Abstract
In 1991, California transferred significant responsibility, resources, and accountability for public mental health from the state to its 58 counties. Using purposeful sampling, we conducted in-depth interviews with ten senior state and county leaders to gain insights into the relatively uncharted area of their understanding of this legislation’s intent, development, and long-term consequences. While realignment secured funding for the system and provided incentives and flexibility for counties to move toward providing more community-based care, the decision to base realignment allocations on counties’ historical spending along with minimal payments to address differences helped to institutionalize spending disparities. Results of this study can inform how we develop and implement decentralization policies.
Similar content being viewed by others
Notes
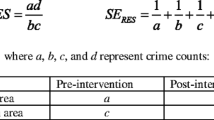
Through Realignment, counties receive revenues equal to the previous year’s total. Growth funds from a sales tax account are first given to caseload-driven social service programs (Legislative Analyst’s Office, 2001). Any remaining growth from the sales tax account and all vehicle license fees (the funding mechanisms for Realignment) are distributed to counties. The balance was given to “under-equity” counties, which received a state mental health financing supplement. To determine under-equity status, a population-poverty measure for each county was calculated by taking the average of two metrics—(1) the county’s portion of the statewide population and (2) the county’s portion of the State’s Supplemental Security Income (SSI) and Aid to Families with Dependent Children (AFDC) recipients (Masland 1997, p. 33). If a county’s population-poverty portion was greater than the portion of the statewide Realignment base it received, it was considered an under-equity county (Department of Mental Health 2003, p. 6).
References
Aberbach, J. D., & Rockman, A. (2002). Conducting and coding elite interviews. Political Science and Politics, 35(4), 673–676. doi:10.1017/S1049096502001142.
Aday, L. A., Begley, C. E., Lairson, D. R., & Balkrishnan, R. (2004). Evaluating the health care system: Effectiveness, efficiency, and equity. Chicago, IL: Health Administration Press.
Berry, J. M. (2002). Validity and reliability issues in elite interviewing. Political Science and Politics, 35(4), 679–682. doi:10.1017/S1049096502001166.
Bronzan-McCorquodale Act, Ch. 89, 1991 Cal. Stat. 303.
Brown, E.G., Jr. (2011). 2011–2012 governor’s budget summary. Retrieved from http://www.dof.ca.gov/budget/historical/2011-12/governors/summary/documents/2011-12_Budget_Summary-State_of_California.pdf. Accessed 26 Aug 2014.
Center on Budget and Policy Priorities. (2011). Medicaid block grant would produce disparate and inequitable results across states. Retrieved from http://www.cbpp.org/cms/index.cfm?fa=view&id=3422.
Community Mental Health Service Act (1957) (Short-Doyle Act), Ch. 1989, Cal. Stat. 3535.
Department of Health Care Services. (2014). Performance outcomes system implementation plan for Medi-Cal specialty mental health services for children & youth. Retrieved from http://www.dhcs.ca.gov/formsandpubs/Documents/Legislative%20Reports/Mental%20Health/SMHSPerf_Outcomes_System-Jan2014.pdf.
Department of Mental Health. (2003). AB 328 Realignment data report as required by AB 328 and AB 2044. Sacramento, CA: State of California Department of Mental Health.
Dey, I. (1999). Grounding grounded theory: Guidelines for qualitative inquiry. San Diego, CA: Academic Press.
Frank, R., & Gaynor, M. (1994). Fiscal decentralization of public mental health and the Robert Wood Johnson Foundation Program on chronic mental illness. The Milbank Quarterly, 72(1), 81–104. doi:10.2307/3350339.
Harvey, W. S. (2011). Strategies for conducting elite interviews. Qualitative Research, 11(4), 431–441. doi:10.1177/1468794111404329.
Hesse-Biber, S. N., & Leavy, P. (2006). The practice of qualitative research. Thousand Oaks, CA: Sage Publications Inc.
Holahan, J., Weil, A., & Wiener, J. M. (Eds.). (2003). Federalism and health policy. Washington, DC: The Urban Institute Press.
HyperRESEARCH. (Version 3.5.2) [Computer Software]. Randolph, MA: ResearchWare, Inc.
Initiative Measure (Prop. 63, approved Nov. 2, 2004), Mental Health Services Act of 2004. Lanterman-Petris-Short Act, Ch. 1667, 1967 Cal. Stat. 4074.
Leech, B. L. (2002a). Asking questions: Techniques for semistructured interviews. Political Science and Politics, 35(4), 665–668. doi:10.1017/S1049096502001129.
Leech, B. L. (2002b). Interview methods in political science. Political Science and Politics, 35(4), 663–664. doi:10.1017/S1049096502001117.
