sellers TA, Jensen LE, Vierkant RA, Fredericksen ZS, Brandt KR, Giuliano AR, Pankratz VS, Cerhan JR, Vachon CM (2007) Association of diabetes with mammographic breast density and breast cancer in the Minnesota breast cancer family study. Cancer Causes Control 18:505–515
Sanderson M, O’Hara H, Foderingham N, Dupont WD, Shu XO, Peterson N, Fair AM, Disher AC (2015) Type 2 diabetes and mammographic breast density among underserved women. Cancer Causes Control 26:303–309
Roubidoux MA, Kaur JS, Griffith KA, Sloan J, Wilson C, Novotny P, Lobell M (2003) Correlates of mammogram density in southwestern Native-American women. Cancer Epidemiol Biomark Prev 12:552–558
Tjonneland A, Olsen A, Boll K, Stripp C, Christensen J, Engholm G, Overvad K (2007) Study design, exposure variables, and socioeconomic determinants of participation in Diet, Cancer and Health: a population-based prospective cohort study of 57,053 men and women in Denmark. Scand J Public Health 35:432–441
Vejborg I, Olsen AH, Jensen MB, Rank F, Tange UB, Lynge E (2002) Early outcome of mammography screening in Copenhagen 1991–99. J Med Screen 9:115–119
Olsen AH, Bihrmann K, Jensen MB, Vejborg I, Lynge E (2009) Breast density and outcome of mammography screening: a cohort study. Br J Cancer 100:1205–1208
Hodge R, Hellmann SS, Mv Euler-Chelpin, Vejborg I, Andersen ZJ (2014) Comparison of Danish dichotomous and BI-RADS classifications of mammographic density. Acta Radiol Short Rep 3(5):2047981614536558
Pedersen CB (2011) The Danish civil registration system. Scand J Public Health 39:22–25
Gunter MJ, Hoover DR, Yu H, Wassertheil-Smoller S, Rohan TE, Manson JE, Li J, Ho GY, Xue X, Anderson GL, Kaplan RC, Harris TG, Howard BV, Wylie-Rosett J, Burk RD, Strickler HD (2009) Insulin, insulin-like growth factor-I, and risk of breast cancer in postmenopausal women. J Natl Cancer Inst 7:48–60
Chappell J, Leitner JW, Solomon S, Golovchenko I, Goalstone ML, Draznin B (2001) Effect of insulin on cell cycle progression in MCF-7 breast cancer cells. Direct and potentiating influence. J Biol Chem 276:38023–38028
Ish-Shalom D, Christoffersen CT, Vorwerk P, Sacerdoti-Sierra N, Shymko RM, Naor D, De Meyts P (1997) Mitogenic properties of insulin and insulin analogues mediated by the insulin receptor. Diabetologia 40:S25–S31
Borugian MJ, Spinelli JJ, Gordon PB, Abanto Z, Brooks-Wilson A, Pollak MN, Warren LJ, Hislop TG, Gallagher RP (2014) Fasting insulin and endogenous hormones in relation to premenopausal breast density (Canada). Cancer Causes Control 25:385–394
Woolcott CG, Courneya KS, Boyd NF, Yaffe MJ, McTiernan A, Brant R, Jones CA, Stanczyk FZ, Terry T, Cook LS, Wang Q, Friedenreich CM (2013) Association between sex hormones, glucose homeostasis, adipokines, and inflammatory markers and mammographic density among postmenopausal women. Breast Cancer Res Treat 139:255–265
Wolin KY, Colangelo LA, Chiu BC, Ainsworth B, Chatterton R, Gapstur SM (2007) Associations of physical activity, sedentary time, and insulin with percent breast density in Hispanic women. J Womens Health 16:1004–1011
Pollak M (2010) Metformin and other biguanieds in oncology; advancing the research agenda. Cancer Prev Res 3:1060–1065
Gandini S, Puntoni M, Heckman-Stoddard BM, Dunn BK, Ford L, DeCensi A, Szabo E (2014) Metformin and cancer risk and mortality: a systematic review and meta-analysis taking into account biases and confounders. Cancer Prev Res 7:867–885
Campagnoli C, Berrino F, Venturelli E, Abbà C, Biglia N, Brucato T, Cogliati P, Danese S, Donadio M, Zito G, Pasanisi P (2013) Metformin decreases circulating androgen and estrogen levels in nondiabetic women with breast cancer. Clin Breast Cancer 13:433–438
Mor A, Petersen I, Sørensen HT, Thomsen RW (2016) Metformin and other glucose-lowering drug initiation and rates of community-based antibiotic use and hospital-treated infections in patients with type 2 diabetes: a Danish nationwide population-based cohort study. BMJ Open 6:e011523
Carstensen B, Kristensen JK, Ottosen P, Borch-Johnsen K, Steering Group of the National Diabetes Register (2008) The Danish National Diabetes Register: trends in incidence, prevalence and mortality. Diabetologia 51:2187–2196
Onitilo AA, Engel JM, Glurich I, Stankowski RV, Williams GM, Doi SA (2012) Diabetes and cancer I: risk, survival, and implications for screening. Cancer Causes Control 23:967–981
van der Waal D, Ripping TM, Verbeek AL, Broeders MJ (2016) Breast cancer screening effect across breast density strata: A case–control study. Int J Cancer. doi:10.1002/ijc.30430
Acknowledgments
Not applicable.
Authors’ Contributions
All authors made substantial contributions to conception and design, analysis, and interpretation of data, and critical review of the manuscript. ZJA conceived the study, participated in its design and coordination, performed the statistical analysis and helped to draft the manuscript. KB contributed to the design of the study and helped drafting the manuscript. KT carried out the literature review for the study and helped to draft the manuscript. EL, MEC, and AT have been involved in revising the manuscript critically for important intellectual content. All authors read and approved the final manuscript.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Informed consent
The study was entirely based on a data from registers and approved by the Danish Data Inspection Agency by Danish law serving as ethical approval of register-based research, which does not require an informed consent from study participants. Thus, no contact has been made with participating women, relatives, or their practicing doctors, and no consent was needed.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Buschard, K., Thomassen, K., Lynge, E. et al. Diabetes, diabetes treatment, and mammographic density in Danish Diet, Cancer, and Health cohort. Cancer Causes Control 28, 13–21 (2017). https://doi.org/10.1007/s10552-016-0829-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-016-0829-z