Abstract
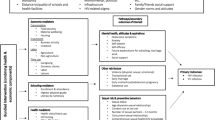
This longitudinal qualitative study sought to understand how and why a livelihood intervention affected the health and health behaviors of HIV-infected Kenyan adults. The intervention included a microfinance loan, agricultural and financial training, and a human-powered water pump. In-depth interviews were conducted at two time points with intervention and control participants and program staff. We double coded interviews (n = 117) and used thematic content analysis of transcripts following an integrative inductive–deductive approach. Intervention participants described improvements in HIV health, including increased CD4 counts and energy, improved viral suppression, and fewer HIV-related symptoms. Better health was linked to improved clinic attendance and ART adherence through several mechanisms: (1) reductions in food insecurity and abject hunger; (2) improved financial stability; (3) improved productivity which enhanced social support; (4) better control over work situations; and, (5) renewed desire to prioritize their own health. Livelihood interventions may improve health by influencing upstream determinants of health behavior including food security and poverty.
Resumen
Este estudio cualitativo longitudinal trató de comprender por qué y de qué manera una intervención sustento impactó la salud y los comportamientos de salud de adultos kenianos infectados por el VIH. La intervención incluyó un préstamo de microfinanzas, capacitación agrícola y financiero, y una bomba de agua de propulsión humana. En dos puntos se llevaron a cabo entrevistas en profundidad con participantes de la intervención y del grupo del control, y el personal del programa. Doble-codificamos las entrevistas (n = 117) y utilizamos un análisis de contenido temático para las transcripciones, según un enfoque inductivo-deductivo integrado. Participantes de la intervención describieron mejor salud del VIH, recuentos de CD4 aumentados, mayor energía, mejor supresión viral, y menos síntomas de enfermedad asociados con el VIH. Mejor salud estaba vinculada a mejor asistencia clínica y cumplimiento de la terapia antiretroviral a través de varios mecanismos: 1) la reducción de la inseguridad alimentaria y el hambre extrema; 2) mejor estabilidad financiera; 3) mejor productividad, que aumentó apoyo social; 4) mejor control sobre situaciones laborales; y, 5) deseos renovados de priorizar a su propia salud. Intervenciones sustentos pueden mejorar la salud por influir los niveles iniciales de factores determinantes a los comportamientos de salud, incluyendo la seguridad alimentaria y la pobreza.

Similar content being viewed by others
References
Radimer KL, Olson CM, Greene JC, Campbell CC, Habicht JP. Understanding hunger and developing indicators to assess it in women and children. J Nutr Educ. 1992;24(Suppl 1):36S–45S.
Weiser SD, Young SL, Cohen CR, Kushel MB, Tsai AC, Tien PC, et al. Conceptual framework for understanding the bidirectional links between food insecurity and HIV/AIDS. Am J Clin Nutr. 2011;94(suppl):1729S–39S.
Weiser SD, Yuan C, Guzman D, Frongillo EA, Riley ED, Bangsberg DR, et al. Food insecurity and HIV clinical outcomes in a longitudinal study of urban homeless and marginally housed HIV-infected individuals. AIDS. 2013;27(18):2953–8.
Nagata JM, Cohen CR, Young SL, Wamuyu C, Armes MN, Otieno BO, et al. Descriptive characteristics and health outcomes of the food by prescription nutrition supplementation program for adults living with HIV in Nyanza Province, Kenya. PLoS ONE. 2014;9(3):e91403.
Kalichman SC, Cherry C, Amaral C, White D, Kalichman MO, Pope H, et al. Health and treatment implications of food insufficiency among people living with HIV/AIDS, Atlanta, Georgia. J Urban Health. 2010;87(4):631–41.
Weiser SD, Tsai AC, Gupta R, Frongillo EA, Kawuma A, Senkungu J, et al. Food insecurity is associated with morbidity and patterns of healthcare utilization among HIV-infected individuals in a resource-poor setting. Aids. 2012;26(1):67–75.
Weiser SD, Fernandes KA, Brandson EK, Lima VD, Anema A, Bangsberg DR, et al. The association between food insecurity and mortality among HIV-infected individuals on HAART. J Acquir Immune Defic Syndr. 2009;52(3):342–9.
Singer AW, Weiser SD, McCoy SI. Does food insecurity undermine adherence to antiretroviral therapy? A systematic review. AIDS Behav. 2015;19(8):1510–26.
Weiser SD, Tuller DM, Frongillo EA, Senkungu J, Mukiibi N, Bangsberg DR. Food insecurity as a barrier to sustained antiretroviral therapy adherence in Uganda. PLoS ONE. 2010;5(4):e10340.