Legislative Analyst’s Office. (2001). Realignment revisited: an evaluation of the 1991 experiment in state-county relations. Retrieved from http://www.lao.ca.gov/2001/realignment/020601_realignment.html.
Lehman, A. F., Postrado, L. T., Roth, D., McNary, S. W., & Goldman, H. H. (1994). Continuity of care and client outcomes in the Robert Wood Johnson Foundation Program on Chronic Mental Illness. The Milbank Quarterly, 72(1), 105–122. doi:10.2307/3350340.
Masland, M. C. (1997). Local variation in response to decentralization of authority in California’s public mental health system (Doctoral dissertation). Retrieved from ProQuest Dissertations & Theses database (Order No. 9827030).
Morrissey, J. P., Calloway, M., Bartko, W. T., Ridgely, M. S., Goldman, H. H., & Paulson, R. I. (1994). Local mental health authorities and service system change: Evidence from the Robert Wood Johnson Foundation Program on Chronic Mental Illness. The Milbank Quarterly, 72(1), 49–80. doi:10.2307/3350338.
Oates, W. E. (1999). An essay on fiscal federalism. American Economic Association, 37(3), 1120–1149. Retrieved from: http://www.jstor.org/stable/2564874.
Palinkas, L. A., Horwitz, S. M., Green, C. A., Wisdom, J. P., Duan, N. & Hoagwood, K. (2013). Purposeful sampling for qualitative data collection and analysis in mixed method implementation research. Administration and Policy in Mental Health and Mental Health Services Research. Advance online publication. doi:10.1007/s10488-013-0528-y.
Patient Protection and Affordable Care Act, Pub. L. No. 111-148, 124 Stat. 119 (2010), as amended by the Health Care and Education Act of 2010, Pub. L. No. 111–152, 124 Stat. 1029 (2010).
Patton, M. Q. (2002). Qualitative research and evaluation methods (3rd ed.). Thousand Oaks, CA: Sage.
Roy, A. (2012). Why block-granting Medicaid will result in better health care for the poor. Forbes. Retrieved September 30, 2012 from http://www.forbes.com/sites/aroy/2012/09/30/why-block-granting-medicaid-will-result-in-better-health-care-for-the-poor/.
Ryan, P. (n.d.). California mental health financing 101: The Mental Health Services Act in the context of overall county mental health financing pressures [PowerPoint presentation]. Retrieved from http://www.mhsoac.ca.gov/Meetings/docs/Meetings/2006/CalifMHFinancing101.pdf.
Scheffler, R., & Smith, R. B. (2006). The impact of government decentralization on county health spending for the uninsured in California. International Journal of Health Care Finance and Economics, 6(3), 237–258. doi:10.1007/s10754-006-9003-6.
Scheffler, R. M., Wallace, N. T., Hu, T. W., Garrett, A. B., & Bloom, J. R. (2000). The impact of risk shifting and contracting on mental health service costs in California. Inquiry 37(2), 121–133. Retrieved from http://www.jstor.org/stable/29772885.
Scheffler, R., Zhang, A., & Snowden, L. (2001). The impact of realignment on utilization and cost of community-based mental health services in California. Administration and Policy in Mental Health, 29(2), 129–143. doi:10.1023/A:1014336530490.
Shapiro, D. L. (1995). Federalism: A dialogue. Evanston, IL: Northwestern University.
Snowden, L., Scheffler, R., & Zhang, A. (2002). The impact of realignment on the client population in California’s public mental health system. Administration and Policy in Mental Health, 29(30), 229–241. doi:10.1023/A:1015191425834.
Sosin, M. R. (1990). Decentralizing the social service system: A reassessment. Social Service Review, 64(4), 617–636. Retrieved from http://www.jstor.org/stable/30000977.
Soss, J., Fording, R. C., & Schram, S. F. (2011). Disciplining the poor: Neoliberal paternalism and the persistent power of race. Chicago: The University of Chicago Press.
Stone, D. (2002). Policy paradox: The art of political decision making, revised edition. New York, NY: W. W. Norton & Company.
Scheffler R., Wallace, N., Hu, T. W., Bloom, J. & Garrett, B. (1998). The effects of decentralisation on mental health costs in California. Mental Health Research Review, 5, 31–32. Retrieved from http://www.pssru.ac.uk/archive/pdf/mhrr5.pdf.
The Kaiser Family Foundation, The Kaiser Commission on Medicaid and the Uninsured. (2011). Mental health financing in the United States: A primer. Retrieved from http://kaiserfamilyfoundation.files.wordpress.com/2013/01/8182.pdf.