Mills EJ, Nachega JB, Buchan I, Orbinski J, Attaran A, Singh S, et al. Adherence to antiretroviral therapy in sub-Saharan Africa and North America: a meta-analysis. JAMA. 2006;296(6):679–90.
Martinez H, Palar K, Linnemayr S, Smith A, Derose KP, Ramirez B, et al. Tailored nutrition education and food assistance improve adherence to HIV antiretroviral therapy: evidence from Honduras. AIDS Behav. 2014;18(Suppl 5):566–77.
Cantrell RA, Sinkala M, Megazinni K, Lawson-Marriott S, Washington S, Chi BH, et al. A pilot study of food supplementation to improve adherence to antiretroviral therapy among food-insecure adults in Lusaka, Zambia. J Acquir Immune Defic Syndr. 2008;49(2):190–5.
Byron E, Gillespie S, Nangami M. Integrating nutrition security with treatment of people living with HIV: lessons from Kenya. Food Nutr Bull. 2008;29(2):87–97.
Tsai AC, Bangsberg DR, Weiser SD. Harnessing poverty alleviation to reduce the stigma of HIV in Sub-Saharan Africa. PLoS Med. 2013;10(11):e1001557.
Schwartlander B, Stover J, Hallett T, Atun R, Avila C, Gouws E, et al. Towards an improved investment approach for an effective response to HIV/AIDS. Lancet. 2011;377(9782):2031–41.
UNAIDS. UNAIDS outcome framework 2009–2011 2010 http://www.unaids.org/en/media/unaids/contentassets/dataimport/pub/basedocument/2010/jc1713_joint_action_en.pdf.
Bateganya MH, Dong M, Oguntomilade J, Suraratdecha C. The impact of social services interventions in developing countries: a review of the evidence of impact on clinical outcomes in people living with HIV. J Acquir Immune Defic Syndr. 2015;68(Suppl 3):S357–67.
Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and evaluating complex interventions: the new Medical Research Council guidance. Bmj. 2008;337:a1655.
Weiser SD, Bukusi EA, Steinfeld RL, Frongillo EA, Weke E, Dworkin SL, et al. Shamba Maisha: randomized controlled trial of an agricultural and finance intervention to improve HIV health outcomes. AIDS. 2015;29(14):1889–94.
Kenya National Bureau of Statistics and ICF Macro. Kenya Demographic and Health Survey 2008-09. Calverton: Kenya National Bureau of Statistics and ICF Macro; 2010.
Kenya National Bureau of Statistics. Food insecurity assessment in Kenya. Nairobi: Government of Kenya; 2008.
Cohen CR, Steinfeld RL, Weke E, Bukusi EA, Hatcher AM, Shiboski S, et al. Shamba Maisha: Pilot agricultural intervention for food security and HIV health outcomes in Kenya: design, methods, baseline results and process evaluation of a cluster-randomized controlled trial. SpringerPlus. 2015;4:122.
Hatcher AM, Bonell CP. High time to unpack the ‘how’ and ‘why’ of adherence interventions. AIDS. 2016;30(8):1301–4.
Creswell JW, Clark VLP. Designing and conducting mixed methods research. New Jersey: Wiley Online Library; 2007.
Patton M. Qualitative research and evaluation methods. 3rd ed. Thousand Oaks: Sage Publications; 2002.
Bernard H. Research methods in anthropology: qualitative and quantitative approaches. 4th ed. Lanham: AltaMira Press; 2006.
Miles MB, Huberman AM, Saldaña J. Qualitative data analysis: a methods sourcebook. Thousand Oaks: SAGE Publications; 2013.
Nyamathi A, Sinha S, Ganguly KK, Ramakrishna P, Suresh P, Carpenter CL. Impact of protein supplementation and care and support on body composition and CD4 count among HIV-infected women living in rural India: results from a randomized pilot clinical trial. AIDS Behav. 2013;17(6):2011–21.
Ivers LC, Chang Y, Jerome JG, Freedberg KA. Food assistance is associated with improved body mass index, food security and attendance at clinic in an HIV program in central Haiti: a prospective observational cohort study. AIDS Res Ther. 2010;7:33.
Hardon AP, Akurut D, Comoro C, Ekezie C, Irunde HF, Gerrits T, et al. Hunger, waiting time and transport costs: time to confront challenges to ART adherence in Africa. AIDS Care. 2007;19(5):658–65.
Kagee A, Remien RH, Berkman A, Hoffman S, Campos L, Swartz L. Structural barriers to ART adherence in Southern Africa: challenges and potential ways forward. Glob Public Health. 2011;6(1):83–97.
Tuller DM, Bangsberg DR, Senkungu J, Ware NC, Emenyonu N, Weiser SD. Transportation costs impede sustained adherence and access to HAART in a clinic population in southwestern Uganda: a qualitative study. AIDS Behav. 2010;14(4):778–84.