Weiss, R. S. (1994). Learning from strangers: The art and method of qualitative interview studies. New York: The Free Press.
Zhang, A., Scheffler, R., & Snowden, L. (2000). State health care reform: The effects of program realignment on severely mentally ill persons in California’s community-based mental health system. Psychiatric Services, 51(9), 1103–1106. doi:10.1176/appi.ps.51.9.1103.
Acknowledgments
The authors would like to thank the interviewees for their time and insights. Dr. Vanneman gratefully acknowledges funding for her dissertation work from UC Berkeley’s Graduate Division and the School of Public Health, California Program on Access to Care (CPAC). This paper is also the result of work supported with resources and the use of facilities at the VA Palo Alto Health Care System as well as a postdoctoral fellowship from the VA Office of Academic Affiliations. The views expressed in this paper are those of the authors and do not necessarily reflect the position or policy of CPAC, UC Berkeley, the Regents of the University of California, Stanford University, the Department of Veterans Affairs, or the United States government.
Author information
Authors and Affiliations
Corresponding author
Additional information
Parts of this paper were presented in a poster at the 2014 Annual Research Meeting for AcademyHealth.
Appendix
Appendix
Historical Informant In-Depth Interview Guide
Background
-
(1)
Could you start off by giving me a little background on yourself? What was your path to the position you have now?
-
(2)
My research focuses on the public mental health system and care for children, youth, and young adults since the early 1990s. Since that time, what do you see as the major changes to the public mental health system that have affected children, youth, and young adults?
Probes:
Financially?
In the delivery of care?
For populations served?
-
(3)
Have any state or county policies been significant in catalyzing these changes? If yes, which ones, and how?
Probes:
1991 Realignment?
Systems of Care (1984–1998)?
EPSDT expansion/T.L. v. Belshe lawsuit (1995)?
Medi-Cal mental health services “carve out” (1995)?
County mental health plans (1995)?
Medi-Cal consolidation (1997–1998)?
Mental Health Services Act (2004)?
2011–2012 Realignment?
Intended and Unintended Consequences of Realignment
-
(4)
Now I’d like to focus on one of the major changes to the public mental health system in California—the 1991 Realignment when much administrative and financial responsibility was transferred from the state to the counties. What do you see as the major factors that lead to this realignment?
-
(5)
Now I’d like to ask you about the impacts of Realignment. Specifically, I wonder if you could describe what you thought Realignment would achieve when it was implemented. I’m also interested in hearing about any ways the actual results, as you see them, confirmed or were different from your expectations.
-
(a)
Was the balance of authority delegated from the State to the counties expected to change? If yes, how and why? Was this expectation fulfilled? Were there any unintended consequences?
-
(b)
Were financial responsibilities for the State and counties expected to change? If yes, how and why? Was this expectation fulfilled? Were there any unintended consequences?
-
(c)
Was redistribution from better-resourced and more under-resourced counties expected to occur? If yes, how and why? Was this expectation fulfilled? Were there any unintended consequences?
-
(d)
Was delivery of care for children, youth, and young adults expected to change? If yes, how and why? Was this expectation fulfilled? Were there any unintended consequences?
i. Were counties encouraged to provide certain types of services to children, youth, and young adults? If yes, how and why? Was this expectation fulfilled? Were there any unintended consequences?
Probes:
Community-based versus institutional?
Non-crisis versus crisis?
Outpatient versus inpatient?
Those that are Medi-Cal reimbursable versus those that are not?
ii. Were counties expected to dedicate a higher portion of expenditures to certain types of services for children, youth, and young adults? If yes, how and why? Was this expectation fulfilled? Were there any unintended consequences?
Probes:
Community-based versus institutional?
Non-crisis versus crisis?
Outpatient versus inpatient?
Those that are Medi-Cal reimbursable versus those that are not?
iii. Were counties expected to dedicate more resources to particular groups? If yes, how and why? Was this expectation fulfilled? Were there any unintended consequences?
Probes:
Children? Youth? Young adults? Adults?
Particular racial/ethnic minorities (Asian, Black, Latino, Alaska Native or Native American) and facilities providing care for those groups?
Those with serious emotional disturbance (SED) or serious mental illness (SMI)?
Medi-Cal beneficiaries versus the uninsured?
iv. Were counties expected to contract out (to non-profit or for-profit facilities) for services more or less after Realignment? If yes, how and why? Was this expectation fulfilled? Were there any unintended consequences?
-
(a)
-
(6)
Has Realignment affected particular counties differentially? If yes, what types of counties?
Probes:
Those with larger or smaller racial/ethnic minority populations?
Better-resourced versus under-resourced counties?
Those with a large versus small number of Medi-Cal enrollees and/or uninsured population?
-
(7)
What aspects of the public mental health system might be better or worse off if devolution were undone now, and some parts were re-centralized? Can you think of some functions that might be more effective or efficient with better state-level coordination?
Probes:
Provision of mental health care?
Finances?
Redistribution?
Generalizability
-
(8)
Are there any lessons that could be applied to other areas about devolution (transferring responsibility, resources, and accountability from a higher level of government to a lower level of government) from the realignment of the public mental health system?
Probes:
For the state of California and its counties?
For other states and counties?
For the relationship between the state and federal governments?
-
(9)
Is there anything unique about California in comparison to other states with respect to the realignment of the public mental health system? Is this devolution story unique because it is California, and/or because of considerations of the case of mental health?
Share Preliminary Results
-
(10)
At this point, I’d like to share some preliminary analysis of my data. Do you have any comments about these preliminary findings that relate to our discussion today?
Current Administrator In-Depth Interview Guide
Background
-
(1)
Could you start off by giving me a little background on yourself? Could you briefly describe your path to the position you have now?
-
(2)
How would you describe your mental health department compared to other county mental health departments?
Probes:
With respect to mental health services provided?
With respect to funding priorities for mental health services?
With respect to contracting services out?
-
(3)
Does your county focus on serving any particular priority populations? Which ones?
Probes:
The uninsured?
The Medi-Cal population?
Children and youth with serious emotional disturbance (SED) or young adults with serious mental illness (SMI)?
Particular racial or ethnic minorities?
Need and Demand for Mental Health Services
-
(4)
Do different racial or ethnic groups need different types of mental health services? If yes, what differences are there, and why are there differences?
Probes:
Institutional versus community-based care?
Crisis versus non-crisis care?
Inpatient versus outpatient care?
-
(5)
Are there general differences in the ways that different racial or ethnic groups use or access mental health services? If yes, what differences are there, and why are there differences?
Probes:
Institutional versus community-based care?
Crisis versus non-crisis care?
Inpatient versus outpatient care?
In different settings, such as racial/ethnic-focused organizations?
Resources to Address Need and Demand
-
(6)
Does your county address racial and ethnic disparities (or differences) in access to and use of mental health care? If yes, how does it address these disparities?
Probes:
Are there particular organizations or programs that focus on racial or ethnic minorities in your county?
-
(7)
Have any state or county policies been influential in shifting your county’s attention toward addressing racial and ethnic disparities in mental health treatment? If yes, which policies?
Probes:
1991 Realignment?
Systems of Care (1984–1998)?
EPSDT expansion/T.L. v. Belshe lawsuit (1995)?
Medi-Cal mental health services “carve out” (1995)?
County mental health plans (1995)?
Medi-Cal consolidation (1997–1998)?
Mental Health Services Act (2004)?
2011–2012 Realignment?
-
(8)
To what extent have you been able to address these racial and ethnic disparities? What are some of the key barriers?
Probes:
Other funding priorities for your counties? Which ones?
Other mental health funding priorities? Which ones?
Provider resistance?
Political resistance?
-
(9)
Does your department have the flexibility to alter its mix of mental health services in response to your priorities, to ensure optimal delivery of care, or other needs? If yes, how does it exercise this flexibility? If no, why does it not have this flexibility?
Probes:
Institutional versus community-based care?
Crisis versus non-crisis care?
Inpatient versus outpatient care?
In different settings, such as racial/ethnic-focused organizations?
-
(10)
Does your department have the policy discretion to alter the mix of mental health services provided? If yes, how does it exercise this policy discretion? If no, why does it not have policy discretion?
-
(11)
Does your department have the spending flexibility to alter the mix of mental health services provided? If yes, how does it exercise this spending flexibility? If no, why does it not have this spending flexibility?
-
(12)
Compared to many other states, California grants its counties a high degree of responsibility with respect to mental health services. In what ways would the provision of mental health services change in your agency if mental health services were more centralized?
Probes:
Mix of mental health services provided?
Amount of services contracted out to private for-profit or non-profit entities?
Expenditures for particular services?
Expenditures for the mental health system in totality?
Preliminary Results
-
(13)
My research focuses on the public mental health system and care for children, youth, and young adults since the early 1990s. I would like to share some preliminary results on California with you, and get your feedback. What are your thoughts on these preliminary findings that relate to our discussion today?
Rights and permissions
About this article
Cite this article
Vanneman, M.E., Snowden, L.R. Linking the Legislative Process to the Consequences of Realigning California’s Public Mental Health System. Adm Policy Ment Health 42, 593–605 (2015). https://doi.org/10.1007/s10488-014-0591-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10488-014-0591-z