Young S, Wheeler AC, McCoy SI, Weiser SD. A review of the role of food insecurity in adherence to care and treatment among adult and pediatric populations living with HIV and AIDS. AIDS Behav. 2014;18(Suppl 5):S505–15.
Ware NC, Idoko J, Kaaya S, Biraro IA, Wyatt MA, Agbaji O, et al. Explaining adherence success in sub-Saharan Africa: an ethnographic study. PLoS Med. 2009;6(1):e11.
Tanser F, Barnighausen T, Vandormael A, Dobra A. HIV treatment cascade in migrants and mobile populations. Curr Opin HIV AIDS. 2015;10(6):430–8.
Taylor BS, Reyes E, Levine EA, Khan SZ, Garduno LS, Donastorg Y, et al. Patterns of geographic mobility predict barriers to engagement in HIV care and antiretroviral treatment adherence. AIDS Patient Care STDS. 2014;28(6):284–95.
Lima V, Fernandes K, Rachlis B, Druyts E, Montaner J, Hogg R. Migration adversely affects antiretroviral adherence in a population-based cohort of HIV/AIDS patients. Soc Sci Med. 2009;68(6):1044–9.
Johnson MO, Rose CD, Dilworth SE, Neilands TB. Advances in the conceptualization and measurement of Health Care Empowerment: development and validation of the Health Care Empowerment inventory. PLoS ONE. 2012;7(9):e45692.
Finitsis DJ, Pellowski JA, Johnson BT. Text message intervention designs to promote adherence to antiretroviral therapy (ART): a meta-analysis of randomized controlled trials. PLoS ONE. 2014;9(2):e88166.
Chaiyachati KH, Ogbuoji O, Price M, Suthar AB, Negussie EK, Barnighausen T. Interventions to improve adherence to antiretroviral therapy: a rapid systematic review. AIDS. 2014;28(Suppl 2):S187–204.
Ford N, Nachega JB, Engel ME, Mills EJ. Directly observed antiretroviral therapy: a systematic review and meta-analysis of randomised clinical trials. Lancet. 2009;374(9707):2064–71.
Ramjan R, Calmy A, Vitoria M, Mills EJ, Hill A, Cooke G, et al. Systematic review and meta-analysis: patient and programme impact of fixed-dose combination antiretroviral therapy. Trop Med Int Health. 2014;19(5):501–13.
Bangsberg DR, Mills EJ. Long-term adherence to antiretroviral therapy in resource-limited settings: a bitter pill to swallow. Antivir Ther. 2013;18(1):25–8.
Wouters E, Masquillier C, Ponnet K, le Roux Booysen F. A peer adherence support intervention to improve the antiretroviral treatment outcomes of HIV patients in South Africa: the moderating role of family dynamics. Soc Sci Med. 2014;113:145–53.
Weigers E. The role of the agricultural sector in mitigating the impact of HIV/AIDS in sub-Saharan Africa. NJAS Wagening J Life Sci. 2008;56(3):155–66.
Economic Commission for Africa. Mitigating the impact of HIV/AIDS on smallholder agriculture, food security and rural livelihoods in Southern Africa: Challenges and Action Plan. Addis Ababa: Economic Commission for Africa; 2006.
UNAIDS. Report on the global AIDS epidemic. Geneva: Joint United Nations Programme on HIV/AIDS; 2008.
WHO. Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection. Geneva: World Health Organization; 2013.
Creswell JW, Miller DL. Determining validity in qualitative inquiry. Theory into practice. 2000;39(3):124–30.
UNAIDS. 90-90-90: an ambitious treatment target to help end the AIDS epidemic. Joint United Nations Programme on HIV/AIDS: Geneva; 2014.
Acknowledgments
We gratefully acknowledge the important support of the Kenyan Medical Research Institute (KEMRI) and Family AIDS Care & Educational Services (FACES). We also thank the women and men who generously gave their time to participate in the study. We gratefully acknowledge the Director of KEMRI and the Director of KEMRI’s Centre for Microbiology for their support in conducting this research. We also thank the Kevin Kadede, Priscah Owato, Pamela Kimwele, Gina Clark, Kyle Pusateri, and Nandy Nittur for their important contributions to this research.
Funding
This study was funded by National Institute of Mental Health (grant R34MH094215). Additional funding was provided by the World Food Programme and the Burke Family foundation. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Weiser, S.D., Hatcher, A.M., Hufstedler, L.L. et al. Changes in Health and Antiretroviral Adherence Among HIV-Infected Adults in Kenya: Qualitative Longitudinal Findings from a Livelihood Intervention. AIDS Behav 21, 415–427 (2017). https://doi.org/10.1007/s10461-016-1551-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-016-1551-2